| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Case Report
Volume 15, Number 4, August 2024, pages 314-317
Unveiling the Link: Hypocalcemia-Induced Unstable Sustained Ventricular Tachycardia in Nonischemic Cardiomyopathy
Joel Shaha, c, Kahtan Fadahb, Jan M. Lopesb, Moeen Abedinb
aDepartment of Internal Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX 79905, USA
bDepartment of Cardiology, Texas Tech University Health Sciences Center El Paso, El Paso, TX 79905, USA
cCorresponding Author: Joel Shah, Department of Internal Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX 79905, USA
Manuscript submitted June 18, 2024, accepted July 1, 2024, published online July 18, 2024
Short title: Hypocalcemia-Induced Unstable Sustained VT
doi: https://doi.org/10.14740/cr1683
| Abstract | ▴Top |
A 63-year-old female presented to a freestanding emergency room with dizziness, palpitations, and hypotension, The patient was found to have an irregular wide complex tachycardia, consistent with ventricular tachycardia, hypomagnesemia and severe hypocalcemia. The tachycardia was refractory to treatment with IV amiodarone and magnesium, and only resolved with correction of the serum calcium. Review of the medical record revealed an echocardiogram 19 years earlier reporting left ventricular dysfunction. The patient was unaware of this diagnosis and was not taking medical therapy. Echocardiogram revealed no significant change in left ventricular function, and coronary angiography showed no significant coronary artery disease. The patient’s nonischemic cardiomyopathy may have been a predisposing factor for the arrhythmia presentation. We explore a hospital admission involving the rare association of hypocalcemia and monomorphic ventricular tachycardia, which is not well documented in the literature.
Keywords: Ventricular tachycardia; Hypocalcemia; Unstable sustained monomorphic VT; Nonischemic cardiomyopathy
| Introduction | ▴Top |
Hypocalcemia, defined by total serum calcium concentration < 8.5 mg/dL or serum ionized calcium < 4.7 mg/dL [1], has well-documented effects on myocardial function, manifesting as prolonged QT intervals and altered depolarization thresholds, thereby predisposing individuals to cardiac arrhythmias such as atrioventricular (AV) blocks and ventricular tachycardia (VT) [2, 3]. Typically, repletion of the serum calcium will reverse the myocardial impairment, QT prolongation and other hypocalcemia-induced symptoms such as tetany, fatigue, muscular or abdominal cramping, and paresthesia [4].
While the existing literature mainly associates hypocalcemia with reentrant ventricular tachyarrhythmias like torsades de pointes and ventricular fibrillation, the connection between hypocalcemia and monomorphic VT, in the context of nonischemic cardiomyopathy remains an underexplored area [1, 2, 5].
We present a unique case wherein an untreated hypocalcemia-induced VT posed a significant hemodynamic challenge in a patient with previously undiagnosed nonischemic cardiomyopathy and heart failure with reduced ejection fraction (HFrEF).
| Case Report | ▴Top |
Investigations
A 63-year-old female with a medical history of hypothyroidism following thyroidectomy for a goiter at age 10, hyperlipidemia, and asthma presented to a free-standing emergency department (ED) with dizziness and palpitations that began 4 days prior. She denied shortness of breath, chest pain, syncope, or presyncope. Her past surgical history included thyroidectomy, tubal ligation, and hysterectomy. She has no known drug allergies. The patient’s family history included a father with hypertension and heart failure who died from a myocardial infarction in his 70s. She denied any alcohol, tobacco, or illicit drug use in the past. Initial blood pressure was 77/39. The patient had been taking supplemental calcium following her thyroidectomy but discontinued it approximately 3 months before presentation due to severe constipation. Electrocardiogram (ECG) revealed a wide complex tachycardia (Fig. 1). The patient declined cardioversion and was given an intravenous (IV) amiodarone bolus followed by an amiodarone drip by the ED.
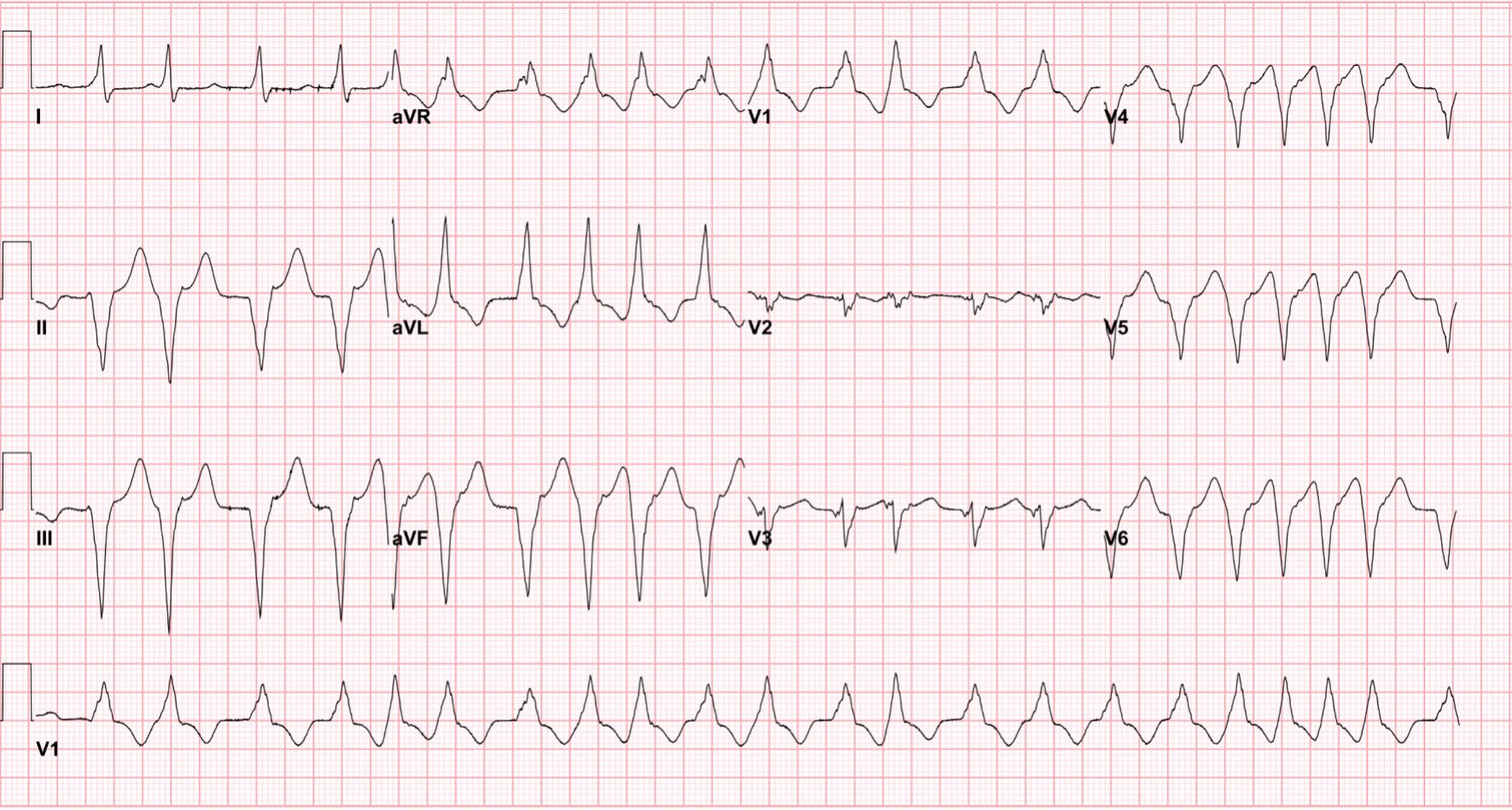 Click for large image | Figure 1. ECG on admission demonstrating wide complex sustained tachycardia with right bundle branch block and AV dissociation. ECG: electrocardiogram; RBBB: right bundle branch block. |
Subsequently, the patient was transferred to our facility, where she was hemodynamically stable with a blood pressure of 141/95 and heart rate ranging from 150 to 170 beats per minute (bpm). ECG revealed a left axis deviation, heart rate of 162, and irregular wide complex tachycardia with right bundle branch block (RBBB) concerning for ventricular tachycardia. Shortly after admission, the patient had one episode of non-bloody emesis but denied chest pain or shortness of breath. Amiodarone (360 mg (1 mg/min), IV) was continued due to a lack of labs and history including why the freestanding ED began amiodarone. Additionally, magnesium sulfate (4 mg IV) and trimethobenzamide (300 mg once, for emesis) were administered. Labs were obtained and included thyroid-stimulating hormone (TSH), parathyroid hormone (PTH), and vitamin D levels which were within normal limits; however, the patient had decreased serum magnesium and calcium levels were at 1.4 mg/dL and 6.4 mg/dL, respectively. A transthoracic echocardiogram (TTE) from 19 years prior revealed a left ventricular enlargement with ejection fraction 33% and evidence of moderate mitral and tricuspid insufficiency, but no ischemic workup was performed at that time. The patient was unaware of any heart-related diagnosis or previous echocardiogram.
Diagnosis
The initial differential diagnosis of wide complex tachycardia includes ventricular tachycardia, atrial fibrillation or supraventricular tachycardia (SVT) with aberrancy, or pre-excited tachycardia. The patient was admitted to the cardiovascular intensive care unit (CVICU) for close monitoring. She was administered magnesium (4 mg IV), and calcium gluconate (2 mg IV every hour) for electrolyte repletion and cardiac membrane stabilization, and IV amiodarone was continued at 1 mg/min for 6 h followed by 0.5 mg/min for 18 h. Sustained ventricular tachycardia continued after repletion of serum magnesium to a value of 2.0 mg/dL. Subsequent TTE revealed similar left ventricular function the previous study with left ventricular ejection fraction (LVEF) 35%. Left heart catheterization showed no obstructive coronary lesions with normal left heart filling pressures.
Treatment
After the administration of several doses of IV calcium gluconate and starting the patient on calcium carbonate (1,250 mg oral (PO), three times a day), the patient’s serum calcium level rose to 7.4 mg/dL. Once calcium improved to near normal levels, the patient’s VT terminated (Fig. 2).
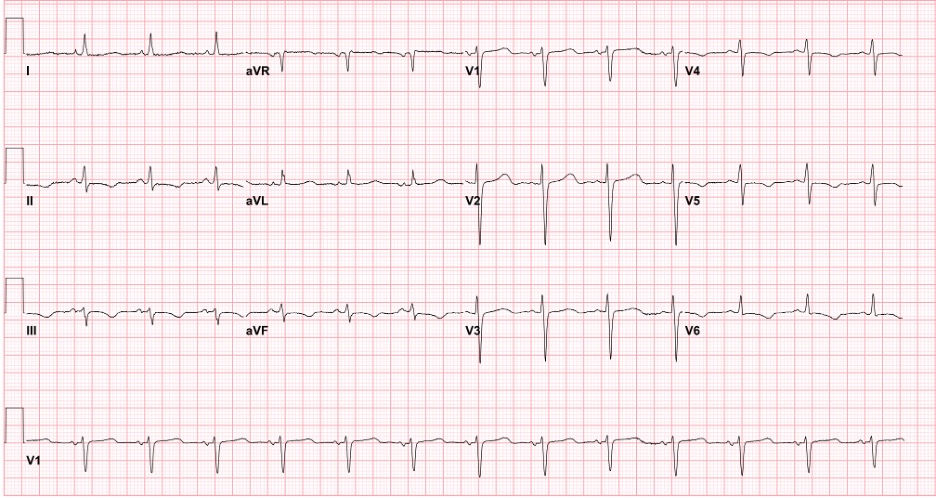 Click for large image | Figure 2. ECG after calcium supplementation. The above heart rhythm is normal sinus with nonspecific repolarization abnormalities. The burden of ventricular tachycardia has subsided. ECG: electrocardiogram. |
While the available data on the management of VT arising from electrolyte abnormalities remain limited, the medical team opted for a comprehensive approach. After 24 h, the patient was started on amiodarone (200 mg PO, once a day (qd)) and to initiate the established guideline-directed medical therapy (GDMT) for HFrEF. This included lisinopril (2.5 mg, qd), metoprolol succinate (25 mg, qd), and furosemide (20 mg, qd), along with vigilant electrolyte monitoring.
Follow-up and outcomes
By hospital day 3, the patient remained stable, with no further arrhythmias. She was hemodynamically stable, clinically euvolemic, with laboratory values well within normal limits, so she was discharged to her home. She was sent home with a wearable external defibrillator (Lifevest, Zoll, Inc., Chelmsford, MA) with a plan to reassess the left ventricular function as an outpatient in 90 days.
One month later, during a cardiology clinic follow-up, she reported being symptom-free since discharge. She continued to take GDMT, and amiodarone (200 mg PO, qd) was renewed, with plans for a gradual taper over a 9 - 12-month period depending on LVEF. The patient was also started on supplemental magnesium oxide (400 mg PO, qd) in addition to previously prescribed calcium supplement for electrolyte stability. The patient regained her daily functionality, including walking over a block without interruption, absence of chest pain, dyspnea, edema, syncope, palpitations, or life vest shocks during this time.
| Discussion | ▴Top |
In this case, a woman in her 60s presented with lightheadedness, dizziness, and palpitations, due to hypotension from a wide complex tachycardia consistent with VT. Subsequent evaluation revealed pre-existing untreated nonischemic cardiomyopathy, and laboratory tests showed mild to moderate hypomagnesemia and severe hypocalcemia secondary to hypoparathyroidism from a previous thyroidectomy. The patient notably stopped taking her calcium supplementation 3 months prior to her symptom onset due to constipation resulting in significant hypocalcemia on admission. While both hypomagnesemia and hypocalcemia are recognized triggers for ventricular arrhythmias [3, 6], the arrhythmias continued despite normalization of the serum magnesium level and treatment with IV amiodarone. The rhythm only stabilized with calcium repletion to a level above 8 mg/dL.
The association of hypocalcemia with ventricular arrhythmias, specifically torsade de pointes due to QT prolongation, has been long recognized [7]. Few cases of monomorphic VT due to hypocalcemia are reported in the medical literature. Cecchi et al [2] give one such example of symptomatic VT attributed to hypocalcemia that resolved with calcium supplementation; however, that electrolyte disturbance was due to underlying chronic kidney disease (CKD) and severe vitamin D deficiency. Chavan et al documented a case of reversible heart failure and VT secondary to hypocalcemia, in which the patient was found to have severe vitamin D deficiency and secondary hyperparathyroidism [8]. The VT was not reported as sustained or non-sustained, but the patient’s arrhythmia and heart failure resolved with calcium supplementation.
This report highlights the importance of a thorough review of a patient’s medical history. The patient had a previously untreated cardiomyopathy with LVEF 33% noted on echocardiogram performed 19 years prior. This pre-existing cardiomyopathy may have predisposed her to VT with hypocalcemia acting as the trigger after many years of decreased heart function [9]. To our knowledge, there are no published case reports identifying an underlying cardiomyopathy associated with hypocalcemia-induced sustained VT.
Further research is warranted to better understand the underlying mechanisms linking hypocalcemia and VT. Investigation of ion channel polymorphisms that may pre-dispose patients to hypocalcemia-induced ventricular arrhythmias, and possibly even concomitant cardiomyopathy would help identify specific patients at risk for hypocalcemia-induced VT. Additionally, studies focused on the optimal management strategies for VT secondary to hypocalcemia, including the role of specific antiarrhythmic agents and long-term electrolyte monitoring protocols to correctly treat the arrhythmia, would provide valuable insights into improving patient outcomes.
The limitations of this report must be considered when examining the reason for the patient’s cardioverted VT. The patient declined electrical cardioversion on her initial presentation, and it is therefore unknown if the arrhythmia would have dissipated without electrolyte repletion or antiarrhythmic drugs. However, since the VT remained paroxysmal until the calcium was repleted, it is reasonable to suspect cardioversion would not have suppressed the subsequent episodes of non-sustained VT. Additionally, hypomagnesemia is known to decrease the levels of PTH in the body and thus decrease available serum calcium [10]. Therefore, correcting the hypomagnesemia may have indirectly helped to improve the patient’s serum calcium. However, this effect was most likely insignificant when compared to direct calcium repletion with calcium gluconate and calcium carbonate.
In conclusion, unstable sustained monomorphic VT secondary to hypocalcemia is a rare but critical condition that should be promptly identified and treated in patients presenting with life-threatening ventricular arrhythmias. Untreated chronic cardiomyopathy may increase the risk for VT secondary to hypocalcemia. While the role of hypocalcemia in QT prolongation resulting in polymorphic VT (torsades de pointes) is well recognized, the potential for this electrolyte abnormality to cause monomorphic VT is not well described. Prompt recognition, correction of the underlying electrolyte abnormality, and appropriate antiarrhythmic therapy are vital in managing unstable sustained VT and preventing hemodynamic instability. Further research is needed to enhance our understanding of the association between heart failure, nonischemic cardiomyopathy, hypocalcemia, and VT and guide evidence-based management strategies.
Learning points
Unstable sustained monomorphic VT secondary to hypocalcemia is a rare phenomenon that requires prompt electrolyte repletion. Underlying cardiomyopathy may predispose individuals with electrolyte abnormalities to VT. Thorough medical history and meticulous chart review play a pivotal role in elucidating underlying factors contributing to a patient’s current clinical presentation. It is imperative not to solely depend on the patient’s recollection or recent documentation.
Acknowledgments
None to declare.
Financial Disclosure
The authors have no financial disclosure or sources of funding to disclose.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
The patient’s informed consent for publication of this case report was obtained prior to submission.
Author Contributions
Joel Shah provided the rough draft including the initial abstract, introduction, case, and conclusion. Dr. Fadah provided additional edits to each individual portion of the rough draft with key edits to the case itself including where to put the figures and how to discuss the flow of the case. Dr. Lopes and Dr. Abedin read both ECGs and provided the figure texts alongside additional edits to the case and discussion including the possibility of amiodarone prolonging the hypocalcemia-induced ventricular tachycardia. Dr. Abedin additionally acted as the senior author on the case with guidance regarding writing up the case report, additional final edits to the paper, and insight into the case itself which were utilized to create the rough draft.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Goyal A, Anastasopoulou C, Ngu M, Singh S. Hypocalcemia. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Cecchi E, Grossi F, Rossi M, Giglioli C, De Feo ML. Severe hypocalcemia and life-threatening ventricular arrhytmias: case report and proposal of a diagnostic and therapeutic algorithm. Clin Cases Miner Bone Metab. 2015;12(3):265-268.
doi pubmed pmc - Ashwin Reddy S. Ventricular arrhythmia precipitated by severe hypocalcaemia secondary to primary hypoparathyroidism. Case Rep Cardiol. 2019;2019:4851073.
doi pubmed pmc - Nijjer S, Ghosh AK, Dubrey SW. Hypocalcaemia, long QT interval and atrial arrhythmias. BMJ Case Rep. 2010;2010:bcr0820092216.
doi pubmed pmc - Foth C, Gangwani MK, Ahmed I, Alvey H. Ventricular tachycardia. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Plastiras SC, Moutsopoulos HM. Arrhythmias and conduction disturbances in autoimmune rheumatic disorders. Arrhythm Electrophysiol Rev. 2021;10(1):17-25.
doi pubmed pmc - Behere SP, Weindling SN. Inherited arrhythmias: The cardiac channelopathies. Ann Pediatr Cardiol. 2015;8(3):210-220.
doi pubmed pmc - Chavan CB, Sharada K, Rao HB, Narsimhan C. Hypocalcemia as a cause of reversible cardiomyopathy with ventricular tachycardia. Ann Intern Med. 2007;146(7):541-542.
doi pubmed - Chung FP, Lin CY, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, et al. Ventricular arrhythmias in nonischemic cardiomyopathy. J Arrhythm. 2018;34(4):336-346.
doi pubmed pmc - Gragossian A, Bashir K, Bhutta BS, Friede R. Hypomagnesemia. In: StatPearls. Treasure Island (FL). 2024.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


