| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 15, Number 5, October 2024, pages 377-395
Prevalence, Clinical Manifestations, and Adverse Outcomes of Left Ventricular Noncompaction in Adults: A Systematic Review and Meta-Analysis
Jordan Llerena-Velasteguia, b , Almendra Lopez-Usinaa
, Camila Mantilla-Cisnerosa
aMedical School, Pontifical Catholic University of Ecuador, Quito, Ecuador
bResearch Center, Center for Health Research in Latin America (CISeAL), Quito, Ecuador
Manuscript submitted June 1, 2024, accepted July 7, 2024, published online September 16, 2024
Short title: Left Ventricular Noncompaction
doi: https://doi.org/10.14740/cr1673
| Abstract | ▴Top |
Background: Left ventricular noncompaction (LVNC) is recognized within the spectrum of adult cardiomyopathies for its unique pathophysiologic features and clinical challenges. This condition exhibits a wide range of clinical manifestations, from asymptomatic states to severe cardiovascular complications, making its diagnosis and management challenging. This study aimed to synthesize current data on the prevalence, diagnostic methods, clinical outcomes, and treatment efficacy of LVNC in adults to address gaps in understanding and management strategies.
Methods: A systematic review and meta-analysis of research from 2000 to March 2024 was conducted, focusing on studies involving adults diagnosed with LVNC. This approach aimed to collect data on the prevalence of LVNC, the diagnostic accuracy of different imaging modalities, clinical manifestations, and the impact of different treatment strategies.
Results: The study showed a prevalence of LVNC of 0.5%, with cardiovascular magnetic resonance outperforming echocardiography in diagnosis with a detection rate of 1.3%. Mortality and heart transplantation rates were 12% and 7%, respectively. Significant predictors of adverse outcomes included New York Heart Association (NYHA) class III or IV, ventricular tachycardia, and reduced left ventricular ejection fraction (LVEF), guiding a nuanced approach in tailoring therapeutic strategies to optimize patient care and outcomes.
Conclusions: This study advances the understanding of LVNC by refining diagnostic criteria and evaluating management strategies, highlighting the superiority of cardiovascular magnetic resonance. It identifies predictors of adverse outcomes and assesses treatment efficacy, urging precision in diagnosis and tailored treatments. Its comprehensive analysis and methodological rigor make it a key resource advocating a multidisciplinary approach to improve patient outcomes in LVNC.
Keywords: Left ventricular noncompaction; Cardiovascular magnetic resonance; Diagnostic criteria; Clinical outcomes; Treatment strategies
| Introduction | ▴Top |
Left ventricular noncompaction (LVNC) is emerging as a unique entity within the diverse spectrum of adult cardiomyopathies, characterized by its distinct pathophysiological features and clinical presentation [1]. Characterized by an intricate network of trabeculations in the left ventricular myocardium, LVNC is distinguished not only by its morphological features but also by the clinical challenges it presents [2]. This condition, formerly known as hypertrabeculation syndrome or spongy myocardium, has been the subject of extensive debate regarding its nomenclature, diagnostic criteria, and clinical significance [3]. The clinical manifestations of LVNC are highly variable, ranging from asymptomatic individuals to patients with severe cardiovascular complications, highlighting the diagnostic dilemma and therapeutic challenges associated with this cardiomyopathy [4].
The ambiguity surrounding LVNC extends to its prevalence in the adult population, with estimates varying widely depending on the imaging modality used for diagnosis [5]. Prevalence rates reported in the literature range from a modest 0.014% to an alarming 14.79%, with this variability largely attributed to the diagnostic criteria used and the sensitivity of different imaging techniques [5]. This inconsistency in prevalence data underscores the critical need for a systematic approach to the diagnosis of LVNC, aimed at improving the accuracy of detection and understanding of the epidemiology of the condition [6, 7].
Furthermore, the clinical impact of LVNC is profound, encompassing a spectrum of presentations ranging from heart failure and arrhythmias to thromboembolic events [8]. These manifestations not only complicate the clinical management of patients, but also require a thorough investigation of the efficacy of different treatment strategies [9]. The heterogeneity of clinical outcomes further emphasizes the importance of identifying predictors of adverse events, which could significantly contribute to improving patient management and prognosis [5, 10].
This study carefully addresses the aforementioned gaps in the existing body of knowledge on LVNC, with a particular focus on adults. By conducting a comprehensive literature review and meta-analysis of studies from 2000 to March 2024, this study attempts to synthesize the available data and provide a clearer perspective on the impact and management of LVNC in the adult population. The scope of this study is broad and includes an analysis of the prevalence of LVNC, an examination of its clinical manifestations in various patient demographics, and an evaluation of the efficacy of current treatment modalities. In addition, this research aims to elucidate predictors of adverse outcomes, providing invaluable insight into risk stratification and optimization of patient care.
Through this rigorous investigation, the study makes a significant contribution to the field by providing an updated estimate of the prevalence of LVNC, thereby shedding light on its true epidemiologic footprint. In addition, by delineating the clinical manifestations of the condition, the research helps to refine diagnostic criteria, which is expected to improve the specificity and sensitivity of clinical diagnoses. This, in turn, is expected to mitigate problems associated with both under- and over-diagnosis of LVNC. In addition, the evaluation of treatment strategies within this study will provide critical insight into the most effective approaches to the management of LVNC and guide clinicians in optimizing patient care. Finally, the identification of predictors of adverse outcomes will have a profound impact on the management of LVNC by facilitating more precise risk stratification and enabling tailored therapeutic interventions.
In summary, this study represents a comprehensive and pivotal contribution to the cardiomyopathy literature and addresses important gaps in our understanding of LVNC. Its methodological thoroughness and broad scope make it an invaluable resource for clinicians, researchers and policy makers alike, highlighting the multifaceted complexity of LVNC and underscoring the need for a multidisciplinary approach to its study, diagnosis and management.
| Materials and Methods | ▴Top |
Inclusion and exclusion criteria
To ensure a comprehensive and rigorous analysis of LVNC in the adult population, this study adhered to carefully defined inclusion and exclusion criteria. These criteria were established to accurately delineate the study population, specify the types of studies considered, and outline publication criteria, thereby facilitating the systematic review and meta-analysis process.
Inclusion criteria
The study included research based on the following inclusion parameters.
1) Study population
Only studies that included adults (individuals over 18 years of age) diagnosed with isolated LVNC were considered. This criterion was applied to focus on the adult demographic and to ensure that the findings are relevant to the clinical needs and management strategies of this population.
2) Study design
The analysis included a wide range of study designs to capture a comprehensive dataset, including prospective and retrospective cohort studies, case-control studies, cross-sectional studies, and case series. To maintain statistical power, only studies with at least 10 participants were included.
3) Research focus
To be included, studies had to report on at least one of the following: prevalence of LVNC, diagnostic criteria used, clinical outcomes observed, or treatment strategies implemented. This broad focus allowed for a holistic view of LVNC, including its epidemiology, diagnosis, clinical management, and therapeutic interventions.
4) Language and publication date
The study was limited to research published in English between January 2000 and March 2024. This timeframe was chosen to ensure that the research analyzed is both contemporary and relevant, reflecting the latest advances and understanding in the field of LVNC.
Exclusion criteria
Studies were excluded from this analysis under the following conditions.
1) Pediatric studies
Studies focusing exclusively on pediatric populations (individuals under 18 years of age) were excluded. This decision was made to maintain the study’s focus on adult cases of LVNC, given the different clinical implications and management strategies between these two groups.
2) Mixed population studies
Studies that included patients with LVNC together with patients with concomitant congenital heart disease or other cardiomyopathies were excluded. The aim was to isolate the effects and characteristics of LVNC without the confounding influence of additional cardiomyopathies.
3) Non-original research
The analysis did not include case reports, commentaries, editorials, reviews, animal studies, or in vitro studies. The exclusion of these sources was intended to ensure that the data synthesized were from empirical research involving direct observation or experimentation on human subjects.
4) Language and publication date restrictions
Studies not published in English or published before the year 2000 were excluded. This criterion was applied to ensure the accessibility and relevance of the research to the current clinical and academic discourse on LVNC.
By adhering to these carefully structured inclusion and exclusion criteria, this study aimed to compile and analyze data that would provide a clear, current, and clinically relevant understanding of LVNC in adults. The methodology ensures that the conclusions drawn are based on robust evidence, making a significant contribution to the literature and providing valuable insights for clinicians, researchers and policy makers involved in the management of LVNC.
Search and selection methodology
To ensure a comprehensive and systematic review of LVNC in the adult population, a detailed search and selection methodology was meticulously applied. This methodology was designed to capture the breadth of current research and facilitate in-depth analysis of LVNC prevalence, diagnostic criteria, clinical outcomes, and treatment strategies.
Search strategy
The search strategy was conducted in several prominent electronic databases, including PubMed, Google Scholar, and the Cochrane Library, to include a wide range of scientific publications. The publication inclusion period ranged from January 2000 to March 2024 to ensure the relevance and timeliness of the data analyzed. A strategic combination of keywords and Medical Subject Headings (MeSH) terms was used to maximize the specificity and breadth of the search. The terms used were tailored to capture studies relevant to LVNC in adults using Boolean search logic: (“left ventricular noncompaction” OR “LVNC” OR “noncompaction cardiomyopathy” OR “spongy myocardium”) AND (“adult” OR “adults”). This comprehensive search strategy was developed to identify studies that provide insight into the epidemiology, diagnostic approaches, clinical manifestations, and management strategies for LVNC, thereby ensuring a robust basis for the systematic review and meta-analysis.
Selection methodology
The selection methodology was carefully designed to include studies that provide valuable insights into LVNC in adults. Observational studies including cohort studies, case-control studies, cross-sectional studies, and case series were considered for inclusion. A minimum number of participants was set at 10 to ensure that studies provided a sufficient data pool for meaningful analysis. The focus on adults with isolated LVNC was paramount, with the aim of distilling data specific to this demographic, thus increasing the specificity of the research findings.
There were no demographic restrictions regarding gender, ethnicity, or geographic location, allowing for a diverse and inclusive data set that reflected the global incidence and characteristics of LVNC. This inclusive approach ensured that the research findings would be broadly applicable, enhance the understanding of LVNC in diverse populations, and contribute to the global discourse on this cardiomyopathy.
By adhering to this rigorous search and selection methodology, the study aimed to compile a comprehensive and relevant data set on LVNC in adults. The meticulous design of this methodology ensures the high quality and relevance of the studies included in the analysis, thereby contributing significantly to the existing body of knowledge on LVNC. This approach underscores the study’s potential to inform clinical practice, guide future research directions, and ultimately improve patient outcomes in LVNC.
Data handling
Data extraction
A rigorous data extraction methodology was used to ensure the integrity and completeness of the data analyzed. Two independent reviewers were tasked with extracting data from the included studies using a standardized data extraction form specifically designed for this purpose. This form facilitated the systematic collection of pertinent information, including study characteristics (such as first author’s name, year of publication, study design, and country of origin), participant demographics (including sample size, age, and gender distribution), and specific details related to LVNC (in particular, the imaging modality and diagnostic criteria used in each study). In cases of disagreement between the reviewers, resolution was sought through discussion. If consensus could not be reached, a third reviewer was consulted to arbitrate and ensure the accuracy of the data extraction.
Quality assessment framework
The methodological quality of the studies included in this analysis was carefully assessed using the Newcastle-Ottawa Scale (NOS) for observational studies. The NOS provides a comprehensive framework for assessing the quality of nonrandomized studies, focusing on three critical areas: selection of study participants, comparability of study groups, and ascertainment of the exposure or outcome of interest for case-control or cohort studies, respectively. Each study was assigned a score within these domains, resulting in a total score out of 9. Studies with a score of 7 or more were considered to be of high quality, reflecting robust methodological standards. Those scoring between 4 and 6 were considered to be of moderate quality, while studies scoring below 4 were considered to be of low quality. This stratification ensured a nuanced understanding of the methodological rigor of the studies and informed the synthesis of the findings.
Statistical analysis and synthesis
The synthesis of the data extracted from the included studies began with a narrative summary that summarized the key findings regarding the prevalence of LVNC, diagnostic criteria, observed clinical outcomes, and treatment strategies used. To further quantify these findings, meta-analyses were performed where appropriate, with the aim of pooling data from multiple studies to derive collective insights. Given the expected variability between trials, a random effects model was applied to the meta-analysis. This model accounts for both within-study and between-study heterogeneity, allowing for a more generalized estimate of effect size. The degree of heterogeneity was assessed quantitatively using the I2 statistic, with categories of less than 50%, between 50% and 75%, and greater than 75% indicating low, moderate, and high heterogeneity, respectively. All statistical analyses were performed using sophisticated statistical software, specifically rBiostatistics and Stata (StataCorp Stata MP 16.0), to ensure a rigorous and reliable analytical process.
This review has been successfully registered in the international database PROSPERO, under the ID CRD42024527679. The Institutional Review Board approval and ethics statement are not applicable as this study is based solely on previously published literature. We have adhered strictly to methodological rigor and ethical guidelines in synthesizing the available evidence on the prevalence, clinical manifestations, and adverse outcomes of LVNC in adults.
| Results | ▴Top |
Search overview
The meticulous search and selection process for this systematic review and meta-analysis is illustrated in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart (Fig. 1). Initially, an extensive database search yielded a total of 2,681 studies. Subsequent duplicate removal reduced this number to 2,003, which were then meticulously screened by title and abstract. This screening resulted in the exclusion of 1,752 studies because they did not fit the specific focus of our analysis on LVNC in adults. The intensive screening continued with full-text assessment of 251 studies, of which 179 were inaccessible due to retrieval issues. Of the 72 studies assessed for eligibility, 53 were excluded because they did not meet the strict inclusion criteria established for this review. These criteria were designed to ensure that only studies with appropriate design, population, and outcomes relevant to our analysis were included. Ultimately, 19 studies were deemed eligible for inclusion in our meta-analysis. By adhering to this rigorous process, we ensured the compilation of a high-quality and relevant dataset, providing meaningful and reliable insights into LVNC. This methodology minimizes the risk of bias and enhances the validity of our meta-analysis, ensuring robust conclusions. The characteristics of these studies are summarized in Table 1, which provides a clear overview of the research landscape in LVNC [11-29].
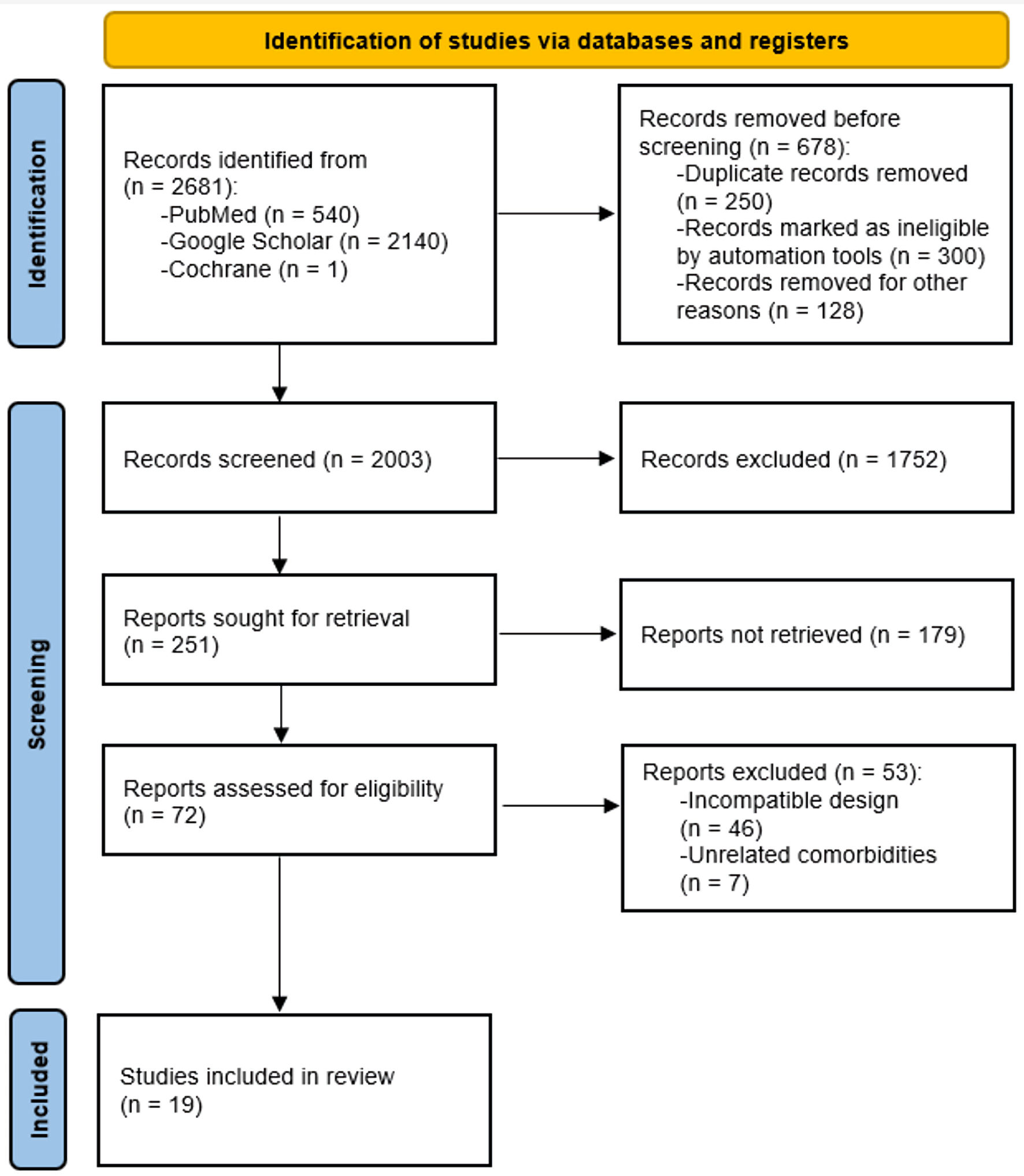 Click for large image | Figure 1. PRISMA diagram for the study selection process. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses. |
 Click to view | Table 1. Summary of the Characteristics of Included Studies |
The integrity and validity of the included studies were rigorously assessed using the NOS, the results of which are detailed in Table 2 [11-29]. Of the studies, five were rated as high quality, scoring between 7 and 9, indicating their robust methodology, comprehensive data collection, and the relevance of their findings to our research question. The remaining 14 studies were of moderate quality, with scores ranging from 4 to 6. Despite this variation, the overall quality of the evidence was considered moderate, highlighting the need for cautious interpretation of the results. This quality assessment underscores the rigorous approach taken in this review to ensure that the synthesis of evidence on the prevalence, diagnostic criteria, and management strategies for LVNC in adults is both reliable and informative.
 Click to view | Table 2. Quality Assessment of Included Studies Using Newcastle-Ottawa Scale |
Regarding the inclusion of funnel plots, our statistical analyses were based on one-group proportion estimates, which typically do not lend themselves to the creation of funnel plots for all aspects under analysis. However, we have generated funnel plots for specific predictors where the data allowed (Fig. 2). These plots illustrate the distribution of study results for critical predictors of adverse outcomes, such as cardiovascular complications, hospitalization for heart failure, left ventricular ejection fraction (LVEF), and New York Heart Association (NYHA) class III or IV. While some asymmetry is observed, it is important to consider the limited number of studies and the inherent heterogeneity in study designs and populations. These funnel plots enhance the transparency of our analysis and provide a visual assessment of potential publication bias, although they should be interpreted with caution due to the aforementioned limitations.
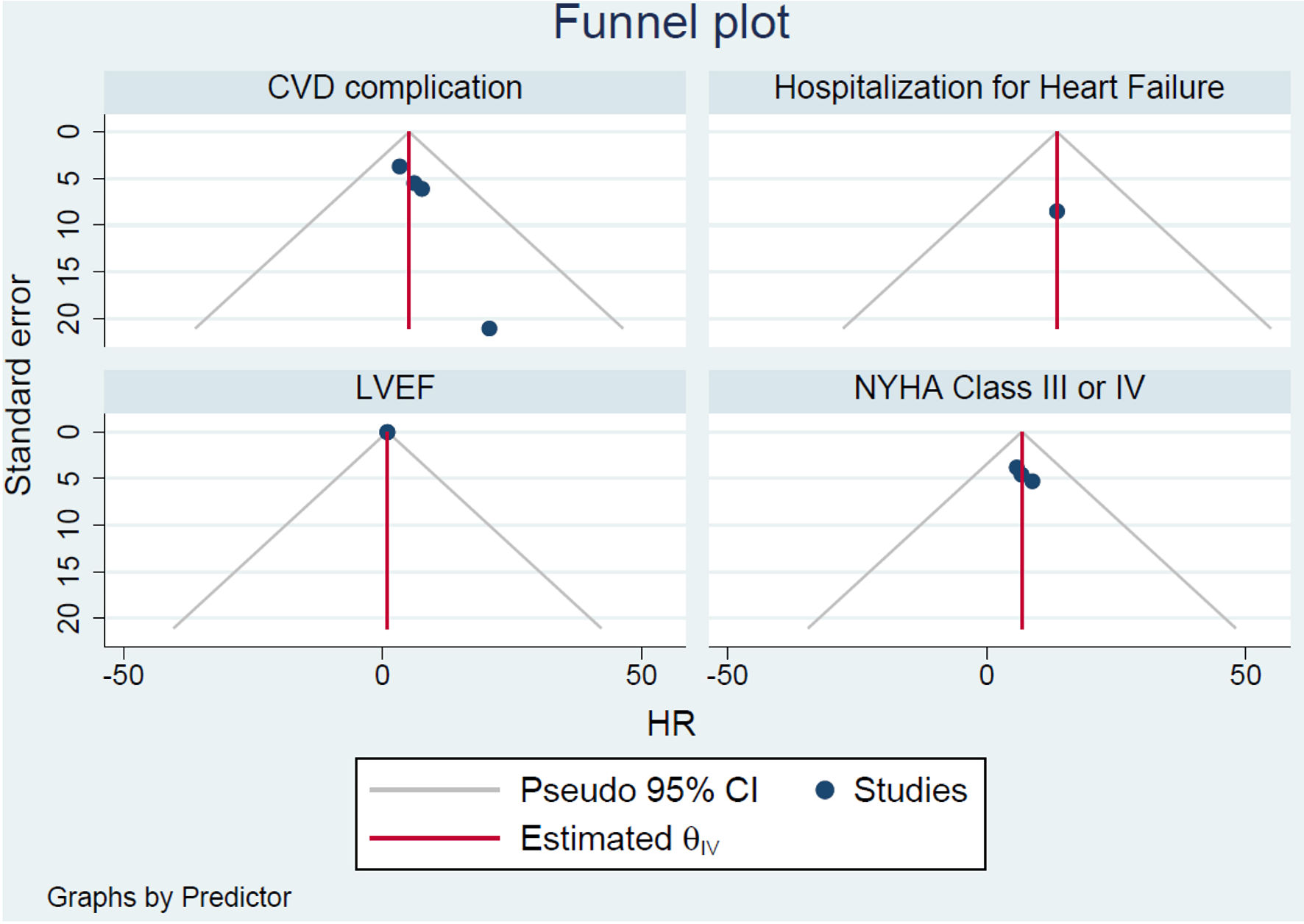 Click for large image | Figure 2. Funnel plot analysis of adverse outcomes in LVNC. LVNC: left ventricular noncompaction; CVD: cardiovascular disease; LVEF: left ventricular ejection fraction; CI: confidence interval; NYHA: New York Heart Association. |
This systematic review and meta-analysis is a major contribution to the existing literature and addresses critical gaps in the understanding of LVNC in adults. Through a comprehensive analysis of prevalence, diagnostic approaches, and treatment efficacy, this study illuminates the complexities surrounding LVNC in the adult population. The findings of this review have implications for clinical practice, providing a basis for the development of more nuanced diagnostic criteria and treatment protocols. In doing so, it reinforces the critical need for ongoing research in this area and underscores the role of this article in advancing the cardiologic discourse surrounding LVNC.
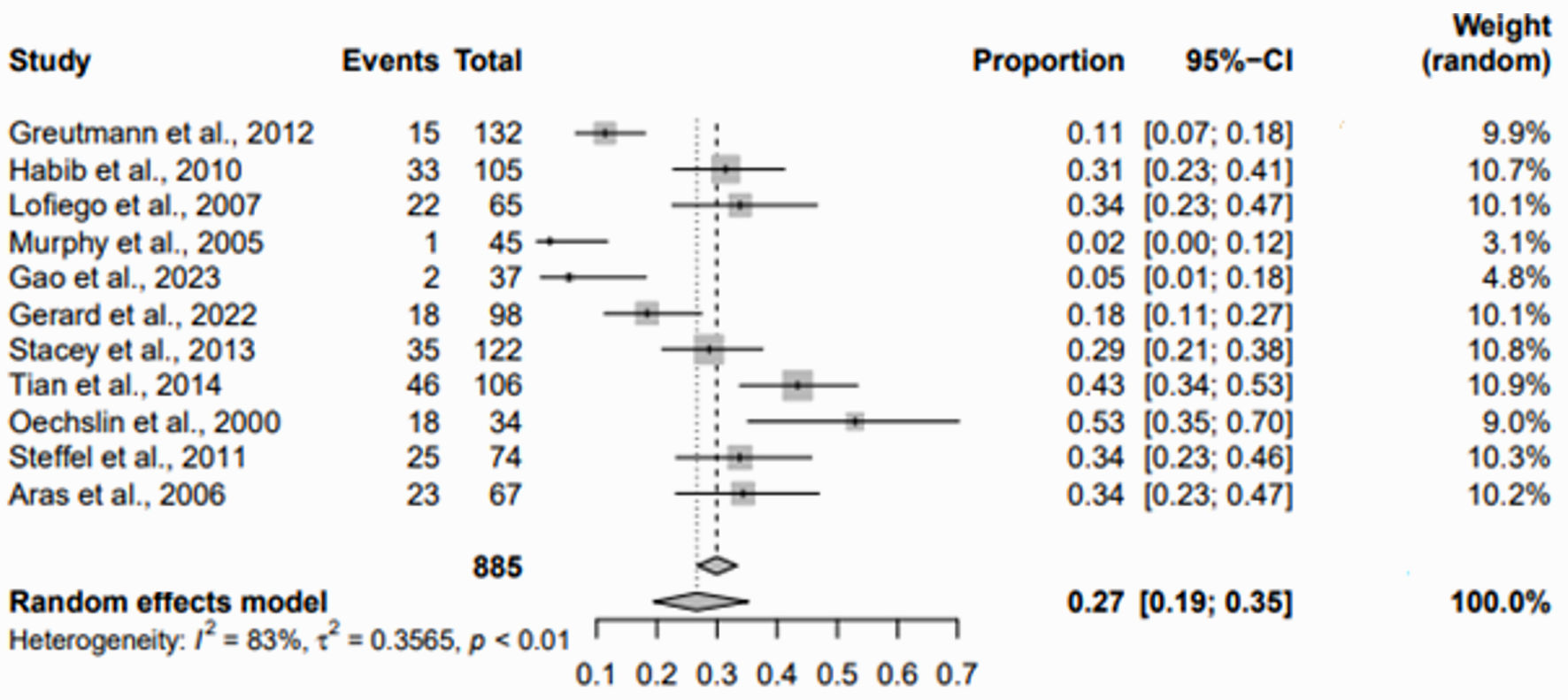
Prevalence and diagnostic criteria
To assess the prevalence of LVNC in the adult population, this analysis used a refined approach to obtain a more accurate pooled prevalence estimate. Given the inherently low prevalence of LVNC, incidence figures from 10 different studies, which reported prevalence rates ranging from 0.014% to 6.9%, were mathematically adjusted. This adjustment involved multiplying the number of events by 10, thereby increasing the precision of the pooled effect calculation. The resulting meta-analysis yielded a pooled prevalence estimate of 0.5% (95% confidence interval (CI): 0.2-1.5%), despite the high degree of heterogeneity among the studies (I2 = 100%) (Fig. 3).
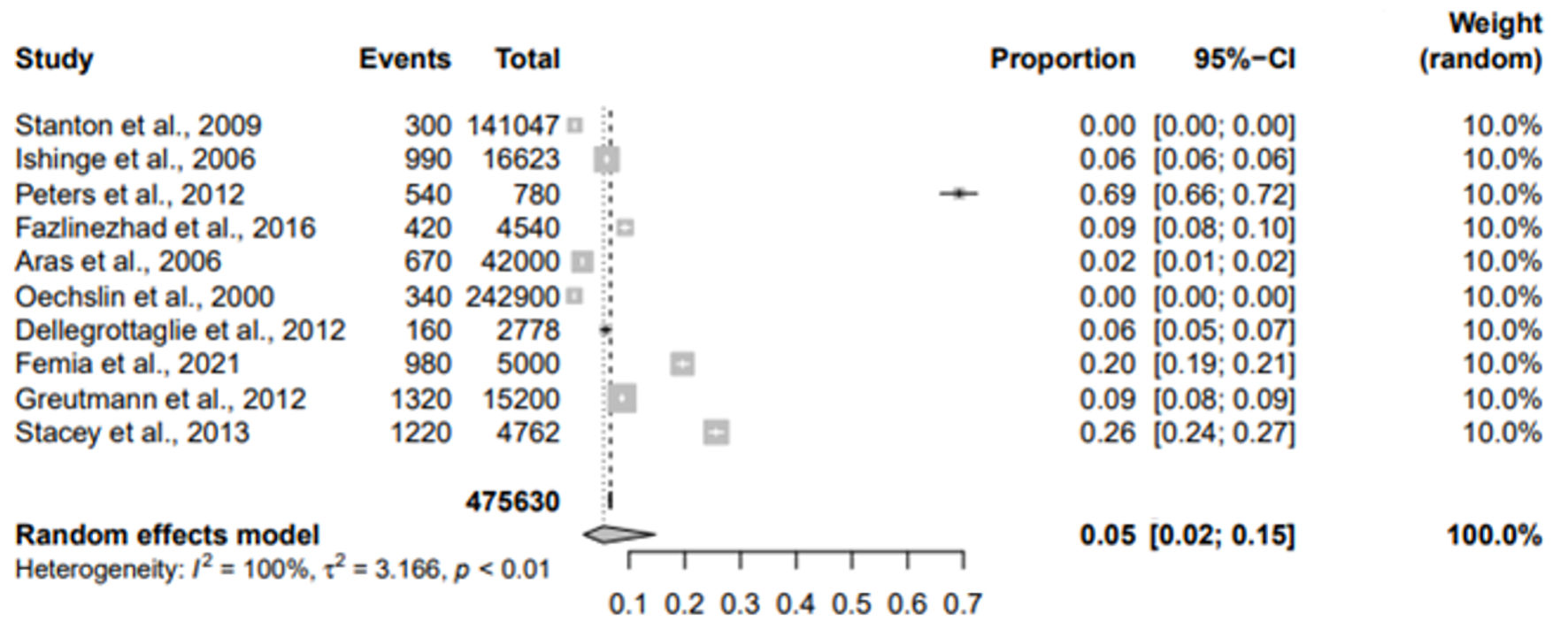 Click for large image | Figure 3. Forest plot for the prevalence of LVNC in adult population. LVNC: left ventricular noncompaction; CI: confidence interval. |
Further investigation focused on comparing the diagnostic capabilities of echocardiography versus cardiovascular magnetic resonance (CMR) imaging in identifying LVNC cases in the adult population. This comparative meta-analysis revealed different pooled prevalence estimates based on the imaging modality used. Specifically, studies using echocardiography reported a pooled prevalence of 0.3% (95% CI: 0.1-1.4%) (Fig. 4), whereas studies using CMR imaging techniques reported a higher pooled prevalence of 1.3% (95% CI: 0.7-2.3%) (Fig. 5). This discrepancy underscores the superior sensitivity of CMR in detecting LVNC cases, compared to echocardiography and highlights the critical role of imaging modality selection in the accurate diagnosis of LVNC.
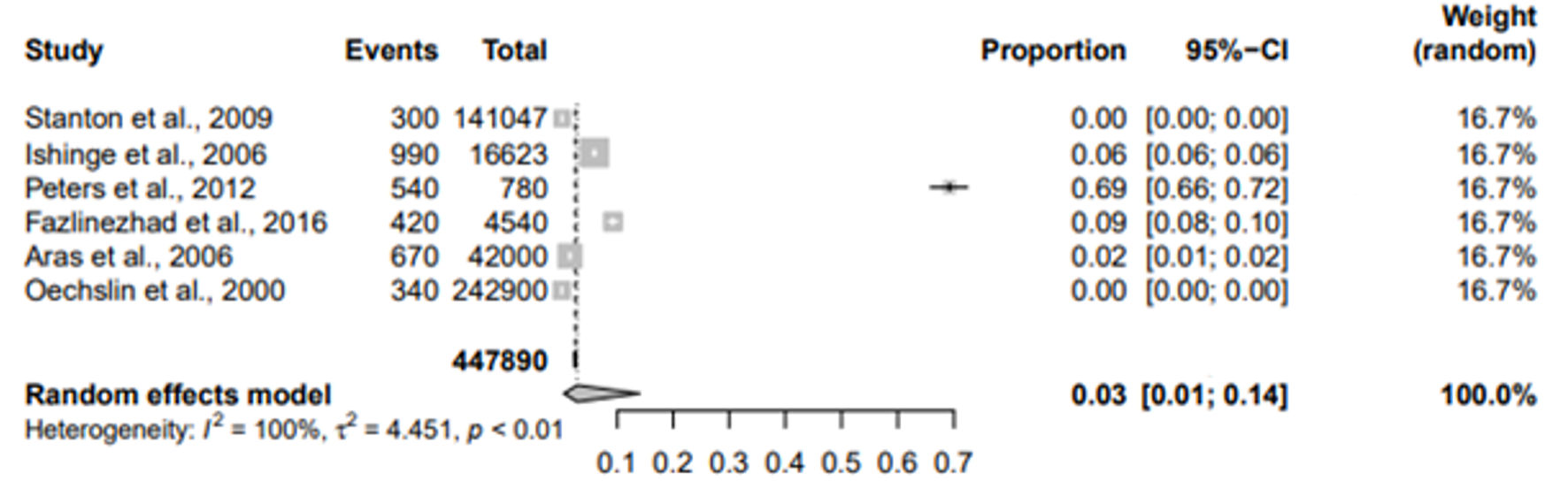 Click for large image | Figure 4. Forest plot for the prevalence of LVNC in adult population on echocardiography. LVNC: left ventricular noncompaction; CI: confidence interval. |
 Click for large image | Figure 5. Forest plot for the prevalence of LVNC in adult population on CMR. LVNC: left ventricular noncompaction; CI: confidence interval; CMR: cardiovascular magnetic resonance. |
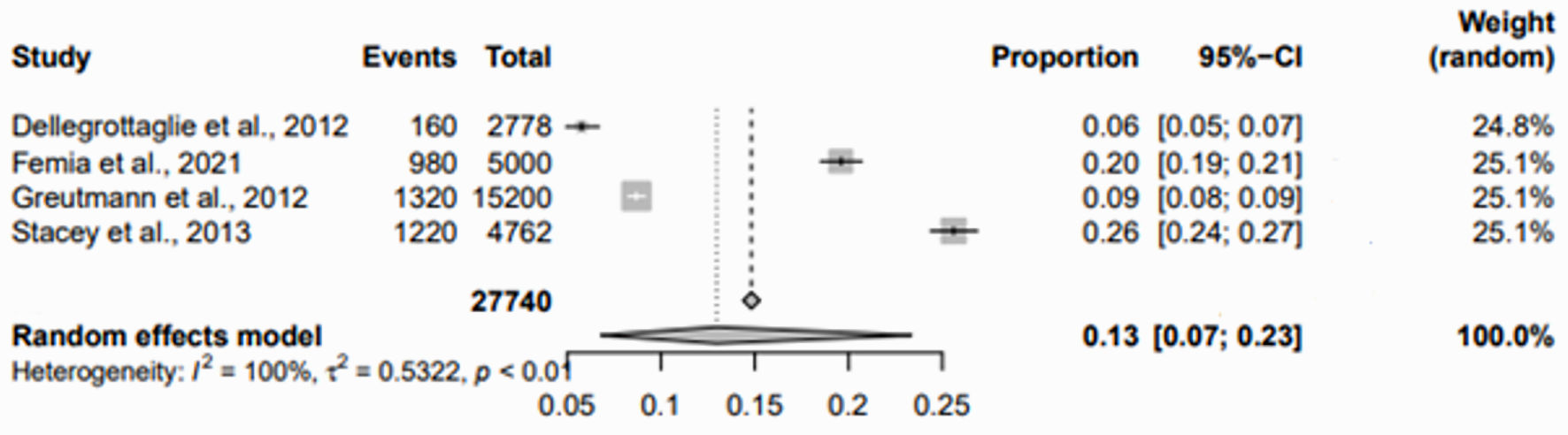
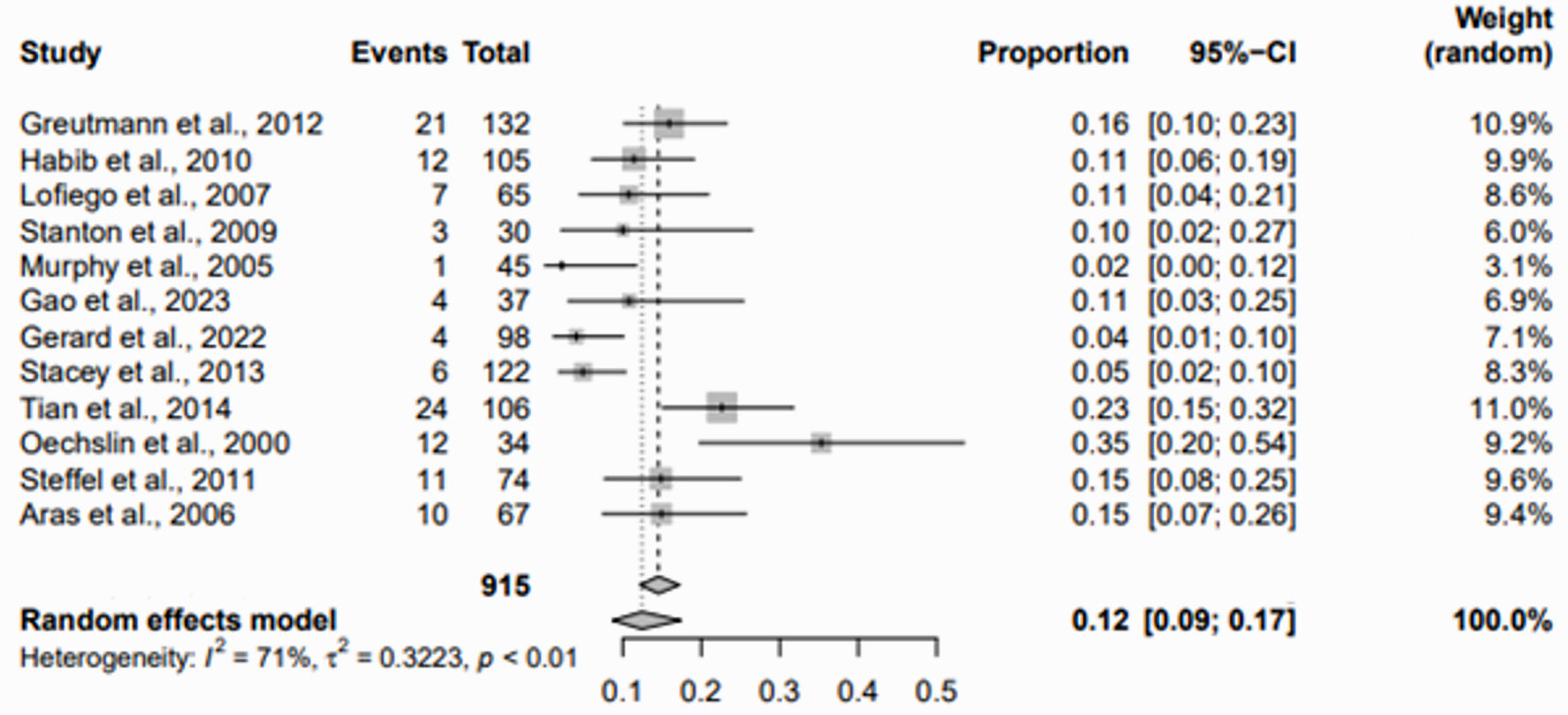
Clinical outcomes and treatment strategies
The review of clinical outcomes associated with LVNC in adults prioritized the analysis of adverse outcomes, with a focus on mortality and the need for heart transplantation. Pooled data from 12 studies showed a notable prevalence of mortality in the adult LVNC population, with a pooled prevalence rate of 12% (95% CI: 9-17%) and moderately high heterogeneity (I2 = 71%) (Fig. 6). In addition, analysis of heart transplantation data from eight studies showed a pooled prevalence of 7% (95% CI: 5-10%) with lower heterogeneity (I2 = 38%) (Fig. 7).
 Click for large image | Figure 6. Forest plot for the prevalence of mortality in adults with LVNC. LVNC: left ventricular noncompaction; CI: confidence interval. |
 Click for large image | Figure 7. Forest plot for the incidence of heart transplantation in adults with LVNC. LVNC: left ventricular noncompaction; CI: confidence interval. |
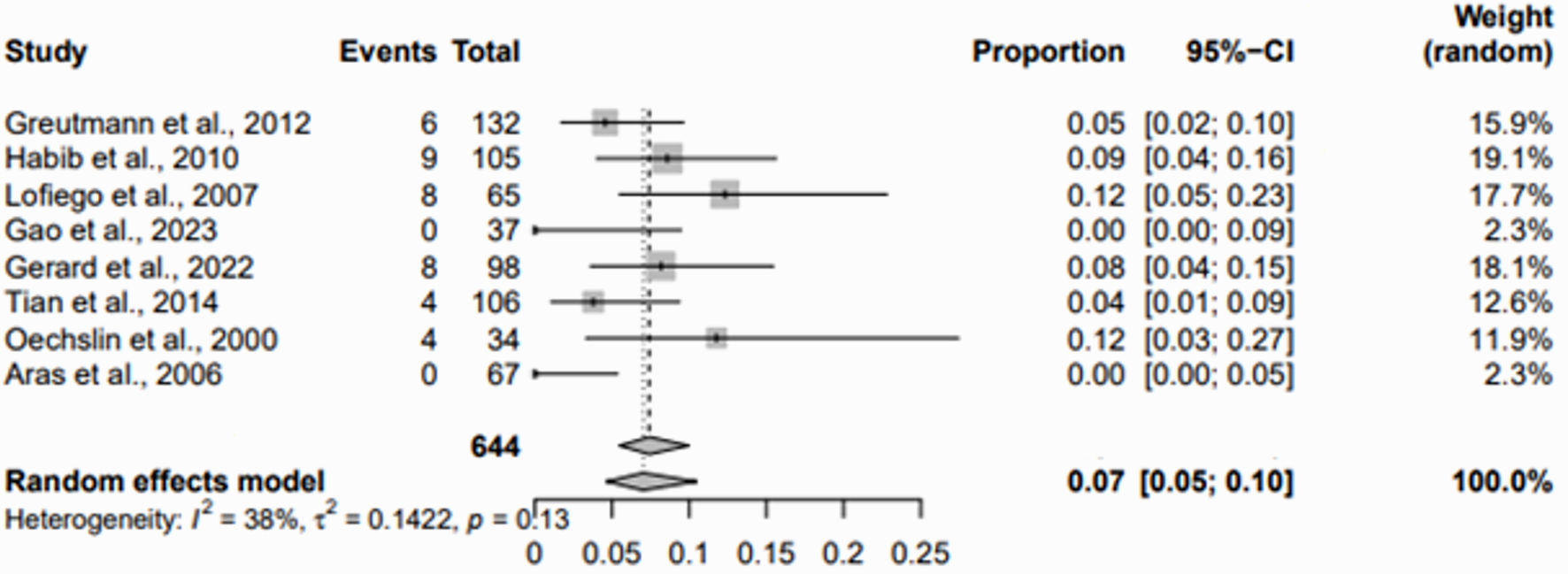
In addition to adverse outcomes, the study examined the common clinical manifestations observed in individuals diagnosed with LVNC. The analysis highlighted heart failure, arrhythmias and thromboembolic events as the predominant clinical manifestations. Specifically, heart failure was reported with a pooled prevalence of 27% (95% CI: 19-35%) (Fig. 8), arrhythmias with 17% (95% CI: 11-25%) (Fig. 9), and thromboembolic events with 7% (95% CI: 5-10%) (Fig. 10).
 Click for large image | Figure 8. Forest plot for the prevalence of heart failure in adults with LVNC. LVNC: left ventricular noncompaction; CI: confidence interval. |
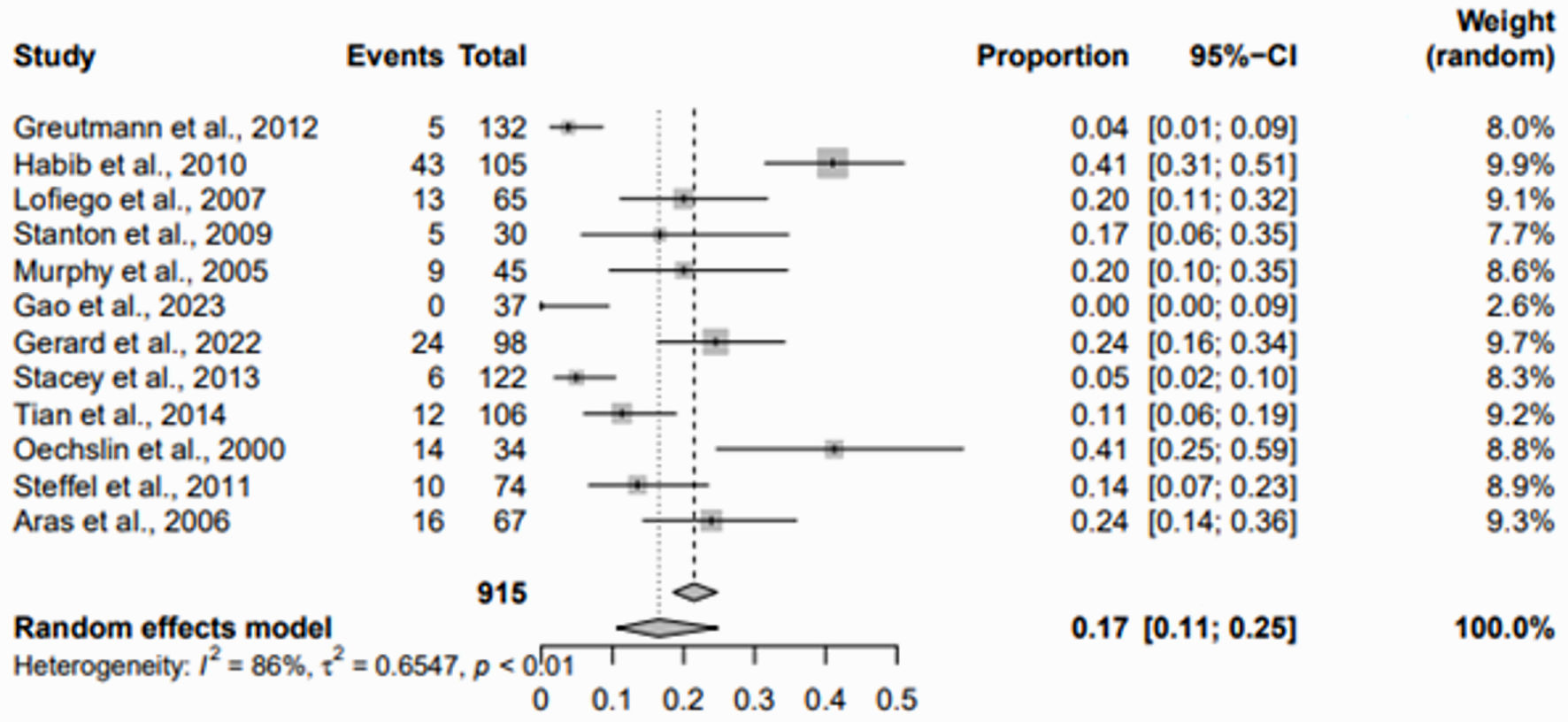 Click for large image | Figure 9. Forest plot for the prevalence of arrhythmic events in adults with LVNC. LVNC: left ventricular noncompaction; CI: confidence interval. |
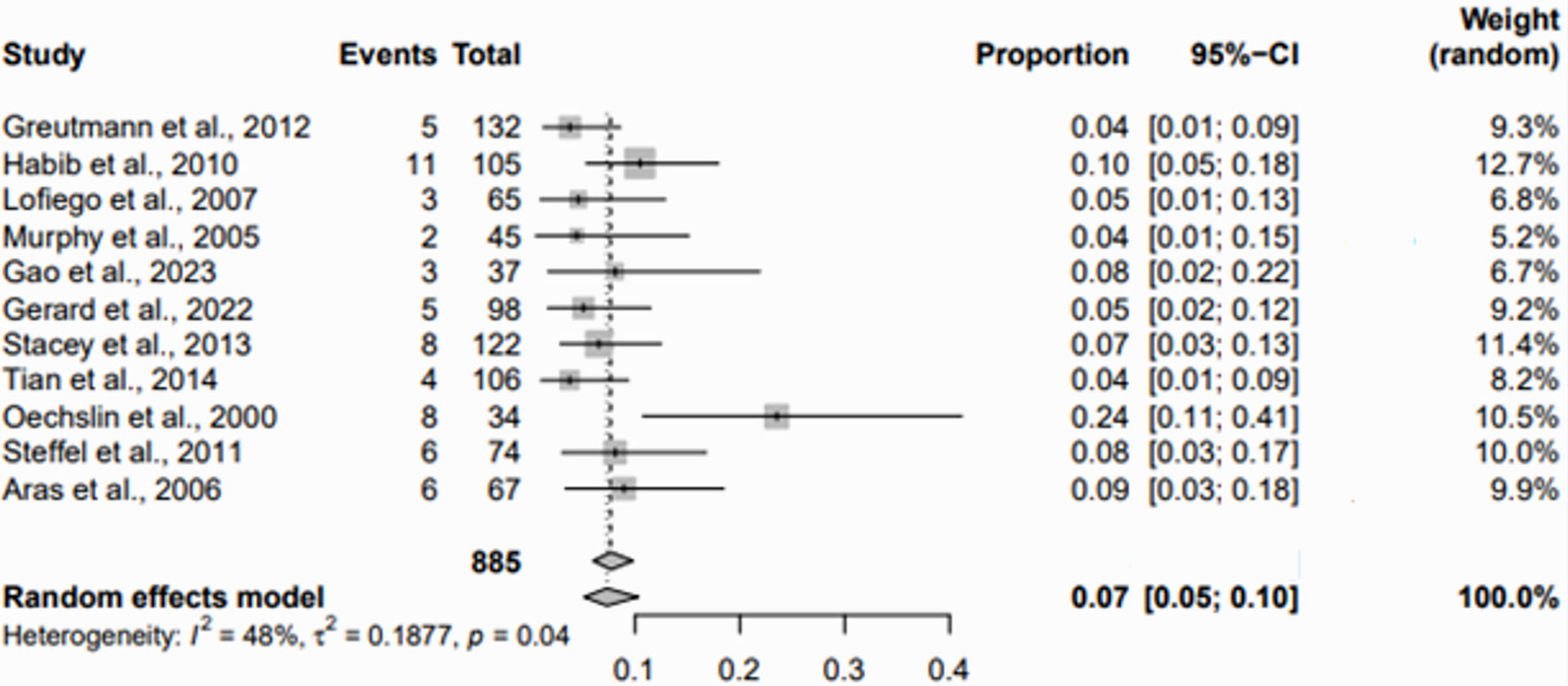 Click for large image | Figure 10. Forest plot for the prevalence of thromboembolic events in adults with LVNC. LVNC: left ventricular noncompaction; CI: confidence interval. |
Treatment strategies for LVNC are tailored to individual patient needs and include pharmacological therapies such as angiotensin-converting enzyme (ACE) inhibitors in 10 trials, angiotensin receptor blockers (ARBs) in 10 trials, beta-blockers in 11 trials, diuretics including spironolactone in five trials, anticoagulants including warfarin in eight trials, aspirin in eight trials, digoxin in two trials, and amiodarone in three trials. In addition, device-based therapies such as implantable cardioverter defibrillator (ICD) therapy for arrhythmia management were reported in three studies. Routine evaluation, including clinical assessment, electrocardiography, and echocardiography, is the cornerstone of LVNC management, with extended electrocardiogram (ECG) monitoring recommended to detect asymptomatic arrhythmias despite variable detection rates [30]. Exercise guidelines recommend against competitive sports for patients with significant risk factors, while allowing participation in asymptomatic individuals with normal function [5]. This approach extends to genetic testing and family screening to identify individuals at risk [31]. Management of complications follows standard guidelines, with treatment based on clinical manifestations; there is no specific therapy for LVNC itself [24]. Advanced therapies, including transplantation, are considered for end-stage heart failure [32]. The comprehensive management strategy integrates evidence-based practices with patient-specific considerations to optimize outcomes [33]. However, heterogeneous reporting across studies precludes meta-analysis for treatment strategies, underscoring the complexity and personalized nature of LVNC management.
This comprehensive analysis of clinical outcomes and treatment strategies for LVNC in adults provides valuable insights into the impact of the condition and the efficacy of current therapeutic approaches, contributing to a deeper understanding of LVNC management in the cardiology community.
Predictors of adverse outcomes
The identification and analysis of predictors of adverse outcomes in adults with LVNC was a central component of this study. This analysis integrates a comprehensive review of several clinical and demographic factors reported in the literature as potential predictors of mortality or need for heart transplantation in this patient population. Primary predictors identified include NYHA functional class, ventricular tachycardia (VT), LVEF, bundle branch block (BBB), left ventricular end-diastolic diameter (LVEDD), supraventricular tachycardia (SVT), left atrial diameter (LAD), age, hospitalization for heart failure, atrial fibrillation (AF), systolic blood pressure (SBP), left ventricular systolic function (LVSF), and ventricular ectopic beats (VES), as detailed in Table 3 [11-29].
 Click to view | Table 3. Clinical Manifestations, Adverse Outcomes, and Predictors of LVNC in Adults |
Because of the heterogeneity in the reporting of these predictors among the included studies, a focused subgroup meta-analysis was performed. This analysis specifically examined the impact of cardiovascular complications, heart failure hospitalization, LVEF, and NYHA class III or IV on the incidence of adverse outcomes in the adult LVNC cohort. The results showed significant associations between these predictors and an increased risk of death or heart transplantation, indicating their critical role in the prognosis of LVNC patients. Specifically, cardiovascular complications had a hazard ratio (HR) of 5.12 (95% CI: -0.20 - 10.45), hospitalization for heart failure had a HR of 13.55 (95% CI: -3.11 - 30.21), LVEF had a HR of 0.92 (95% CI: 0.88 - 0.97), and NYHA class III or IV had a HR of 6.78 (95% CI: 1.74 - 11.82) (Fig. 11). These findings suggest that the presence of LVNC alone is not the sole determinant of outcomes. Instead, specific clinical factors significantly contribute to the risk of adverse events, thereby necessitating a tailored approach to patient management. The figure includes HR values and their corresponding CIs, which clearly indicate the statistical significance of each predictor, ensuring accurate interpretation of the data despite the absence of an identity line. These findings underscore the necessity for a nuanced approach in managing LVNC, as the significant variability in clinical manifestations and risk profiles among patients necessitates individualized treatment strategies to optimize therapeutic interventions and improve patient outcomes. This nuanced understanding is essential for optimizing therapeutic strategies and improving patient care in individuals diagnosed with LVNC.
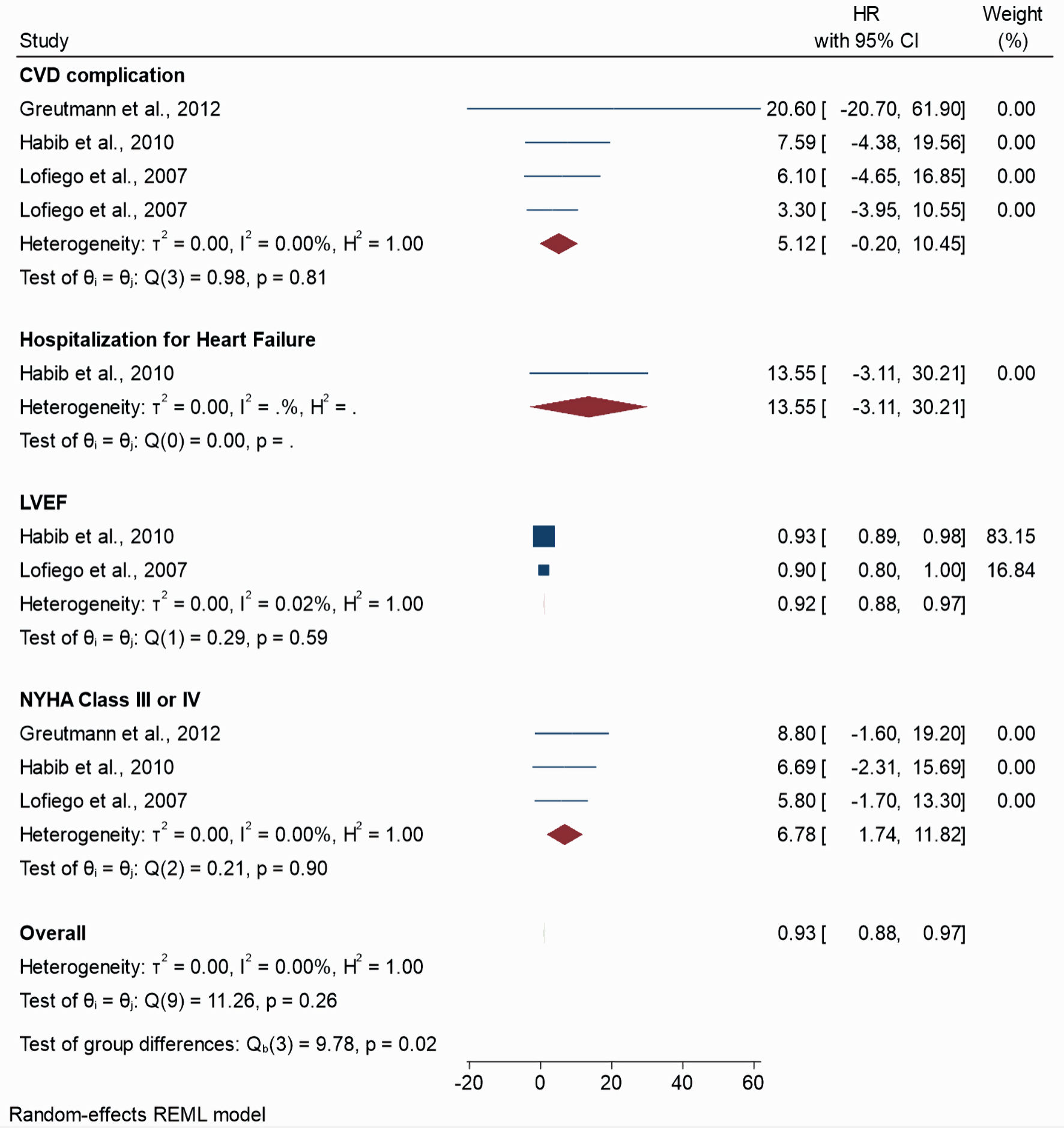 Click for large image | Figure 11. Forest plot for the predictors of death or heart transplantation in adults with LVNC. LVNC: left ventricular noncompaction; CVD: cardiovascular disease; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association; HR: hazard ratio; CI: confidence interval. |
This detailed analysis of predictors underscores the complexity of managing LVNC in the adult population and highlights the need for a tailored approach to the monitoring and management of this patient population, taking into account these significant predictors to reduce the risk of adverse clinical outcomes.
| Discussion | ▴Top |
Interpretation of findings
The results of this study of LVNC in the adult population elucidate important aspects of the prevalence of the condition, diagnostic criteria, and management strategies, adding to the current understanding of this complex cardiomyopathy. With a pooled prevalence estimate of 0.5% (95% CI: 0.2-1.5%), the study highlights the considerable heterogeneity in detection rates of LVNC, reflecting method-dependent variability and the superior sensitivity of CMR over echocardiography. The introduction of a cardiac computed tomography (CCT) non-compacted to compacted (NC/C) ratio of ≥ 1.8 as a diagnostic criterion represents an advance in the field, potentially improving diagnostic accuracy and mitigating the challenges of underdiagnosis or misdiagnosis associated with LVNC.
In terms of treatment strategies, the analysis highlights the prevalent use of pharmacological therapies alongside the role of implantable devices, which is consistent with current management approaches while providing a detailed view of treatment modalities in practice. In addition, the study identifies predictors of adverse outcomes, such as cardiovascular complications and hospitalization for heart failure, providing important insights for clinical management and risk stratification.
Contextual comparison
In contrast to the existing literature on LVNC, particularly in adults, the findings of this study on the prevalence of LVNC [5] and the diagnostic utility of CMR contribute to a growing body of evidence on the heterogeneity of the condition and the diagnostic challenges [32]. While confirming the variability reported in previous studies, this study introduces new diagnostic criteria that may refine the approach to the diagnosis of LVNC [31]. In addition, the detailed examination of treatment strategies and predictors of adverse outcomes addresses a significant gap in the literature and provides a better understanding of LVNC management and its implications for patient care [24].
Clinical and research implications
The implications of these findings for clinical practice are profound, providing a comprehensive overview of the prevalence, diagnostic criteria, and treatment modalities of LVNC. This facilitates improved navigation of the complexities associated with LVNC, improving diagnostic accuracy and optimizing patient management. The identification of specific predictors of adverse outcomes will further aid clinical decision making, allowing for more personalized and effective interventions.
From a research perspective, the study highlights the need for further investigation of LVNC, particularly in terms of standardizing diagnostic criteria and exploring the efficacy of treatment approaches. The gaps identified, such as variability in diagnostic methods and treatment reporting, provide clear directions for future research that could lead to more refined management guidelines and improved patient outcomes.
Two-dimensional speckle tracking echocardiography (STE) has emerged as a novel and feasible tool for assessing LVNC. STE provides detailed insights into myocardial mechanics, offering a noninvasive and widely available alternative to CMR imaging. Studies have demonstrated the utility of STE in comparing global and regional left ventricular function and rotational mechanics between LVNC and other cardiomyopathies, such as hypertrophic cardiomyopathy [34]. Additionally, STE has shown that in LVNC, myocardial efficiency is severely diminished, with left ventricular function appearing to depend mainly on the compact myocardial wall layer [35]. These findings suggest that STE can be a valuable tool in the comprehensive evaluation and management of patients with LVNC.
Recent studies have suggested that circulating microRNAs (miRNAs) may serve as potential biomarkers for myocardial fibrosis in LVNC patients. Specifically, miR-21, miR-29a, miR-30d, and miR-133a have been identified as being significantly upregulated in LVNC patients with late gadolinium enhancement (LGE) detected by CMR imaging, indicating the presence of myocardial fibrosis [36]. These miRNAs offer a noninvasive alternative for detecting fibrosis, which traditionally relies on invasive techniques such as endomyocardial biopsy or noninvasive methods like CMR. Additionally, integrating molecular approaches, such as miRNA profiling, with echocardiographic deformation imaging techniques like two-dimensional STE, can enhance the detection and characterization of myocardial fibrosis [37]. This combination of advanced imaging and molecular biomarkers holds promise for improving the diagnosis and management of myocardial fibrosis in LVNC patients.
Limitations and strengths
The review has several limitations, including the exclusion of non-English literature, which may introduce language bias, and the heterogeneity of diagnostic criteria across included studies, which reflects the broader challenge of standardizing LVNC diagnosis. In addition, the variability in outcome reporting highlights the need for consistent and standardized reporting practices in LVNC research. Another significant limitation is the time span over which the studies were collected, encompassing a period of 20 years. During this time, therapies for heart failure have undergone substantial changes and advancements. These therapeutic developments likely influenced patient outcomes and could have introduced variability in the results. It is essential to consider that the management strategies and treatment protocols for heart failure at the beginning of this period were markedly different from current practices, potentially affecting the generalizability and applicability of the findings. Future research should aim to account for these changes by stratifying data based on the period of study or focusing on more contemporary studies to provide a clearer picture of current outcomes in LVNC.
However, the strengths of the review lie in its comprehensive prevalence estimates, the introduction of a novel diagnostic criterion, and the detailed examination of clinical manifestations, treatment strategies, and predictors of adverse outcomes. These contributions significantly advance the understanding of LVNC and support a nuanced approach to diagnosis and management. This research represents a major advance in the effort to unravel the complexities of LVNC and serves as an essential reference for future clinical and research efforts.
In conclusion, this study represents a critical contribution to cardiology literature and addresses important gaps in the understanding of LVNC. Through a comprehensive analysis, it sheds light on the intricacies of LVNC diagnosis and management, providing insights that could inform clinical practice and guide future research directions, thereby improving the care and outcomes of patients with this challenging cardiomyopathy.
Conclusions
This comprehensive study significantly advances the understanding of LVNC in the adult population and provides important insights into its prevalence, diagnostic criteria, clinical manifestations, and management strategies. By systematically reviewing and meta-analyzing studies from January 2000 to March 2024, the review provides an updated prevalence estimate and highlights the importance of diagnostic accuracy, which is enhanced by the use of CMR over echocardiography. It also identifies key predictors of adverse outcomes, enabling improved patient management and risk stratification. The analysis of treatment strategies, including pharmacological and device-based therapies, contributes to a more effective clinical management framework for LVNC. In the context of current literature, this study fills critical gaps, particularly in refining diagnostic criteria and understanding treatment efficacy. Its findings underscore the need for a nuanced approach to the diagnosis and management of LVNC, emphasizing the role of tailored therapeutic interventions. This research will inform clinical practice and stimulate further investigation to refine management guidelines and ultimately improve patient outcomes in LVNC. The study’s methodological rigor and comprehensive scope make it an important addition to the cardiomyopathy literature, highlighting the complex nature of LVNC and advocating for a multidisciplinary approach to its investigation and management.
Learning points
The study has the following learning points: 1) emphasizes the critical role of CMR imaging in improving the diagnostic accuracy of LVNC, surpassing traditional echocardiography, and refining diagnostic standards; 2) reviews clinical outcomes and management strategies, highlighting the profound impact of LVNC on patient care and the efficacy of specific therapeutic interventions; 3) identifies critical predictors of adverse outcomes, providing new insights into risk stratification and the potential for tailored treatment approaches in the adult LVNC population; 4) provides a comprehensive review and meta-analysis of LVNC in adults, addressing significant gaps in our understanding of prevalence, diagnosis, and management; 5) calls for a multidisciplinary approach to the study, diagnosis, and treatment of LVNC, emphasizing the need for uniform diagnostic criteria and individualized therapeutic strategies to improve patient outcomes.
Acknowledgments
The author has no acknowledgements to declare, reflecting the independent completion of the work.
Financial Disclosure
No funding was received for the conduct of this study or the preparation of this article, indicating that there are no financial sources to declare.
Conflict of Interest
The author declares no conflict of interest to ensure the impartiality of the study.
Informed Consent
Not applicable.
Author Contributions
Jordan Llerena-Velastegui, MD: supervision, conceptualization, writing - original draft, writing - review and editing. Almendra Lopez-Usina, medical student: data curation, formal analysis, writing - review & editing. Camila Mantilla-Cisneros, medical student: conceptualization, writing - original draft, writing - review & editing, methodology.
Data Availability
All data generated or analyzed during this study are included in this published article, and further inquiries should be directed to the corresponding author.
| References | ▴Top |
- Sarma RJ, Chana A, Elkayam U. Left ventricular noncompaction. Prog Cardiovasc Dis. 2010;52(4):264-273.
doi pubmed - Mendpara V, Endreddy JKR, Gajula S, Ravulapalli P, Kumar M, Kaur P, Thakkar M. Overlapping phenotypes of alcoholic cardiomyopathy and left ventricular non-compaction: a case report and discussion of converging cardiomyopathies. Cureus. 2023;15(11):e48220.
doi pubmed pmc - Aung N, Doimo S, Ricci F, Sanghvi MM, Pedrosa C, Woodbridge SP, Al-Balah A, et al. Prognostic significance of left ventricular noncompaction: systematic review and meta-analysis of observational studies. Circ Cardiovasc Imaging. 2020;13(1):e009712.
doi pubmed pmc - Hirono K, Ichida F. Left ventricular noncompaction: a disorder with genotypic and phenotypic heterogeneity-a narrative review. Cardiovasc Diagn Ther. 2022;12(4):495-515.
doi pubmed pmc - Ross SB, Jones K, Blanch B, Puranik R, McGeechan K, Barratt A, Semsarian C. A systematic review and meta-analysis of the prevalence of left ventricular non-compaction in adults. Eur Heart J. 2020;41(14):1428-1436.
doi pubmed - Arbustini E, Favalli V, Narula N, Serio A, Grasso M. Left ventricular noncompaction: a distinct genetic cardiomyopathy? J Am Coll Cardiol. 2016;68(9):949-966.
doi pubmed - Casas G, Limeres J, Oristrell G, Gutierrez-Garcia L, Andreini D, Borregan M, Larranaga-Moreira JM, et al. Clinical risk prediction in patients with left ventricular myocardial noncompaction. J Am Coll Cardiol. 2021;78(7):643-662.
doi pubmed - Ichida F. Left ventricular noncompaction - Risk stratification and genetic consideration. J Cardiol. 2020;75(1):1-9.
doi pubmed - Mirza H, Mohan G, Khan W, Alkhatib A, Kaur I, Asif M, Shah A, et al. A review of left ventricular non-compaction cardiomyopathy (LVNC). J Community Hosp Intern Med Perspect. 2022;12(6):51-63.
doi pubmed pmc - Rojanasopondist P, Nesheiwat L, Piombo S, Porter GA, Jr., Ren M, Phoon CKL. Genetic basis of left ventricular noncompaction. Circ Genom Precis Med. 2022;15(3):e003517.
doi pubmed - Greutmann M, Mah ML, Silversides CK, Klaassen S, Attenhofer Jost CH, Jenni R, Oechslin EN. Predictors of adverse outcome in adolescents and adults with isolated left ventricular noncompaction. Am J Cardiol. 2012;109(2):276-281.
doi pubmed - Habib G, Charron P, Eicher JC, Giorgi R, Donal E, Laperche T, Boulmier D, et al. Isolated left ventricular non-compaction in adults: clinical and echocardiographic features in 105 patients. Results from a French registry. Eur J Heart Fail. 2011;13(2):177-185.
doi pubmed - Lofiego C, Biagini E, Pasquale F, Ferlito M, Rocchi G, Perugini E, Bacchi-Reggiani L, et al. Wide spectrum of presentation and variable outcomes of isolated left ventricular non-compaction. Heart. 2007;93(1):65-71.
doi pubmed pmc - Stanton C, Bruce C, Connolly H, Brady P, Syed I, Hodge D, Asirvatham S, et al. Isolated left ventricular noncompaction syndrome. Am J Cardiol. 2009;104(8):1135-1138.
doi pubmed - Murphy RT, Thaman R, Blanes JG, Ward D, Sevdalis E, Papra E, Kiotsekoglou A, et al. Natural history and familial characteristics of isolated left ventricular non-compaction. Eur Heart J. 2005;26(2):187-192.
doi pubmed - Gao S, Zhang S, Wang Z, Wu M, Gu C, Bai R, Liu M, et al. Long-term prognosis of different subtypes of left ventricular noncompaction cardiomyopathy patients: a retrospective study in China. J Cardiovasc Dev Dis. 2023;10(9):369.
doi pubmed pmc - Gerard H, Iline N, Martel H, Nguyen K, Richard P, Donal E, Eicher JC, et al. Prognosis of adults with isolated left ventricular non-compaction: results of a prospective multicentric study. Front Cardiovasc Med. 2022;9:856160.
doi pubmed pmc - Fazlinezhad A, Vojdanparast M, Sarafan S, Nezafati P. Echocardiographic characteristics of isolated left ventricular noncompaction. ARYA Atheroscler. 2016;12(5):243-247.
pubmed pmc - Ishige A, Sawada H, Uejima T. Demographics and clinical characteristics of the isolated noncompaction of the ventricular myocardium. J Echocardiogr. 2006;4(4):117-122.
- Stacey RB, Andersen MM, St Clair M, Hundley WG, Thohan V. Comparison of systolic and diastolic criteria for isolated LV noncompaction in CMR. JACC Cardiovasc Imaging. 2013;6(9):931-940.
doi pubmed - Peters F, Khandheria BK, dos Santos C, Matioda H, Maharaj N, Libhaber E, Mamdoo F, et al. Isolated left ventricular noncompaction in sub-Saharan Africa: a clinical and echocardiographic perspective. Circ Cardiovasc Imaging. 2012;5(2):187-193.
doi pubmed - Tian T, Liu Y, Gao L, Wang J, Sun K, Zou Y, Wang L, et al. Isolated left ventricular noncompaction: clinical profile and prognosis in 106 adult patients. Heart Vessels. 2014;29(5):645-652.
doi pubmed - Femia G, Zhu D, Choudhary P, Ross SB, Muthurangu V, Richmond D, Celermajer DS, et al. Long term clinical outcomes associated with CMR quantified isolated left ventricular non-compaction in adults. Int J Cardiol. 2021;328:235-240.
doi pubmed - Oechslin EN, Attenhofer Jost CH, Rojas JR, Kaufmann PA, Jenni R. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol. 2000;36(2):493-500.
doi pubmed - Steffel J, Hurlimann D, Namdar M, Despotovic D, Kobza R, Wolber T, Holzmeister J, et al. Long-term follow-up of patients with isolated left ventricular noncompaction: role of electrocardiography in predicting poor outcome. Circ J. 2011;75(7):1728-1734.
doi pubmed - Nucifora G, Aquaro GD, Pingitore A, Masci PG, Lombardi M. Myocardial fibrosis in isolated left ventricular non-compaction and its relation to disease severity. Eur J Heart Fail. 2011;13(2):170-176.
doi pubmed - Dellegrottaglie S, Pedrotti P, Roghi A, Pedretti S, Chiariello M, Perrone-Filardi P. Regional and global ventricular systolic function in isolated ventricular non-compaction: pathophysiological insights from magnetic resonance imaging. Int J Cardiol. 2012;158(3):394-399.
doi pubmed - Cheng H, Zhao S, Jiang S, Yu J, Lu M, Ling J, Zhang Y, et al. Cardiac magnetic resonance imaging characteristics of isolated left ventricular noncompaction in a Chinese adult Han population. Int J Cardiovasc Imaging. 2011;27(7):979-987.
doi pubmed - Aras D, Tufekcioglu O, Ergun K, Ozeke O, Yildiz A, Topaloglu S, Deveci B, et al. Clinical features of isolated ventricular noncompaction in adults long-term clinical course, echocardiographic properties, and predictors of left ventricular failure. J Card Fail. 2006;12(9):726-733.
doi pubmed - Ricci L, Villegente J, Loyal D, Ayav C, Kivits J, Rat AC. Tailored patient therapeutic educational interventions: A patient-centred communication model. Health Expect. 2022;25(1):276-289.
doi pubmed pmc - Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, et al. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113(14):1807-1816.
doi pubmed - Soliman OI, McGhie J, Ten Cate FJ, et al. Multimodality imaging, diagnostic challenges and proposed diagnostic algorithm for noncompaction cardiomyopathy. In: Caliskan K, Soliman O, ten Cate F, editors. Noncompaction cardiomyopathy. Cham: Springer; 2019.
doi - Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, Dubourg O, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29(2):270-276.
doi pubmed - Ashwal AJ, Mugula SR, Samanth J, Paramasivam G, Nayak K, Padmakumar R. Role of deformation imaging in left ventricular non-compaction and hypertrophic cardiomyopathy: an Indian perspective. Egypt Heart J. 2020;72(1):6.
doi pubmed pmc - Bogunovic N, Farr M, Pirl L, Faber L, van Buuren F, Rudolph V, Roder F. Systolic longitudinal global and segmental myocardial mechanics in symptomatic isolated left ventricular non-compaction cardiomyopathy. Echocardiography. 2021;38(4):555-567.
doi pubmed - Szemraj-Rogucka ZM, Szemraj J, Masiarek K, Majos A. Circulating microRNAs as biomarkers for myocardial fibrosis in patients with left ventricular non-compaction cardiomyopathy. Arch Med Sci. 2019;15(2):376-384.
doi pubmed pmc - Sonaglioni A, Nicolosi GL, Rigamonti E, Lombardo M, La Sala L. Molecular approaches and echocardiographic deformation imaging in detecting myocardial fibrosis. Int J Mol Sci. 2022;23(18):10944.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


