| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Review
Volume 11, Number 6, December 2020, pages 366-369
A Strict Target for Low-Density Lipoprotein Cholesterol May not Be Necessary for Secondary Prevention of Cardiovascular Disease in All Elderly Patients With Dyslipidemia
Shin-ichiro Miuraa, b, d, Yousuke Katsudab, Makoto Sugiharaa, Amane Ikec, Hiroaki Nishikawab, Akira Kawamurac
aDepartment of Cardiology, Fukuoka University Hospital and Fukuoka University School of Medicine, Fukuoka, Japan
bDepartment of Cardiology, Fukuoka University Nishijin Hospital, Fukuoka, Japan
cDepartment of Cardiovascular Diseases, Fukuoka University Chikushi Hospital, Fukuoka, Japan
dCorresponding Author: Shin-ichiro Miura, Department of Cardiology, Fukuoka University School of Medicine, 7-45-1 Nanakuma, Jonan-Ku, Fukuoka, 814-0180, Japan. Email
Manuscript submitted August 27, 2020, accepted September 2, 2020, published online November 2, 2020
Short title: LDL Cholesterol in the Elderly
doi: https://doi.org/10.14740/cr1157
- Abstract
- Introduction
- Clinical Evidence for the Prevention of Cardiovascular Events in Elderly Patients
- Residual Cardiovascular Risks
- Conclusions
- References
| Abstract | ▴Top |
According to the Japan Atherosclerosis Society Guidelines for the Prevention of Atherosclerotic Cardiovascular Diseases 2017, standard statin therapy for hyper-low-density lipoprotein cholesterol cholesterolemia in elderly patients may be effective for the secondary prevention of coronary artery disease, as in non-elderly adults. On the other hand, high-intensity statin therapy may not be recommended in all elderly cardiovascular disease patients with dyslipidemia, and particularly in elderly patients aged ≥ 85 years. In any case, tailor-made medical care with use of statin is required that matches the background of each patient.
Keywords: Low-density lipoprotein cholesterol; Coronary artery disease; Statin therapy; Elderly
| Introduction | ▴Top |
There are three University Hospitals at Fukuoka University, Fukuoka, Japan (Fukuoka University Hospital (develops advanced medical therapies for cardiovascular diseases), Fukuoka University Chikushi Hospital (develops cardiovascular medical therapies to support regional medical institutions), and Fukuoka University Nishijin Hospital (develops community-based cardiovascular medical therapies)) (Table 1). Each of these University Hospitals has a Department of Cardiology, and, overall, thousands of cardiovascular inpatients are treated every year. Most inpatients receive statin to prevent progression of cardiovascular atherosclerosis. Nonetheless, many of these patients are readmitted to the hospital. Aging is characterized by chronic inflammation that progresses atherosclerotic cardiovascular disease (CVD). Statin has anti-inflammatory effect. According to the Japan Atherosclerosis Society Guidelines for the Prevention of Atherosclerotic Cardiovascular Diseases 2017 [1], standard statin therapy for hyper-low-density lipoprotein cholesterol (LDL-C) cholesterolemia may be effective for the secondary prevention of CVD in elderly patients, as in non-elderly adults. However, it is not clear whether high-intensity statin therapy should be recommended in all elderly CVD patients. Here, we cite previous reports and discuss this issue.
 Click to view | Table 1. Summary of Three University Hospitals of Fukuoka University in Japan |
| Clinical Evidence for the Prevention of Cardiovascular Events in Elderly Patients | ▴Top |
Elderly patients are defined as aged equal to or more than 65 years. They are divided into three groups: aged 65 - 74 years, 75 - 84 years, and ≥ 85 years (Table 2). There is almost no clinical evidence regarding the prevention of cardiovascular events in elderly patients aged ≥ 85 years by high-intensity statin therapy. Only the Cardiovascular Health Study has reported risk factors associated with cardiovascular outcome [2]. This study analyzed the 5-year risk of a composite outcome including myocardial infarction, stroke, and cardiovascular death. In elderly patients aged ≥ 85 years, low-density lipoprotein cholesterol (LDL-C) was not a risk factor for cardiovascular events. Most of the participants in the study were free of CVD, and this study did not take into account statin therapy.
 Click to view | Table 2. Should High-Intensity Statin Therapy Be Recommended in Elderly CAD Patients? |
Afilalo et al reported that statin therapy reduced the incidence of all-cause mortality [3]. They sought to determine whether statins reduce all-cause mortality in elderly patients with coronary heart disease based on the results of nine trials. The mean age range was 67.6 - 75.6 years. Statin therapy reduced the incidence of all-cause mortality at 22% over 5 years. The mean change in LDL-C was from -24 to -36%. LDL-C levels reached 90 - 100 mg/dL at follow-up. These data indicated that standard statin therapy was effective. Next, is high-intensity statin therapy more effective than standard statin therapy in elderly patients with CVD?
The High-Dose Versus Low-Dose Pitavastatin in Japanese Patients with Stable Coronary Artery Disease (REAL-CAD) study was performed to determine whether high-dose versus low-dose pitavastatin reduced CVD events in patients with CAD [4]. The mean age of the subjects was 68 years. LDL-C levels in the high-dose and low-dose statin groups were 91 and 76.6 mg/dL, respectively. High-dose statin therapy reduced the primary endpoint (a composite of cardiovascular death, nonfatal myocardial infarction, nonfatal ischemic stroke, and unstable angina requiring emergency hospitalization) compared to low-dose statin therapy. Although the data indicated that high-dose statin therapy was significantly effective, the actual value was reduced by only 1%. We do not know whether high-intensity statin therapy should be recommended in all elderly CAD patients.
Another report analyzed the effects on major vascular events per 1.0 mmol/L reduction in LDL-C, in patients subdivided by age at randomization and by previous vascular disease [5]. The relative risk of major vascular events per 1.0 mmol/L reduction by statin in the high-dose statin group in patients aged > 65 to ≤ 70 years and > 70 to ≤ 75 years was 0.79 and 0.80 relative to the control or low-dose statin group, respectively. Although the relative risk in the group aged > 75 years was 0.85, the 95% confidence interval (CI) was 0.73 - 0.98. This relatively wide range of CI was because the number of subjects was small. We should not conclude that high-dose statin therapy is effective for the secondary prevention of major vascular events in patients aged < 75 years. In addition, the relative risk of vascular death per 1.0 mmol/L reduction by statin in the high-dose more intensive statin group in patients aged > 65 to ≤ 70 years and > 70 to ≤ 75 years was 0.82 and 0.87 relative to the control or low-dose less intensive statin group, respectively. The relative risk in the group aged > 75 years was 0.88, and the 95% CI was 0.69 - 1.08. We should not conclude that high-dose more intensive statin therapy is effective for the secondary prevention of vascular death in patients aged < 75 years. Therefore, high-dose statin may be effective in all patients aged 65 - 74 years, but not in all patients aged 75 - 84 years. There is no clinical evidence available on patients aged ≥ 85 years.
| Residual Cardiovascular Risks | ▴Top |
According to the relative residual CVD risks after statin treatment for primary and secondary prevention from several large-scale randomized clinical trials [6], there is still a residual CVD risk, even though we performed high-intensity statin therapy in elderly CAD patients. After statin treatment, one-third of the instances of the onset and progression of CVD were prevented, whereas two-thirds were not, in clinical trials on primary and secondary prevention.
There are three major problems regarding residual CVD risk: 1) Insufficient reduction of LDL-C levels; 2) Low levels of high-density lipoprotein cholesterol (HDL-C) together with elevated triglyceride (TG)-rich lipoproteins; 3) Insufficient control of other risk factors (e.g., high blood pressure, obesity, metabolic syndrome, and type 2 diabetes [7]). Even if we address an insufficient reduction of LDL cholesterol levels, there can still be several other problems, such as low levels of HDL-C, elevated TG and insufficient control of other risk factors.
In the FOURIER study, a proprotein convertase subtilisin/kexin type 9 inhibitor, evolocumab, greatly reduced LDL-C levels to 30 mg/dL compared to placebo at 90 mg/dL [8]. Evolocumab significantly suppressed the primary endpoint (CVD events) compared to placebo. Thus, the intensive reduction of LDL-C levels should help to prevent CVD. The actual percentage reduction was only 2%, and 12.6% of residual CVD was not prevented. The rate of residual CVD risk is still high.
As an example of residual CVD risks, we analyzed the associations between TG levels and coronary plaque components in males and females with statin therapy (Figure 1) [9] . The average age was around 70 years, and LDL-C and TG levels were 90 mg/dL and 139 mg/dL, respectively. Integrated backscatter intravascular ultrasound examination was performed for non-culprit segments. Percent lipid volume in females, but not males, was positively associated with TG levels. Factors associated with the percentage of lipid volume evaluated in females were examined by a multivariate stepwise regression analysis using various factors including LDL-C. TG, hypertension and diabetes mellitus were significantly associated with coronary percentage of lipid volume in females. In males, only diabetes mellitus was significantly associated with lipid volume. Thus, TG levels may be a more important indicator of residual risks after statin treatment in females. The adequate control of other risk factors in addition to high-intensity statin therapy should be recommended.
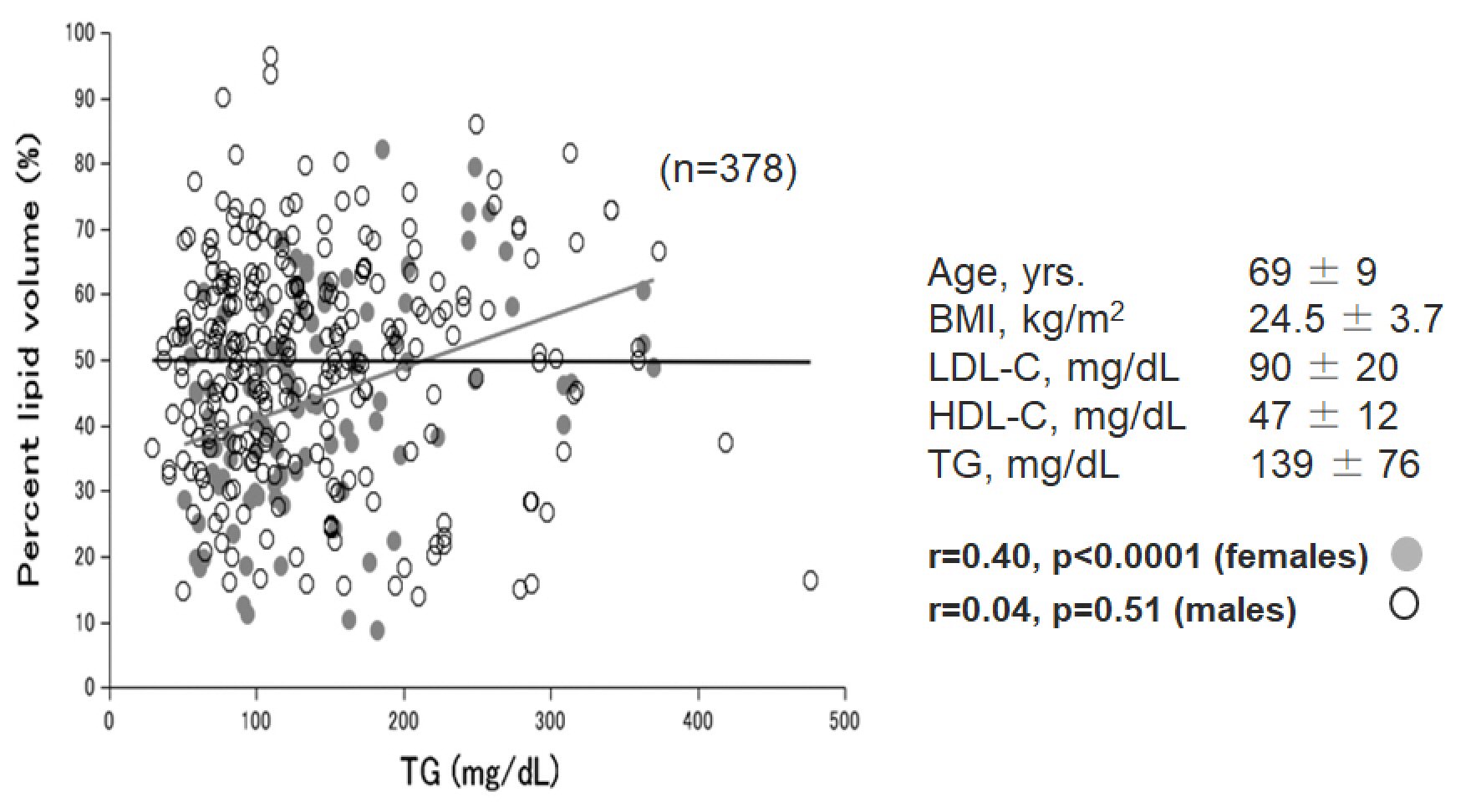 Click for large image | Figure 1. Associations between triglyceride (TG) levels and coronary plaque components in coronary artery disease patients with statin therapy. BMI: body mass index; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol. |
| Conclusions | ▴Top |
Standard statin therapy significantly prevented cardiovascular events. Although high-intensity statin therapy might be recommended in elderly CAD patients, the effect of preventing the progression of CAD by that therapy may be weak (Table 2). We should address lower HDL-C and higher TG levels in addition to the control of other risk factors to prevent cardiovascular atherosclerosis. In any case, tailor-made medical care is required that matches the background of cardiovascular risks in each patient, such as insufficient reduction of LDL-C levels, low levels of HDL-C, elevated TG, presence of high blood pressure, obesity, metabolic syndrome, and type 2 diabetes.
Acknowledgments
We thank all of the members of the Department of Cardiology, Fukuoka University Hospital, Department of Cardiovascular Diseases, Fukuoka University Chikushi Hospital, and Department of Cardiology, Fukuoka University Nishijin Hospital, Fukuoka, Japan.
Financial Disclosure
None to declare.
Conflict of Interest
SM received Trust research/joint research funds (Sumitomo Dainippon Pharma. Co., Ltd., Bayer Yakuhin Ltd., Alfresa Parma. Co.), Scholarship funds (Takeda Pharm. Co. Ltd., Daiichi Sankyo Co. Ltd., Bayer Yakuhin Ltd., Astellas Pharma Inc., Boehringer-Ingelheim, MSD K.K.) and Remuneration for lectures (Takeda Pharm. Co. Ltd., Daiichi Sankyo Co. Ltd., Bayer Yakuhin Ltd.).
Author Contributions
Conceptualization: AK, SM. Validation: SM, YK, MS, AI, HN, and AK. Investigation: YK, MS, AI, HN, and AK. Writing of original draft: AI, MS, and HN. Writing of review and editing: SM. Supervision: SM.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, Umemoto S, et al. Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2017. J Atheroscler Thromb. 2018;25(9):846-984.
doi pubmed - Odden MC, Shlipak MG, Whitson HE, Katz R, Kearney PM, defilippi C, Shastri S, et al. Risk factors for cardiovascular disease across the spectrum of older age: the Cardiovascular Health Study. Atherosclerosis. 2014;237(1):336-342.
doi pubmed - Afilalo J, Duque G, Steele R, Jukema JW, de Craen AJ, Eisenberg MJ. Statins for secondary prevention in elderly patients: a hierarchical bayesian meta-analysis. J Am Coll Cardiol. 2008;51(1):37-45.
doi pubmed - Taguchi I, Iimuro S, Iwata H, Takashima H, Abe M, Amiya E, Ogawa T, et al. High-dose versus low-dose pitavastatin in Japanese patients with stable coronary artery disease (REAL-CAD): a randomized superiority trial. Circulation. 2018;137(19):1997-2009.
doi pubmed - Cholesterol Treatment Trialists C. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407-415.
doi - Chapman MJ, Redfern JS, McGovern ME, Giral P. Niacin and fibrates in atherogenic dyslipidemia: pharmacotherapy to reduce cardiovascular risk. Pharmacol Ther. 2010;126(3):314-345.
doi pubmed - Miura S, Shiga Y, Ike A, Iwata A. Atherosclerotic coronary artery disease in patients with cardiometabolic syndrome. Cardiol Res. 2019;10(2):69-73.
doi pubmed - Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, Kuder JF, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713-1722.
doi pubmed - Yamashita M, Iwata A, Kato Y, Futami M, Imaizumi S, Kuwano T, Ike A, et al. Impact of the triglyceride level on coronary plaque components in female patients with coronary artery disease treated with statins. Heart Vessels. 2018;33(10):1175-1184.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


