| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 15, Number 4, August 2024, pages 246-252
The Predictive Role of Cardiac Troponin Elevation Ratio Combined With Heart Function Index Model in the Prognosis of Non-ST-Segment Elevation Myocardial Infarction Patients
Xian Jun Hua, b, Xiao Guang Suna, b, Jia Yuan Chenga, Jie Maa, c
aDepartment of Cardiovascular Medicine, Chaohu Hospital of Anhui Medical University, Chaohu, China
bThese authors contributed equally to this work.
cCorresponding Author: Jie Ma, Department of Cardiovascular Medicine, Chaohu Hospital of Anhui Medical University, Chaohu City, Anhui Province 823000, China
Manuscript submitted March 19, 2024, accepted June 7, 2024, published online July 18, 2024
Short title: Predictive Role of cTnI/ULN in NSTEMI
doi: https://doi.org/10.14740/cr1639
| Abstract | ▴Top |
Background: Non-ST-segment elevation myocardial infarction (NSTEMI) is a common form of coronary artery disease, and its prognosis is influenced by multiple factors. This study aimed to analyze the predictive role of the combined application of cardiac troponin and cardiac function indices in NSTEMI patients’ prognosis.
Methods: NSTEMI patients were screened and included in the study. Cardiac troponin elevation ratio (cardiac troponin I (cTnI)/upper limit of normal (ULN)) was measured upon admission, and cardiac function was assessed. General clinical data, laboratory parameters, Grace score, New York Heart Association (NYHA) functional class, complications, and mortality data were collected. The correlation between mortality in NSTEMI patients and clinical parameters was analyzed, and a nomogram prediction model for NSTEMI patient mortality was established.
Results: A total of 252 NSTEMI patients were included. Female gender, elevated high-sensitivity C-reactive protein (H-CRP), left ventricular ejection fraction (LVEF) < 50%, NYHA class III and IV, and cTnI/ULN elevation by 36.25-fold were significantly independently associated with mortality outcomes. Multifactorial logistic analysis indicated that these indices remained associated with mortality. A nomogram model predicting NSTEMI patient mortality was constructed using these indices, with an area under the curve (AUC) of 0.911, sensitivity of 97.5%, and specificity of 72.8%. This predictive model outperformed the Grace score (AUC = 0.840).
Conclusions: In NSTEMI patients, a 36.25-fold increase in cTnI/ULN, coupled with NYHA class III and IV, independently predicted prognosis. We developed a nomogram model integrating cTnI/ULN and cardiac function indices, aiding clinicians in assessing risk and implementing early interventions for improved outcomes.
Keywords: NSTEMI; Cardiac troponin; Cardiac function; Nomogram model
| Introduction | ▴Top |
Cardiovascular disease remains a leading cause of global mortality [1, 2]. Over the past 30 years, the incidence of acute coronary syndromes (ACS) has significantly increased in China [2, 3]. Non-ST-segment elevation myocardial infarction (NSTEMI) represents a major component of ACS, with an incidence exceeding that of ST-segment elevation myocardial infarction (STEMI) by more than two-fold [4]. However, risk stratification for patients with chest pain who do not exhibit ST-segment elevation or pathological Q-waves has remained challenging. This issue not only impacts clinical decision-making but also involves choices regarding medical and interventional interventions and the determination of conservative or invasive treatment strategies. Moreover, there exists substantial heterogeneity in clinical outcomes among NSTEMI patients, underscoring the critical need for risk assessment to guide timely treatment decisions [5]. Current guidelines recommend risk stratification of high-risk patients upon admission to facilitate more aggressive invasive treatment in high-risk populations [6]. Therefore, there is a need for a simple and accurate method to assess individual risk.
The Grace score is a commonly used ACS prediction model that can predict all-cause mortality in NSTEMI patients. However, its predictive accuracy is limited [7], and its predictive utility for major adverse cardiovascular events in certain subtypes of NSTEMI patients is suboptimal [8]. There is still a lack of an ideal tool that is both convenient and accurate for predicting the prognosis of NSTEMI patients.
Cardiac troponin is a protein closely associated with myocardial injury [9] and is widely used in the diagnosis of myocardial infarction. Elevated cardiac troponin is an early marker of myocardial injury and is associated with adverse outcomes in NSTEMI patients, including a higher incidence of congestive heart failure, shock, and death. Additionally, persistently elevated cardiac troponin levels (approximately greater than five times the normal value) following percutaneous coronary intervention (PCI) are associated with adverse long-term outcomes [10]. However, given the variability in results due to differences in study populations, cut-off values, and timing of measurements across various studies, further investigation into the predictive role of elevated cardiac troponin in the prognosis of NSTEMI patients is warranted [11, 12]. Furthermore, considering that combined markers may enhance predictive value [13], studies have explored this aspect but have not yet yielded significant predictive results [14, 15]. New York Heart Association (NYHA) functional classification is a common clinical method for assessing impaired heart function.
Objectives
In this study, we aimed to explore prognostic factors in a Chinese cohort of NSTEMI patients, investigate the predictive role of the cardiac troponin elevation ratio combined with cardiac function for short-term adverse outcomes in NSTEMI patients, and compare the predictive abilities of the Grace score and the new prognostic factors in patient prognosis risk scoring.
| Materials and Methods | ▴Top |
Clinical data
The study retrospectively collected data from NSTEMI patients treated at Chaohu Hospital of Anhui Medical University between January 2021 and December 2022. Inclusion criteria were as follows: 1) Typical chest pain symptoms; 2) Presence of an electrocardiogram (ECG) showing no ST-segment elevation, possibly accompanied by ST-segment depression or T-wave inversion; 3) Laboratory markers indicating myocardial injury, such as elevated cardiac troponin or creatine kinase-MB (CKMB). Exclusion criteria were: 1) Atypical chest pain symptoms; 2) Lack of ECG results or ECG showing ST-segment elevation; 3) Absence of laboratory markers indicating myocardial injury, such as elevated cardiac troponin or CKMB.
This study was reviewed and approved by the Ethics Committee of Chaohu Hospital of Anhui Medical University and was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Sample volume
Based on the situation at a single center, the study plans to include patients who underwent PCI treatment within a 2-year period as the study sample. According to statistical data, the number of PCI-treated cases in our hospital ranges from approximately 450 to 500 per year, with NSTEMI patients accounting for approximately 20-30% of the total sample. Therefore, this study planned to include at least 200 NSTEMI patients as study subjects to ensure an adequate and representative sample size.
Treatments
All patients with ACS received a loading dose of dual antiplatelet therapy (DAPT) within 10 min of diagnosis prior to enrollment (except those with contraindications), with approximately 60% of ACS patients receiving anticoagulant therapy within 10 min of diagnosis. PCI preparation was conducted for all patients upon enrollment as NSTEMI patients.
Prior to treatment, patients orally ingest 300 mg enteric-coated aspirin tablets (manufactured by Bayer Group, national drug approval number D98765432, specification: 100 mg/tablet.), and 300 mg clopidogrel hydrogen sulfate tablets (manufactured by AstraZeneca, national drug approval number T180MG0923, specification: 180 mg/tablet), and undergo iodine allergy testing.
Patients meeting PCI treatment criteria undergo iodine disinfection in the right arm and bilateral groin regions, local anesthesia is administered, and upon successful anesthesia, radial artery puncture is performed. The sheath is advanced along the guidewire into the radial artery, blood is aspirated from the sheath to prevent air bubbles from entering the vessel, and the sheath is sealed with heparin saline solution. The catheter is advanced along the guidewire for coronary angiography. Before angiography, 3,000 U of heparin is administered. The nature and characteristics of the lesion are clarified by coronary angiography. Guiding catheters are selected based on the characteristics of the aortic root. After placing the guiding catheter, additional heparin is administered at 100 U/kg to advance the guidewire to the distal vessel. The appropriate balloon is selected based on the vessel diameter, and precise positioning of the balloon is performed to dilate the target vessel lesion. If vessel stenosis is ≥ 70%, the corresponding drug-eluting stent is implanted. Coronary angiography is performed again to observe vessel patency, ensuring good interventional treatment outcomes, and completing the interventional treatment.
For NSTEMI patients who do not meet the criteria for PCI treatment (anatomical limitations, medical contraindications, patient preference), treatment involves the use of antiplatelet agents (aspirin), anticoagulants (low molecular weight heparin), and anti-anginal medications (nitrates, beta-blockers) based on the patient’s specific condition and severity of the illness.
Data collection for enrolled patients
Data were collected including: 1) General information: name, gender, and age. 2) Laboratory parameters upon admission (measurement of cardiac troponin I (cTnI), cardiac troponin T, CKMB, N-terminal pro-B-type natriuretic peptide (NT-proBNP), left ventricular ejection fraction (LVEF), creatinine, low-density lipoprotein, homocysteine, high-sensitivity C-reactive protein, uric acid, and cardiac troponin elevation ratio (cTnI/upper limit of normal (ULN) (cTnI/ULN is the ratio of cTnI concentration to the ULN, typically used to assess myocardial injury. The formula for calculation is: cTnI/ULN = cTnI/ULN). The initial cardiac troponin sampling was conducted within 3 - 6 h following the onset of chest pain upon admission. A second sampling was performed within 6 h after the initial collection. Afterwards, monitoring is conducted every 12 h. 3) Scoring: a) Grace score (The Grace score consists of eight independent factors including age, heart rate, blood pressure, renal function, cardiac biomarkers, electrocardiographic findings (ST-segment deviation), signs of impending myocardial infarction, and signs of heart failure. Each factor is assigned a different score, and the total score ranges from 0 to multiple, with higher scores indicating higher risk.). b) Functional class (It is typically assessed using the NYHA functional classification system, which categorizes patients into one of four classes (I, II, III, IV) based on the degree of limitation of physical activity and severity of symptoms experienced during daily activities.). c) Gensisi score (The Gensini score calculates based on the location and severity of coronary artery stenosis, with a focus on the severity and number of major vessel lesions. Scoring is based on the location (major, minor, or branch) and severity of coronary artery lesions, with different scores assigned for different lesion locations and severity levels. The total score is used to assess the severity of the condition.). 4) Comorbidities: hypertension, diabetes, hyperlipidemia. 5) Outcome information: hospitalization duration, hospitalization expenses, mortality, and other complications during hospitalization.
Statistical analysis
The study employed rigorous statistical analyses to investigate the relationship between mortality status and clinical characteristics. Initial analyses utilized Spearman’s Chi-squared test, Mann-Whitney U test, and t-test to explore associations. Subsequently, logistic regression models were applied to further assess these associations, providing estimates of odds ratios (ORs) and their corresponding 95% confidence intervals (CIs). Two-tailed tests of significance were conducted, with a threshold of P < 0.05 denoting statistical significance. All statistical procedures were conducted using SPSS 22.0 software (IBM Corp., Armonk, NY, USA). Logistic regression was specifically utilized to identify clinical characteristics predictive of mortality. Variables demonstrating significant associations with mortality were then chosen to construct a nomogram aimed at predicting MLH1 promoter methylation. The nomogram was developed utilizing the rms package (version 5.1-4) within R statistical software (version 3.4.3). Performance assessment of the nomogram was conducted using the C-index. This comprehensive analytical approach ensured robust investigation and prediction capabilities within the study’s framework.
| Results | ▴Top |
Ultimately, a total of 251 NSTEMI patients were included in the study, and baseline clinical data for patients are presented in Table 1. At the beginning of the study, we conducted a detailed analysis of baseline characteristics of the enrolled NSTEMI patients, including demographic information such as age, gender, body mass index (BMI), as well as medical history, Grace score, cardiac troponin elevation ratio, cardiac function assessment, and treatment strategies following diagnostic assessment. The average follow-up time was 2 years, with 11 cases of mortality.
 Click to view | Table 1. Demographic and Clinical Characteristics of the Study Population |
The study found a significant correlation between the cardiac troponin elevation ratio and the outcome of mortality. The optimal cut-off value determined from the receiver operating characteristic (ROC) curve was 36.25-fold, with an area under the curve (AUC) of 0.707, sensitivity of 90.9%, specificity of 47.5%, and a 95% CI of 0.571 - 0.842, with a P value of 0.021 (Fig. 1). Logistic regression analysis was conducted to assess the association between mortality outcome and clinical, pathological features, and the results are summarized as follows.
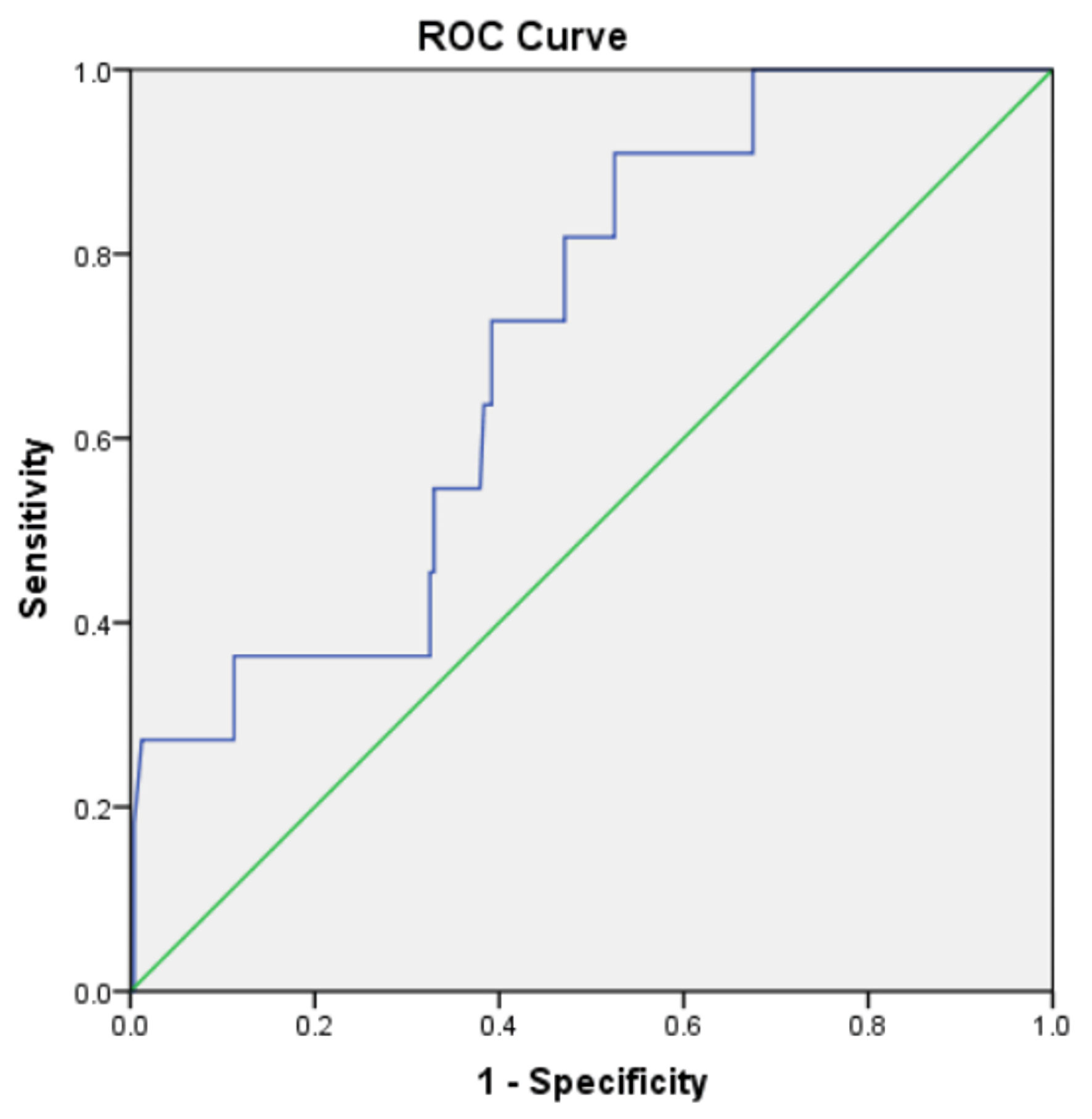 Click for large image | Figure 1. The correlation between the rate of elevation of cardiac troponin and the mortality rate. Optimal cut-off value = 36.25-fold; AUC = 0.707, sensitivity = 90.9%, specificity = 47.5%. AUC: area under the curve; ROC: receiver operating characteristic. |
Univariate logistic regression analysis revealed that age, female gender, elevated high-sensitivity C-reactive protein (H-CRP), LVEF < 50%, NYHA class III and IV, and a 36.25-fold elevation in cTnI/ULN were independent influencing factors for mortality outcome (all variables with P < 0.05). These variables were included in multivariate analysis, which showed that all the aforementioned associations remained significant, with an exceptionally high OR of 14.36 (95% CI: 2.57 - 80.177, P = 0.002) for NYHA class III and IV and an OR of 5.219 (95% CI: 12.54 - 50.27, P = 0.038) for a 36.25-fold elevation in cTnI/ULN.
Subsequently, these five significant variables were incorporated into the construction of the prediction model (Fig. 2a) and were subjected to model calibration (Fig. 2b). The AUC for the prediction model was 91.1% (95% CI: 0.890 - 0.931) (Fig. 2c). The prediction model exhibited sensitivity and specificity for predicting mortality outcome at 72.8% and 95.1%, respectively. It significantly outperformed the Grace score in predictive performance, with an AUC of 0.840 (95% CI: 0.728 - 0.953, P < 0.001) (Fig. 3).
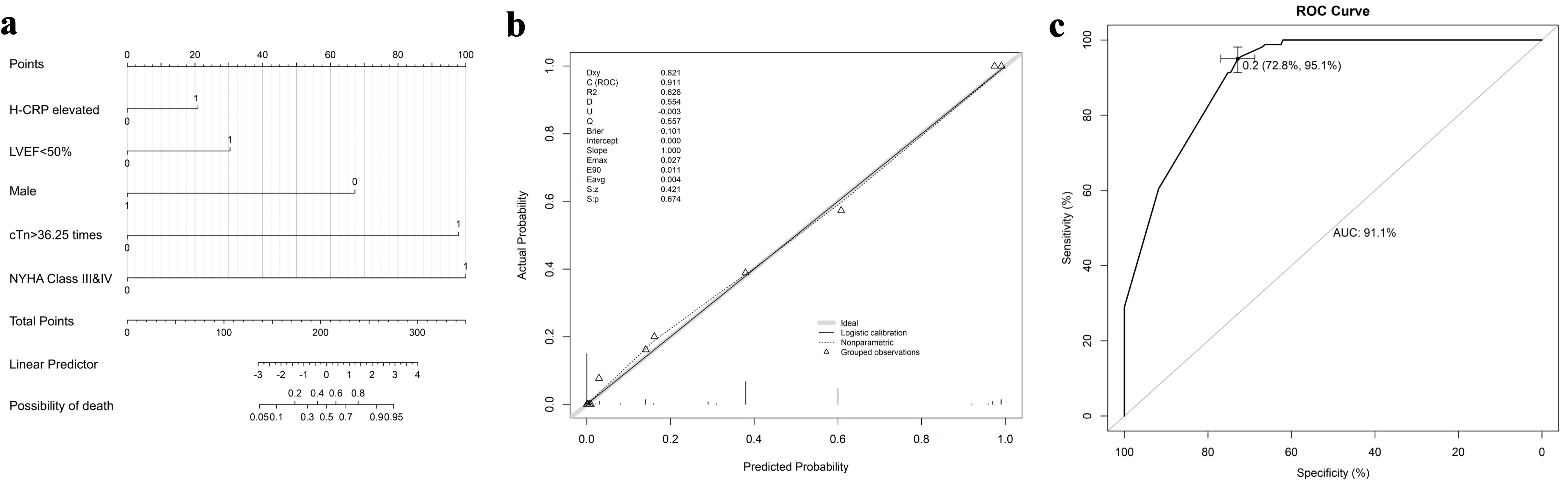 Click for large image | Figure 2. Nomogram and calibration curves for predicting the probability of death in NSTEMI patients. (a) Nomogram for prediction with the following variables: H-CRP elevated = 1; sex: 1 = male; LVEF < 50% = 1; cTnI/ULN > 36.25 times = 1; NYHA class III and IV = 1. (b) Calibrate curve of the nomogram. The C-index of this nomogram is 0.911. (c) The receiver operating characteristic (ROC) curve of the nomogram with an AUC of 0.911. The sensitivity and specificity were 72.8% and 95.1%, respectively. NYHA: New York Heart Association; LVEF: left ventricular ejection fraction; cTnI: cardiac troponin I; ULN: upper limit of normal; AUC: area under the curve. |
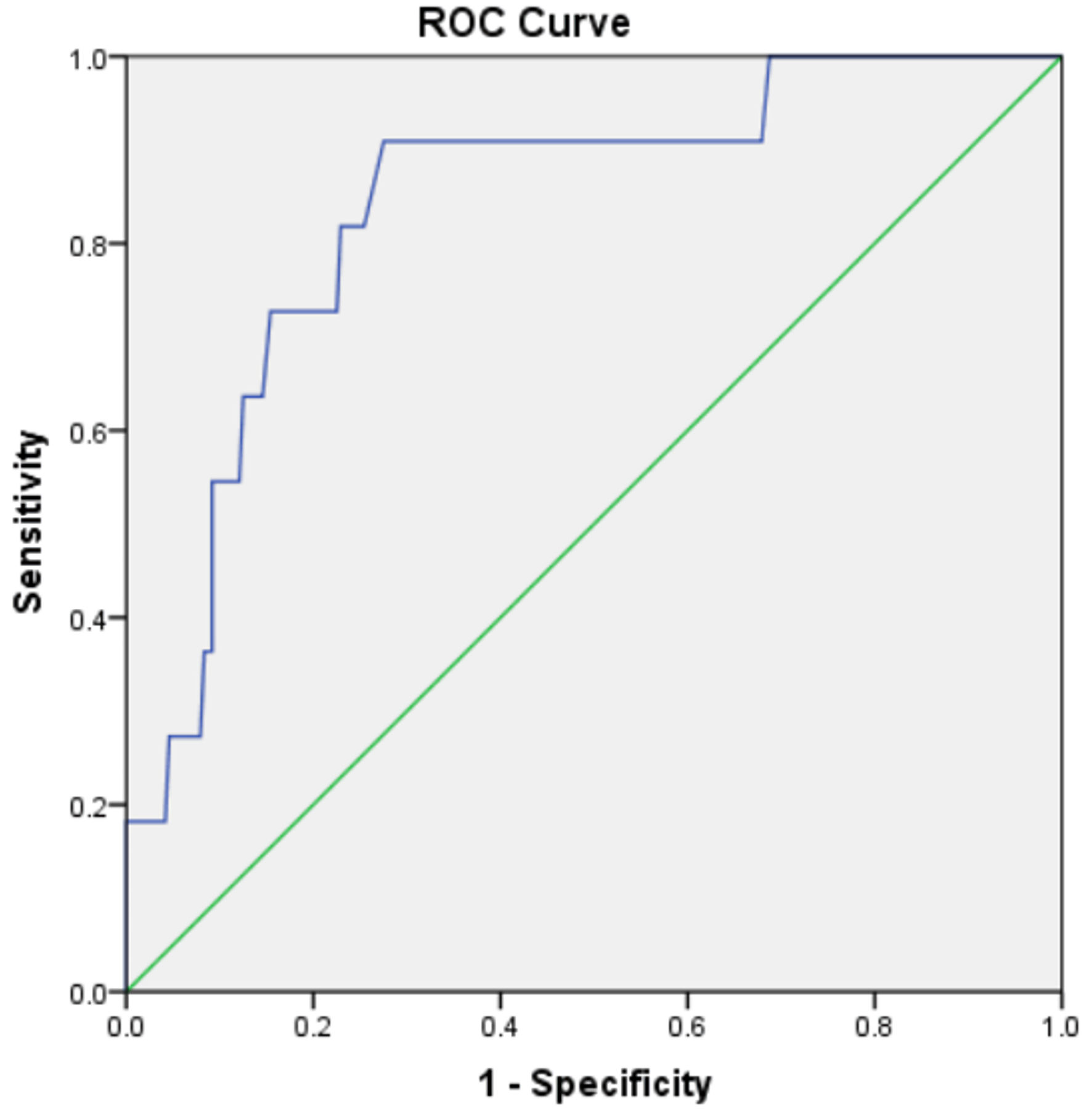 Click for large image | Figure 3. The predictive efficacy of the Grace score. AUC = 0.840, 95% CI: 0.728 - 0.953, P < 0.001. AUC: area under the curve; CI: confidence interval. |
In addition to the primary outcome, we also conducted an analysis of secondary outcomes. It was observed that patients with NYHA class III and IV and cTnI/ULN > 36.25 times had a significantly increased demand for cardiac intervention treatment, which in turn led to a significant increase in treatment costs (all P = 0.001).
| Discussion | ▴Top |
This study aimed to explore the potential role of cardiac troponin elevation ratio (cTnI/ULN) in conjunction with cardiac function indices in predicting the prognosis of NSTEMI patients. The study results revealed associations between cardiac function indices, cTnI/ULN, and outcomes in NSTEMI patients, providing important insights for clinical management and prognosis assessment.
Firstly, we observed a significant correlation between cTnI/ULN and the outcome of mortality in NSTEMI patients. Through ROC curve analysis, we determined the optimal cut-off value for cTnI/ULN elevation to be 36.25-fold, which exhibited high sensitivity and reasonable specificity. This suggests that cTnI/ULN has predictive value in assessing the risk of death in NSTEMI patients. Furthermore, multivariate logistic regression analysis confirmed that age, gender, elevated H-CRP, LVEF < 50%, NYHA class III and IV, and a 36.25-fold elevation in cTnI/ULN were independent factors influencing the mortality outcome of NSTEMI patients. These results are in line with a study by Antman et al, which identified independent prognostic factors for NSTEMI patients [16].
We further constructed a prediction model that integrated these five significant factors to predict the risk of death in NSTEMI patients. The model exhibited high accuracy, sensitivity, and specificity after calibration. The AUC was 91.1%, indicating significant predictive performance in assessing patient mortality risk. Compared to the traditional Grace score [17], this model demonstrated superior predictive efficacy, further highlighting its potential applicability in NSTEMI patients.
Additionally, beyond the primary mortality outcome, we observed that patients with NYHA class III and IV and cTnI/ULN > 36.25-fold were more likely to require cardiac intervention treatment, leading to a significant increase in treatment costs. This underscores the importance of timely identification of high-risk patients to facilitate appropriate treatment measures and optimize resource allocation.
Despite providing valuable insights into prognosis prediction for NSTEMI patients, this study has certain limitations. Firstly, it is a single-center retrospective study, which may introduce selection bias and information bias. Secondly, the sample size is relatively small, and larger-scale studies are needed to validate these findings. Thirdly, our study focused on the mortality outcome of NSTEMI patients, and future research can further explore the relevance of other clinical outcomes and interventions. Lastly, the model in this study serves as a supplement and enhancement to the Grace score. It does not differentiate by race; therefore, theoretically, it predicts based solely on the definition and presentation of the disease, without considering race. However, there are genetic, lifestyle, and environmental differences among different populations, which may affect the occurrence of cardiovascular events and the applicability of predictive models. Therefore, this represents an area for future research, which will involve multicenter validation to address this issue.
Conclusions
This study emphasizes the potential role of cTnI/ULN in conjunction with cardiac function indices in predicting the prognosis of NSTEMI patients. It also establishes a prediction model that can be used to more accurately assess patients’ risk of mortality. This model may assist clinical practitioners in better identifying high-risk patients and taking timely intervention measures to improve patient outcomes. Further research is needed to validate these findings and expand the scope of prognosis assessment in NSTEMI patients.
Acknowledgments
None to declare.
Financial Disclosure
This work was supported by the Anhui Medical University School Fund (2022xkj209 to the Xian Jun Hu). The funder did not influence study design, data collection, and analysis, the decision to publish, or the manuscript preparation.
Conflict of Interest
All the authors have no conflict of interest.
Informed Consent
This study is a retrospective study and waiver informed consent has been obtained
Author Contributions
XJH and XGS: conceptualization, methodology, funding acquisition, writing - original draft, investigation, data curation, and formal analysis. JYC: investigation, data curation, software, and validation. JM: conceptualization, supervision, writing - review, and editing. All authors contributed to the article and approved the submitted version.
Data Availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
| References | ▴Top |
- Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56-e528.
doi pubmed - Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, Liu Y, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 global burden of disease study. JAMA Cardiol. 2019;4(4):342-352.
doi pubmed pmc - Du X, Patel A, Anderson CS, Dong J, Ma C. Epidemiology of cardiovascular disease in china and opportunities for improvement: JACC International. J Am Coll Cardiol. 2019;73(24):3135-3147.
doi pubmed - Puelacher C, Gugala M, Adamson PD, Shah A, Chapman AR, Anand A, Sabti Z, et al. Incidence and outcomes of unstable angina compared with non-ST-elevation myocardial infarction. Heart. 2019;105(18):1423-1431.
doi pubmed - Puymirat E, Simon T, Cayla G, Cottin Y, Elbaz M, Coste P, Lemesle G, et al. Acute myocardial infarction: changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation. 2017;136(20):1908-1919.
doi pubmed - Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267-315.
doi pubmed - Gong IY, Goodman SG, Brieger D, Gale CP, Chew DP, Welsh RC, Huynh T, et al. GRACE risk score: Sex-based validity of in-hospital mortality prediction in Canadian patients with acute coronary syndrome. Int J Cardiol. 2017;244:24-29.
doi pubmed - Chen X, Wu H, Li L, Zhao X, Zhang C, Wang WE. The prognostic utility of GRACE risk score in predictive adverse cardiovascular outcomes in patients with NSTEMI and multivessel disease. BMC Cardiovasc Disord. 2022;22(1):568.
doi pubmed pmc - Filatov VL, Katrukha AG, Bulargina TV, Gusev NB. Troponin: structure, properties, and mechanism of functioning. Biochemistry (Mosc). 1999;64(9):969-985.
pubmed - Setiadi BM, Lei H, Chang J. Troponin not just a simple cardiac marker: prognostic significance of cardiac troponin. Chin Med J (Engl). 2009;122(3):351-358.
pubmed - Tjora HL, Steiro OT, Langorgen J, Bjorneklett RO, Skadberg O, Bonarjee VVS, Mjelva OR, et al. Diagnostic performance of novel troponin algorithms for the rule-out of non-ST-elevation acute coronary syndrome. Clin Chem. 2022;68(2):291-302.
doi pubmed - Widera C, Giannitsis E, Mueller-Hennessen M, Reimann I, Guba-Quint A, Marquardt I, Bethmann K, et al. Diagnostic and prognostic value of sex- and age-specific cutpoints for high-sensitivity Troponin T in non-ST-elevation acute coronary syndrome. Int J Cardiol. 2019;275:13-19.
doi pubmed - Ishihara M, Nakao K, Ozaki Y, Kimura K, Ako J, Noguchi T, Fujino M, et al. Long-term outcomes of non-ST-elevation myocardial infarction without creatine kinase elevation - The J-MINUET study. Circ J. 2017;81(7):958-965.
doi pubmed - Chenevier-Gobeaux C, Sebbane M, Meune C, Lefebvre S, Dupuy AM, Lefevre G, Peschanski N, et al. Is high-sensitivity troponin, alone or in combination with copeptin, sensitive enough for ruling out NSTEMI in very early presenters at admission? A post hoc analysis performed in emergency departments. BMJ Open. 2019;9(6):e023994.
doi pubmed pmc - Vargas KG, Tajsic M, Latsuzbaia A, Bastian S, Andric T, Kassem M, Jager B, et al. Gender-based differences of copeptin alone or combined with troponin for early rule-out of non-ST-elevation myocardial infarction. Am J Emerg Med. 2021;45:248-253.
doi pubmed - Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, Mautner B, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835-842.
doi pubmed - Guenancia C, Stamboul K, Hachet O, Yameogo V, Garnier F, Gudjoncik A, Cottin Y, et al. Clinical effectiveness of the systematic use of the GRACE scoring system (in addition to clinical assessment) for ischaemic outcomes and bleeding complications in the management of NSTEMI compared with clinical assessment alone: a prospective study. Heart Vessels. 2016;31(6):897-906.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


