| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 12, Number 1, February 2021, pages 10-15
Association Between the Level of Low-Density Lipoprotein Cholesterol and Coronary Atherosclerosis in Patients Who Have Undergone Coronary Computed Tomography Angiography
Hiroko Inouea, c, Yuhei Shigab, c, Kohei Tashirob, Yuto Kawahirab, Yasunori Suematsub, Yoshiaki Idemotob, Kanako Tanob, Takashi Kuwanob, Makoto Sugiharab, Hiroaki Nishikawaa, Yousuke Katsudaa, Shin-ichiro Miuraa, b, d
aDepartment of Cardiology, Fukuoka University Nishijin Hospital, Fukuoka, Japan
bDepartment of Cardiology, Fukuoka University School of Medicine, Fukuoka, Japan
cThese authors contributed equally to this manuscript.
dCorresponding Author: Shin-ichiro Miura, Department of Cardiology, Fukuoka University School of Medicine, 7-45-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan
Manuscript submitted October 6, 2020, accepted November 4, 2020, published online December 11, 2020
Short title: LDL Cholesterol and Coronary Atherosclerosis
doi: https://doi.org/10.14740/cr1180
| Abstract | ▴Top |
Background: Although the Japan Atherosclerosis Society Guidelines 2017 recommend lower levels of low-density lipoprotein cholesterol (LDL-C, < 70 mg/dL or ≤ 100 mg/dL) to prevent secondary cardiovascular events, we cannot conclude that a low level of LDL-C prevents primary cardiovascular events in patients with suspected coronary artery disease (CAD).
Methods: We registered 1,016 patients who were clinically suspected to have CAD and who underwent coronary computed tomography angiography (CCTA) for screening of coronary atherosclerosis. We excluded 350 patients who were receiving anti-lipidemic therapies and finally analyzed 666 patients. The patients were divided into three groups according to the LDL-C level: < 70 mg/dL (n = 25, Low LDL-C), 70 - 99 mg/dL (n = 141, Middle LDL-C), and ≥ 100 mg/dL (n = 500, High LDL-C). A ≥ 50% coronary stenosis was initially diagnosed as CAD, and the number of significantly stenosed coronary vessels (VD), Gensini score and coronary artery calcification (CAC) score were quantified.
Results: There were no significant differences in age, high-density lipoprotein cholesterol, rates of hypertension, hemoglobin A1c, blood sugar or systolic blood pressure among the Low, Middle and High LDL-C groups. On the other hand, there were significant differences in rates of males, smoking, dyslipidemia and diabetes, diastolic blood pressure and triglyceride among the groups. The prevalence of CAD values in the Low, Middle and High LDL-C groups were similar, at 52%, 47%, and 46%, respectively. In addition, there were no significant differences in the number of VD, Gensini score or CAC score among the Low LDL-C, Middle LDL-C and High LDL-C groups.
Conclusions: We showed that the level of LDL-C was not associated with the presence or severity of CAD, which indicates that we need to screen by CCTA to prevent primary coronary events even if patients without anti-lipidemic therapies show low levels of LDL-C.
Keywords: Low-density lipoprotein cholesterol; Coronary artery disease; Coronary computed tomography angiography; Gensini score
| Introduction | ▴Top |
The incidence of atherosclerotic cardiovascular disease (ASCVD) is high when low-density lipoprotein cholesterol (LDL-C) and/or triglyceride (TG) levels are high and/or when the high-density lipoprotein cholesterol (HDL-C) level is low [1-5]. According to the Japan Atherosclerosis Society Guidelines for the Prevention of Atherosclerotic Cardiovascular Diseases 2017 [6], the management target for LDL-C for primary prevention in patients with low, moderate and high coronary risk should be < 160 mg/dL, < 140 mg/dL and < 120 mg/dL, respectively. Moreover, the target LDL-C for secondary prevention in patients with a history of coronary artery disease (CAD) is < 100 mg/dL. For patients who have high-risk conditions, such as familial hypercholesterolemia, acute coronary syndrome or diabetes complicated by other high-risk conditions, the target LDL-C is < 70 mg/dL.
We have been studying the Coronary Computed Tomography Angiography (FU-CCTA) Registry at Fukuoka University in Japan and have identified coronary risk factors for the primary prevention of CAD [7-16]. In this Registry, none of the patients were diagnosed with CAD until the time of CCTA because we used CCTA to screen for CAD. When patients had significant coronary stenosis as assessed by CCTA, they were initially diagnosed with CAD.
Therefore, using the FU-CCTA Registry, we hypothesized that the target LDL-C level for primary prevention of coronary events in patients should be < 70 mg/dL or < 100 mg/dL.
| Materials and Methods | ▴Top |
Study subjects
One thousand sixteen consecutive subjects who were clinically suspected of having CAD or who had at least one cardiac risk factor (aging, gender male, hypertension (HTN), dyslipidemia (DL), diabetes mellitus (DM), smoking, obesity, family history of CAD and/or chronic kidney disease (CKD)) underwent CCTA. Suspected CAD is defined as having some chest symptoms and/or electrocardiogram (ECG) abnormalities. All subjects underwent CCTA between 2012 and 2019. Patients with creatinine > 2.0 mg/dL or contrast-induced allergy did not undergo multidetector computed tomography (MDCT). This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. The protocol in this study was approved by the ethics committee of Fukuoka University Hospital (#09-10-02), and all subjects gave their written informed consent to participate.
Evaluation of coronary stenosis using CCTA
We evaluated coronary stenosis using CCTA as previously described [7-9]. Patients were assessed by 64-MDCT on an Aquilion 64 (TOSHIBA, Tokyo, Japan) or by 320-MDCT on an Aquilion ONE ViSION (TOSHIBA, Tokyo, Japan). Overall, 15 coronary artery segments were assessed in all patients. Narrowing of the normal contrast-enhanced lumen to ≥ 50% that could be identified in multiplanar reconstructions or cross-sectional images was defined as significant stenosis [17]. The narrowing of the normal contrast-enhanced lumen to ≥ 70% was also defined as significant stenosis. When patients had significant coronary stenosis, they were initially diagnosed with CAD. In addition, in all patients, the severity of CAD was assessed in terms of the number of significantly stenosed coronary vessels (VD) and the Gensini score [18]. The coronary artery calcification (CAC) score was defined on CT images as the presence of more than two contiguous pixels with greater than 130 Hounsfield units. The CAC score in each lesion was then computed by the Agatston method [19].
Evaluation of risk factors for CAD
Body mass index (BMI), systolic blood pressure (SBP), diastolic BP (DBP), serum levels of TG, HDL-C, LDL-C, fasting blood glucose (FBG), hemoglobin A1c (HbA1c), smoking status, and medication use were collected as risk factors in all patients. BMI was calculated as weight (kg)/height (m)2. The characteristics of patients were obtained from medical records with regard to history of HTN, DL and DM.
Medications
Information on medication use was obtained from medical records and included biguanide, dipeptidyl peptidase-4 inhibitor (DPP-4I), insulin, angiotensin II receptor blocker/angiotensin-converting enzyme inhibitor (ARB/ACEI), calcium channel blocker (CCB), β-blocker and diuretics.
Statistical analysis
A statistical analysis was performed using Excel 2016 (SSRI, Tokyo, Japan) and the Stat View statistical software package (Stat View 5; SAS Institute Inc., Cary, NC, USA). Continuous variables are shown as the mean ± standard deviation. Categorical and continuous variables were analyzed for trends among the groups by the Cochran-Armitage trend test and Jonckheere-Terpstra trend test, respectively. A value of P < 0.05 was considered significant.
| Results | ▴Top |
Patient characteristics
One thousand sixteen patients were assessed for eligibility (Fig. 1). Three hundred fifty patients were excluded because they were receiving anti-lipidemic therapies. Six hundred sixty-six patients were divided into three groups: LDL-C < 70 mg/dL (n = 25, Low LDL-C group), 100 mg/dL > LDL-C ≥ 70 mg/dL (n = 141, Middle LDL-C group) and LDL-C ≥ 100 mg/dL (n = 500, High LDL-C group) (Table 1). The mean levels of LDL-C in the Low LDL-C, Middle LDL-C and High LDL-C groups were 57 mg/dL, 87 mg/dL and 133 mg/dL, respectively (P for trend < 0.001). In addition, the mean levels of TG in the Low LDL-C, Middle LDL-C and High LDL-C groups were 125 mg/dL, 132 mg/dL and 136 mg/dL, respectively (P for trend < 0.001). There were no significant differences in age, HDL-C, rate of HTN, HbA1c, FBS, SBP or medications (the rates of biguanide, DPP4-I, CCB, β-blocker and diuretics). On the other hand, there were significant differences in the rates of males, smoking, DL, DM, insulin and ARB/ACEI, and BMI and DBP.
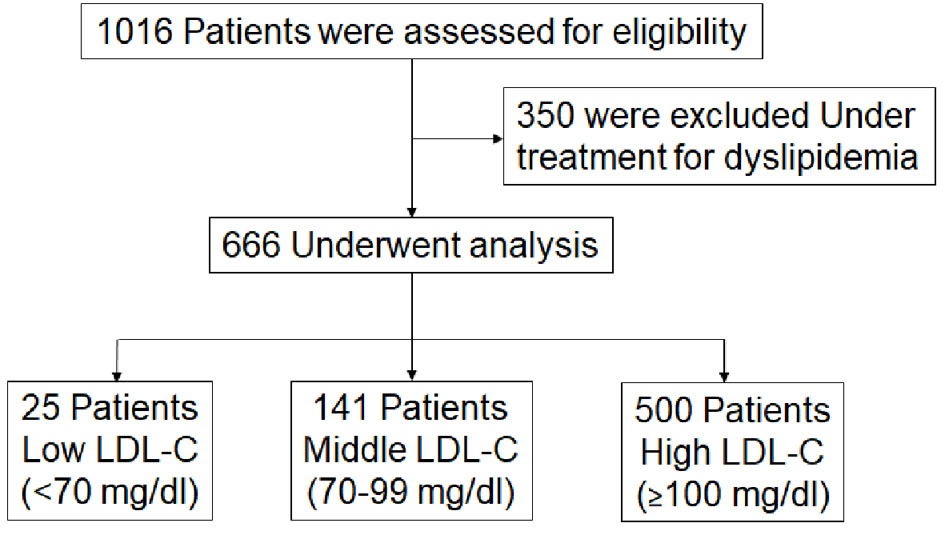 Click for large image | Figure 1. Flow chart of the enrollment process. LDL-C: low-density lipoprotein cholesterol. |
 Click to view | Table 1. Patients Characteristics in All Patients, Low LDL-C, Middle LDL-C and High LDL-C groups |
The prevalence of CAD, number of VD, Gensini score and CAC score
When ≥ 50% of coronary stenosis was defined as significant stenosis, the prevalence of CAD values in the Low LDL-C, Middle LDL-C and High LDL-C groups were similar, at 52%, 47%, and 46%, respectively (P for trend 0.3) (Fig. 2a). The number of VD in the Low LDL-C, Middle LDL-C and High LDL-C groups was 0.8, 0.9 and 0.8, respectively (P for trend 1.0) (Fig. 2b). The Gensini score and CAC score were also similar between the groups (Fig. 2c, d). In addition, when ≥ 70% of coronary stenosis was defined as significant stenosis, there were also no differences in %CAD and the number of VD among Low, Middle and High LDL-C groups (Fig. 2e, f).
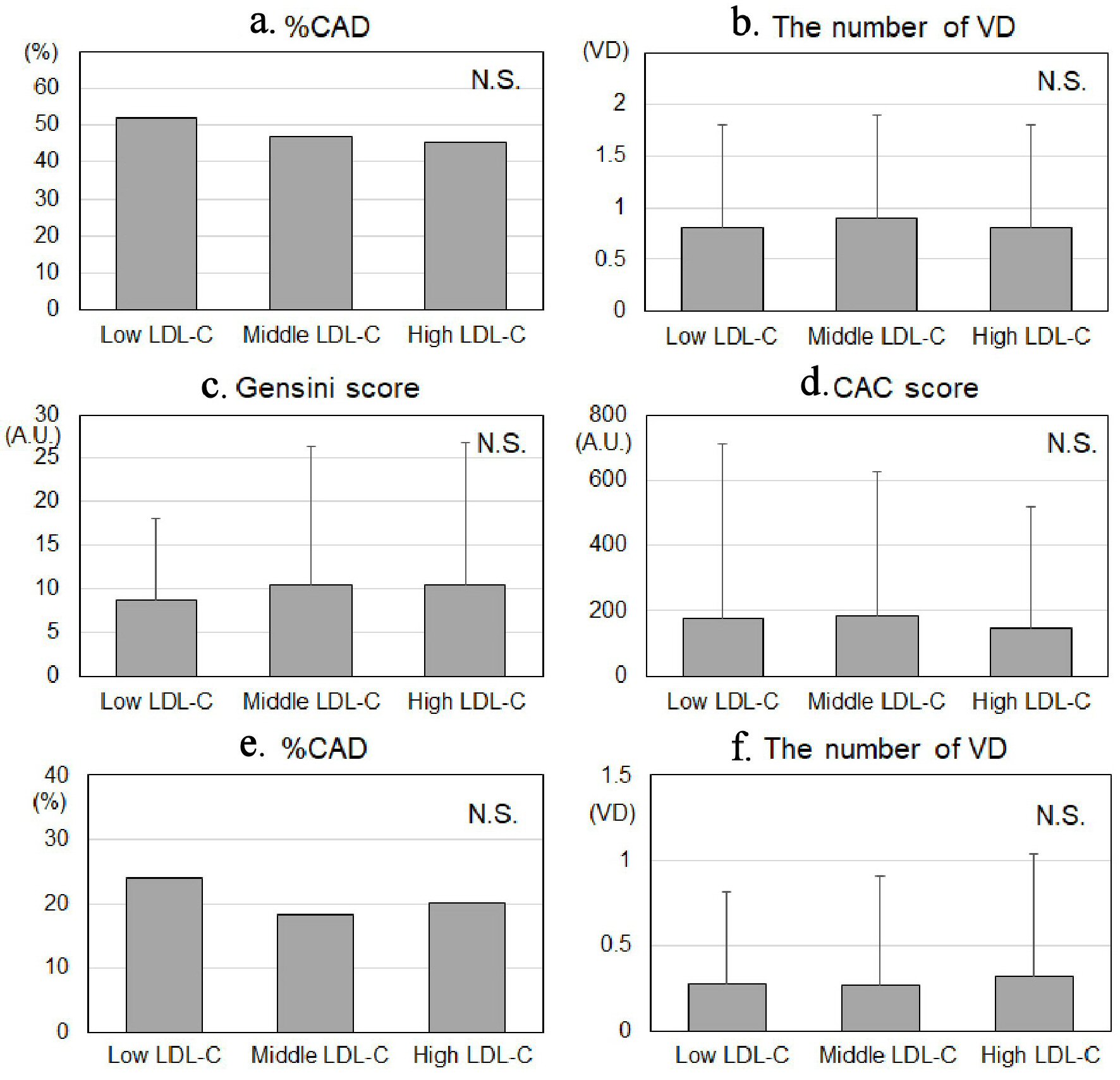 Click for large image | Figure 2. The prevalence of CAD (a, e), number of VD (b, f), Gensini score (c) and CAC score (d) in the Low LDL-C, Middle LDL-C and High LDL-C groups. The ≥ 50% and ≥ 70% of coronary stenosis were defined as significant stenosis in (a, b) and (e, f), respectively. CAD: coronary artery disease; number of VD: number of significantly stenosed coronary vessels; CACS: coronary artery calcium score; LDL-C: low-density lipoprotein cholesterol; N.S.: not significant; A.U.: arbitrary unit. |
| Discussion | ▴Top |
In this study, we hypothesized that the target LDL-C level in patients for the primary prevention of CAD events should be < 70 mg/dL or < 100 mg/dL. We showed that LDL-C < 70 mg/dL or < 100 mg/dL under no anti-lipidemic therapies was not associated with the presence or severity of CAD. These results indicated that we need to screen with CCTA to prevent primary events regardless of LDL-C levels.
The most important finding in this study was that LDL-C < 70 mg/dL or < 100 mg/dL was not associated with lower the prevalence of CAD or a reduced severity of CAD, since there were no significant differences in the prevalence of CAD, number of VD, Gensini score or CAC score among the Low LDL-C, Middle LDL-C and High LDL-C groups. In a word, patients with lower LDL-C levels do not have a lower risk of CAD compared to patients with higher LDL-C (≥ 100 mg/dL). The High LDL-C group had lower rates of males, smoking and HTN compared to the Low and Middle LDL-C groups. Male, smoking and HTN are critical coronary risk factors [20]. Although there were no significant differences in HbA1c between the groups, the rate of insulin use in the High LDL-C group was lower than those in the Low and Middle LDL-C groups. The data indicated that the severity of DM in the High LDL-C group may be lower than those in the Low and Middle LDL-C groups. Although LDL-C levels in the High LDL-C group were relatively high (≥ 100 mg/dL), the rates of other risk factors were relatively low. Therefore, there were no significant differences in the presence or severity of CAD among the groups. In this study, patients who were clinically suspected of having CAD or who had at least one cardiac risk factor underwent CCTA. Thus, even though patients may show low LDL-C levels under no treatment of DL, it may be advisable to aggressively perform CCTA when patients are clinically suspected of having CAD or coronary risk factors other than DL.
This study has several important limitations. First, this study was cross-sectional. Second, CCTA is not a gold standard for the evaluation of CAD, although recent studies have shown that its sensitivity and specificity were both approximately 95% of those for invasive coronary angiography for the identification of significant coronary stenosis [21]. A large-scale prospective study will be needed to address these issues.
In conclusion, the LDL-C level was not associated with atherosclerotic CAD, which indicates that we need to perform CCTA for screening to prevent primary cardiovascular events even if patients without anti-lipidemic therapies show low levels of LDL-C.
Acknowledgments
We thank all of the members of the Department of Cardiology, Fukuoka University Hospital, and Department of Cardiology, Fukuoka University Nishijin Hospital, Fukuoka, Japan.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consents were obtained.
Author Contributions
Conceptualization: Y. Katsuda and S.M. Validation: H.I., K.T., Y. Kawahira, and Y.I. Formal analysis: Y.S. and T.K. Investigation: M.S., H.N., and Y. Kawahira. Data curation: H.I., K.T., and Y.S. Writing-original draft: H.I., T.K., Y.S., and M.S. Writing-review and editing: S.M. Supervision: S.M.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, Toyota T, Nakaya N, et al. Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet. 2006;368(9542):1155-1163.
doi - Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr., Kastelein JJ, Koenig W, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195-2207.
doi pubmed - LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC, Gotto AM, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352(14):1425-1435.
doi pubmed - Pedersen TR, Faergeman O, Kastelein JJ, Olsson AG, Tikkanen MJ, Holme I, Larsen ML, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005;294(19):2437-2445.
doi pubmed - Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, Joyal SV, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350(15):1495-1504.
doi pubmed - Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, Umemoto S, et al. Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. J Atheroscler Thromb. 2018;25(9):846-984.
doi pubmed - Mitsutake R, Miura S, Kawamura A, Saku K. Are metabolic factors associated with coronary artery stenosis on MDCT? Circ J. 2009;73(1):132-138.
doi pubmed - Mitsutake R, Miura S, Zhang B, Saku K. HDL-associated factors provide additional prognostic information for coronary artery disease as determined by multi-detector row computed tomography. Int J Cardiol. 2010;143(1):72-78.
doi pubmed - Mitsutake R, Miura S, Shiga Y, Uehara Y, Saku K. Association between hypertension and coronary artery disease as assessed by coronary computed tomography. J Clin Hypertens (Greenwich). 2011;13(3):198-204.
doi pubmed - Shiga Y, Miura S, Mitsutake R, Kawamura A, Uehara Y, Saku K. Significance of serum high-density lipoprotein cholesterol levels for diagnosis of coronary stenosis as determined by MDCT in patients with suspected coronary artery disease. J Atheroscler Thromb. 2010;17(8):870-878.
doi pubmed - Nakamura A, Miura S, Sugihara M, Miyase Y, Norimatsu K, Shiga Y, Nishikawa H, et al. Contrast between innovator drug- and generic drug-induced renal dysfunction on coronary angiography (CONTRAST study). Heart Vessels. 2014;29(5):603-610.
doi pubmed - Norimatsu K, Miura S, Suematsu Y, Shiga Y, Miyase Y, Nakamura A, Yamada M, et al. Associations between glycated albumin or hemoglobin A1c and the presence of coronary artery disease. J Cardiol. 2015;65(6):487-493.
doi pubmed - Yano M, Miura S, Shiga Y, Miyase Y, Suematsu Y, Norimatsu K, Nakamura A, et al. Association between smoking habits and severity of coronary stenosis as assessed by coronary computed tomography angiography. Heart Vessels. 2016;31(7):1061-1068.
doi pubmed - Norimatsu K, Kuwano T, Miura SI, Shimizu T, Shiga Y, Suematsu Y, Miyase Y, et al. Significance of the percentage of cholesterol efflux capacity and total cholesterol efflux capacity in patients with or without coronary artery disease. Heart Vessels. 2017;32(1):30-38.
doi pubmed - Ueda Y, Shiga Y, Idemoto Y, Tashiro K, Motozato K, Koyoshi R, Kuwano T, et al. Association between the presence or severity of coronary artery disease and pericardial fat, paracardial fat, epicardial fat, visceral fat, and subcutaneous fat as assessed by multi-detector row computed tomography. Int Heart J. 2018;59(4):695-704.
doi pubmed - Nose D, Shiga Y, Ueda Y, Idemoto Y, Tashiro K, Suematsu Y, Kuwano T, et al. Association between plasma levels of PCSK9 and the presence of coronary artery disease in Japanese. Heart Vessels. 2019;34(1):19-28.
doi pubmed - Leipsic J, Abbara S, Achenbach S, Cury R, Earls JP, Mancini GJ, Nieman K, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2014;8(5):342-358.
doi pubmed - Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51(3):606.
doi - Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827-832.
doi - Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42(9):1235-1481.
doi pubmed - Ropers D, Rixe J, Anders K, Kuttner A, Baum U, Bautz W, Daniel WG, et al. Usefulness of multidetector row spiral computed tomography with 64- x 0.6-mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenoses. Am J Cardiol. 2006;97(3):343-348.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


