| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 7, Number 1, February 2016, pages 36-45
Management of Atrio-Esophageal Fistula Following Left Atrial Ablation
Tariq Yousufa, e, Hesam Keshmiria, Zachary Bulwab, Jason Kramerb, Hafiz Muhammad Sharjeel Arshada, Rasha Issaa, Daniel Woznickaa, Paul Gordonc, Pierre Abi-Mansourd
aDepartment of Internal Medicine, Advocate Christ Medical Center, 105 Covington Ct, Oak Brook, IL 60523, USA
bRosalind Franklin University of Medicine and Science, North Chicago, IL, USA
cDepartment of Cardiovascular Surgery, Advocate Christ Medical Center, Oak Lawn, IL, USA
dDepartment of Cardiology, Advocate Christ Medical Center, Oak Lawn, IL, USA
eCorresponding Author: Tariq Yousuf, Department of Internal Medicine, Advocate Christ Medical Center, 105 Covington Ct, Oak Brook, IL 6052, USA
Manuscript accepted for publication December 23, 2015
Short title: Atrio-Esophageal Fistula
doi: http://dx.doi.org/10.14740/cr454e
| Abstract | ▴Top |
Currently, no guidelines have been established for the treatment of atrio-esophageal fistula (AEF) secondary to left atrial ablation therapy. After comprehensive literature review, we aim to make suggestions on the management of this complex complication and also present a case series. We performed a review of the existing literature on AEF in the setting of atrial ablation. Using keywords atrial fibrillation, atrial ablation, fistula formation, atrio-esophageal fistula, complications, interventions, and prognosis, a search was made using the medical databases PUBMED and MEDLINE for reports in English from 2000 to April 2015. A statistical analysis was performed to compare the three different intervention arms: medical management, stent placement and surgical intervention. The results of our systematic review confirm the high mortality rate associated with AEF following left atrial ablation and the necessity to diagnose atrio-esophageal injury in a timely manner. The mortality rates of this complication are 96% with medical management alone, 100% with stent placement, and 33 % with surgical intervention. Atrio-esophageal injury and subsequent AEF is an infrequent but potentially fatal complication of atrial ablation. Early, prompt, and definitive surgical intervention is the treatment of choice.
Keywords: Atrial ablation; Atrial fibrillation; Arrhythmia; Atrio-esophageal fistula
| Introduction | ▴Top |
Treatment of atrial fibrillation (AF) consists of heart rate control, rhythm control, and anticoagulation. Left atrial catheter ablation with either cryotherapy or radiofrequency is now accepted as a treatment for symptomatic drug-refractory AF. With an increase in left atrial ablation procedures, there has also been a concomitant rise in post-procedural complications.
We present a review of the previous literature that demonstrates the dire complication of atrio-esophageal fistula (AEF), which is defined as an abnormal connection between the esophagus and atrium of the heart following left atrial ablation.
| Case Reports | ▴Top |
Case 1
A 77-year-old female with a past medical history of paroxysmal AF of 8 years duration presented to the hospital with worsening symptoms of palpitations and shortness of breath over the past 6 months. Over the previous 3 months, she had uncontrolled symptomatic arrhythmias despite being on dronedarone, which was then switched to amiodarone. After the switch, she suffered from additional symptoms including fatigue, constipation, loss of appetite, and dry cough. She underwent left atrial cryotherapy ablation for treatment of AF. On post-operative day 1, she complained of dysphagia, which resolved using empiric medical therapy with pantoprazole and sucralfate.
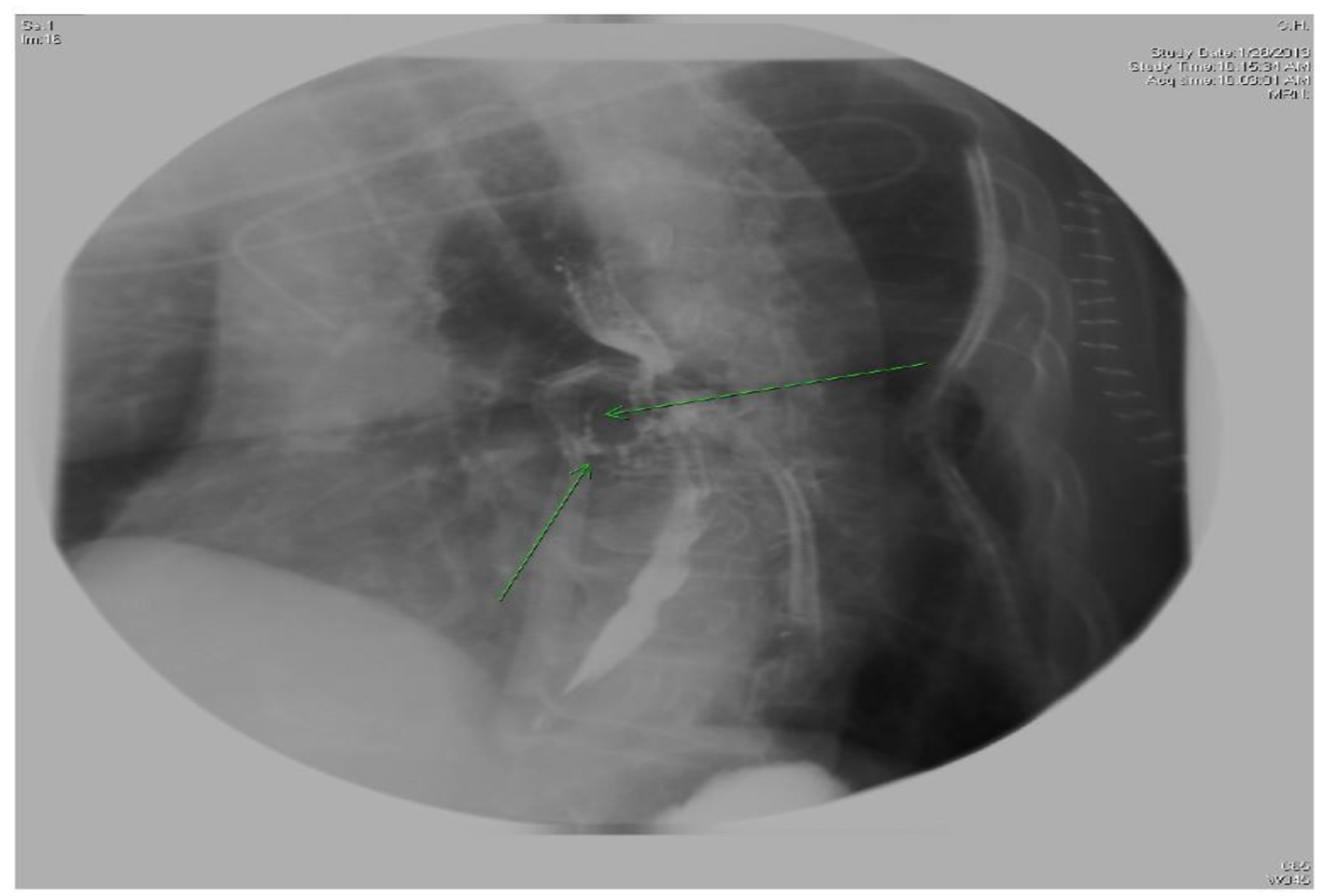
Twenty days after the ablation, the patient was re-admitted with fever, chills, and difficulty swallowing. An esophagram with gastrografin demonstrated a contrast leak anterior to the esophagus at the level of the left atrium but without an obvious connection (Fig. 1). She developed new-onset weakness in her left extremities. Computed tomography angiography (CTA) revealed multifocal emboli. A transthoracic echocardiogram (TTE) did not show any evidence of a clot in the atrium. With a high suspicion for an AEF, a thoracic CT was performed and confirmed a fistulous tract between the esophagus and left atrium.
 Click for large image | Figure 1. X-ray esophagus with gastrografin showing sinus tracts extending from anterior aspect of esophagus. |
A left posterior lateral thoracotomy was performed for surgical repair of the existing fistula. Post-operatively, repeat esophagram with gastrografin was ordered and demonstrated additional sinus tracts extending from the thoracic segment of the esophagus to the left atrium (Fig. 2). Due to the persistent fistula, the patient underwent another surgery. The patient was not sent home on oral anticoagulation therapy. Two weeks following the second surgery, the patient had several bouts of intractable coughing. An esophagram after this episode re-demonstrated a fistulous tract. Despite heroic measures, the patient’s condition deteriorated and she ultimately expired 3 days later secondary to septic shock.
 Click for large image | Figure 2. X-ray esophagus with gastrografin showing two sinus tracts extending from anterior aspect of esophagus at level T7. |
Case 2
A 64-year-old male underwent cryoablation of all four pulmonary veins for symptomatic drug refractory AF and was discharged home the same day on rivaroxaban and amiodarone for 3 months as well as an event monitor for 3 weeks. Later that night, the patient developed pleuritic chest pain. He was found to be in atrial flutter in the emergency department. A CTA of the chest and abdomen identified esophageal perforation with a fistulous tract to the left atrium (Fig. 3). Echocardiogram at this time showed a moderate to large pericardial effusion with no evidence of hemodynamic compromise.
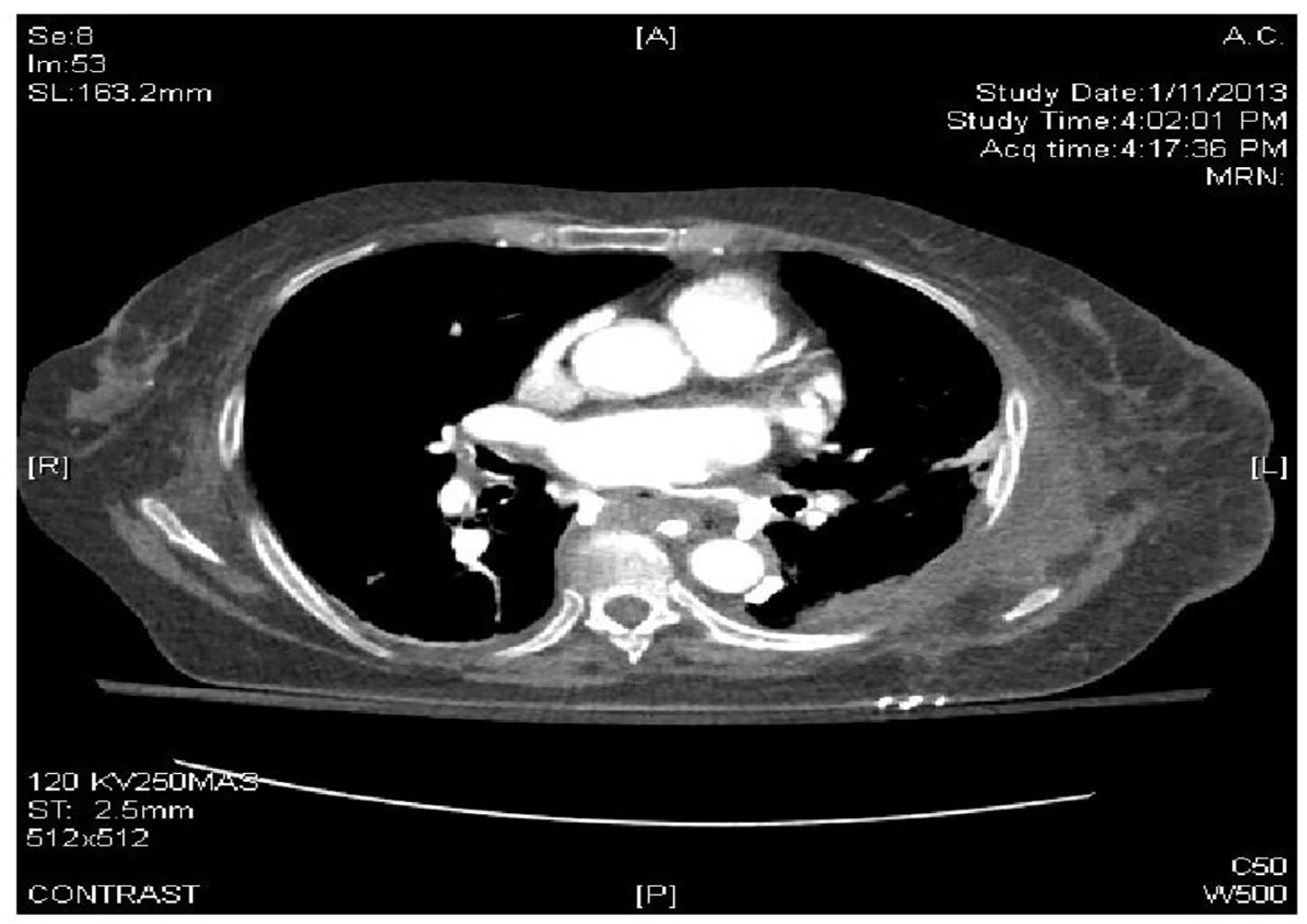 Click for large image | Figure 3. CTA of the chest and abdomen identified esophageal perforation with a fistulous tract to the left atrium. |
Median sternotomy was performed 5 days post-ablation in order to drain the pericardial effusion of purulent fluid. An esophageal stent was also placed for the treatment of an AEF. Pericardial fluid cultures grew group A Streptococcus and the patient was started on antibiotics. Although he improved clinically, an esophagram revealed a persistent AEF (Fig. 4). The patient was sent to a rehabilitation facility.
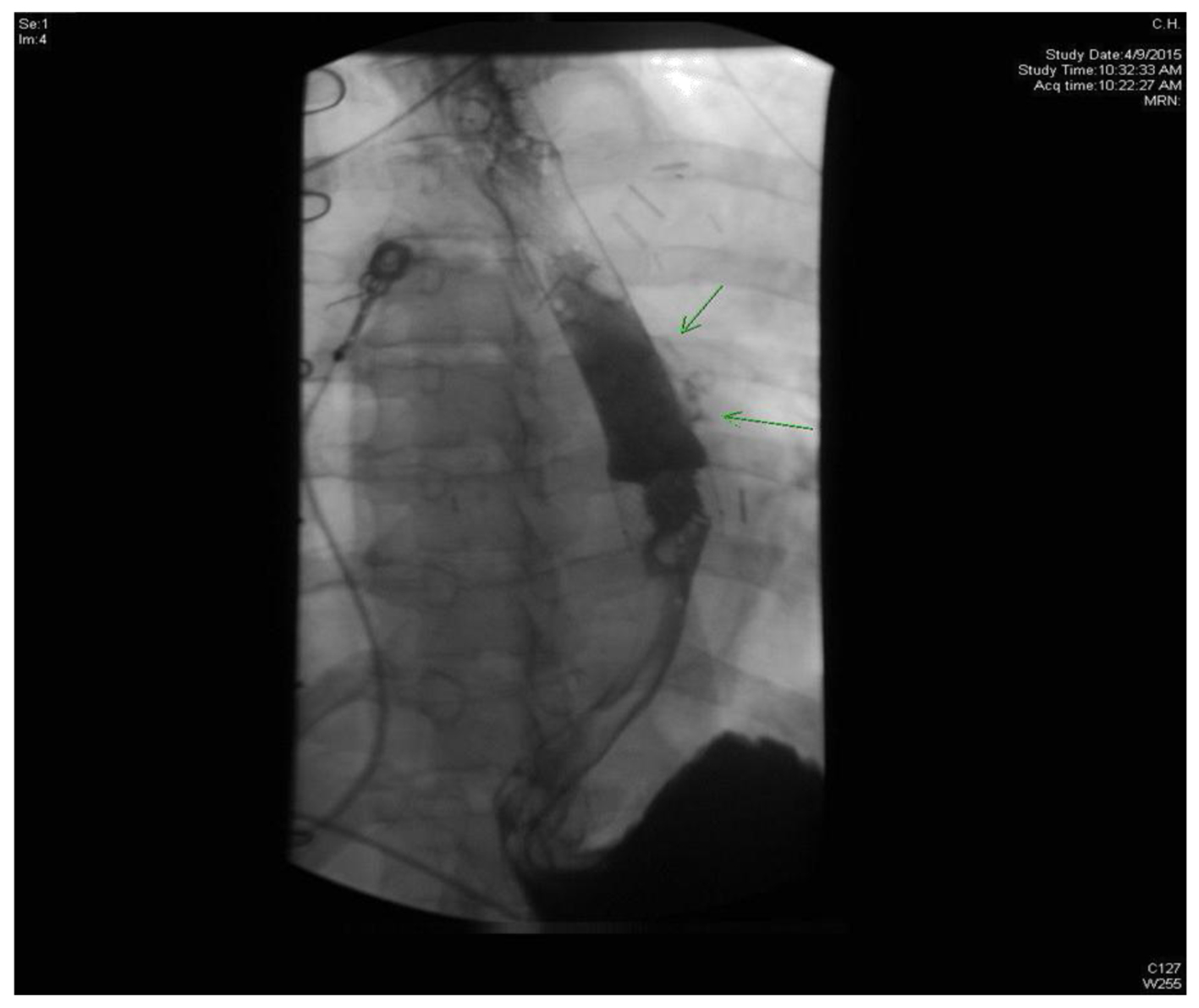 Click for large image | Figure 4. Esophagogram showing extravasation of contrast from posterolateral aspect of esophagus. |
The patient was hospitalized and found to have intermittent febrile episodes with hypotension and three transient episodes of left-sided weakness. The patient was in AF with rapid response; therefore, he was maintained on amiodarone and a heparin drip.
A TTE demonstrated a mobile echogenic structure within the left atrium consistent with a thrombus. He underwent sternotomy with removal of the left atrial thrombus and closure of a patent foramen ovale. The patient was transferred to our facility to undergo repair of the newly demonstrated AEF. Figure 5 demonstrates the 2-cm defect in the esophagus (Fig. 5). It was accomplished with surgery consisting of an autologous pericardial patch with suture repair of the esophageal defect and latissimus dorsi muscle interposition flap placement (Fig. 6). The esophagus was circumferentially wrapped with the latissimus flap. The esophageal stent was also removed. He tolerated the surgery well. Heparin drip was started immediately post-operatively. The patient was discharged to a rehabilitation facility. Patient was followed up several months afterwards and has continued to do well post-operatively.
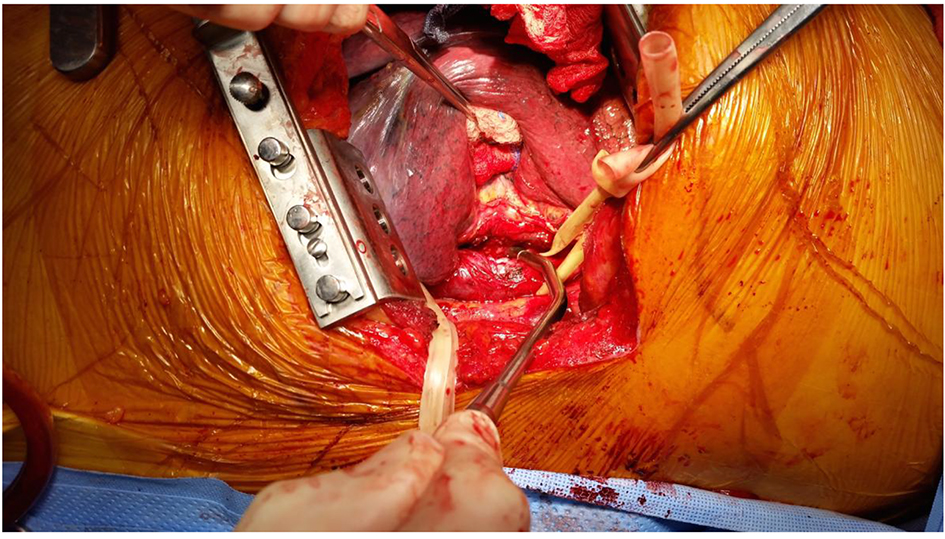 Click for large image | Figure 5. Two-centimeter defect in the esophagus. |
 Click for large image | Figure 6. Esophagus wrapped circumferentially with latissimus flap. |
Discussion
The indications and application of left atrial ablation in the treatment of AF have progressively expanded in the past decade [1, 2]. A single ablation procedure was successful in 50% of patients and additional ablation procedures increased long-term freedom from AF to 80% [3]. Nevertheless, complication rates following ablation have mounted with rates varying amongst studies from 0.8% to 6% [1, 4]. When patients consent to catheter ablation, they must understand the risks associated with the procedure. Major complications include cardiac tamponade (1.31%), thromboembolic events (stroke 0.23%, transient ischemic attacks 0.71%), pulmonary vein stenosis (0.29% requiring dilation), esophageal injury (AEF 0.04%), and death (0.15%) [1, 4]. Esophageal injury can vary greatly from one patient to the next. The spectrum of injury ranges from esophageal erythema, ulcer-like changes in the esophageal wall, peri-esophageal nerve injury, esophageal perforation, and the development of an AEF.
Although AEF is a rare complication, it carries a higher rate of morbidity and mortality compared to all other complications related to AF catheter ablation [1]. Due to its anatomic location relative to the posterior left atrium (0.9 ± 0.2 mm) [4], the anterior esophagus is particularly prone to surgical injury [5]. Esophageal complications have been reported in up to 47% of patients who underwent catheter ablation [4]. The most notorious and fatal of these esophageal complications is AEF. Table 1 [6-48] provides a comprehensive summary of all documented cases of AEF (Table 1).
 Click to view | Table 1. Descriptions of Published Case Reports and Case Series With AEF After Ablation for Atrial Fibrillation |
Prompt diagnosis of AEF is paramount as emergent intervention is required [49]. The clinical presentation of AEF includes but is not limited to fever, chest pain, dysphagia, melena, hematemesis, and sepsis. AEF usually presents between 3 days and 5 weeks post-ablation [50]. Many patients with AEF present with neurological manifestations including stroke, TIA, seizures, and meningitis [49, 50]. The AEF can act as a single-way valve for air and emboli leading to neurologic manifestations [50]. Diagnosis requires high clinical suspicion for AEF and knowledge of the complications of catheter ablation. If AEF is suspected, water-soluble contrast esophagram may illustrate a fistulous tract. In addition, X-ray or CT of the chest may aid in identifying pneumopericardium and pneumomediastinum.
Relative contraindications exist for upper endoscopy and TEE in order to limit food and air embolism, enlargement of the fistula, and further esophageal damage [50, 51]. Furthermore, oral intake should be avoided to prevent postprandial food embolism. In order to prevent AEF formation, several protective measures have been suggested. These include gastric acid suppression, esophageal temperature monitoring, mechanical deflection of the esophagus, and thermal insulation of the esophagus [10].
Although there are no current guideline recommendations about treatment with stents or surgical fistula takedown [2], our review indicates a dramatic response to definitive surgical intervention, which shows a decreased mortality rate from 100% to 32.4% (Table 2).
 Click to view | Table 2. Summary Table |
In a non-randomized control trial, stenting alone was initially chosen because it is less invasive [5]. Due to poor outcomes, the remaining patients were treated with surgical intervention, which showed a significant improvement in mortality. From review of the literature, patients who received stent placement alone had significantly higher mortality because stents cannot prevent embolic events with an established AEF [52]. Ellis et al demonstrated stenting as a preventative measure post-esophageal injury without AEF [10].
The question will arise regarding the unstable patient with AEF. Conventional standards suggest that surgery may be associated with higher risks. However, our review of the literature shows that most patients with AEF who received stent placement or medical therapy alone without surgical intervention will die. Therefore, we believe that even the unstable patient should be taken to the operating room in a timely manner. Stenting may be used as a temporary bridge to surgical intervention but is by no means a definitive therapy. Maintenance of anticoagulation is recommended due to high risk of left atrial thrombus formation and high incidence of cardio-embolic events. Early initiation of anticoagulation after surgical repair may decrease the incidence of post-repair stroke.
A multicenter prospective study may be warranted to further validate our conclusions. This would help elucidate any biases of patient population, physician preference, and operator proficiency.
Conclusion
Esophageal injury and subsequent fistula formation are among the most frequent and fatal complications of left atrial ablation therapy for symptomatic AF. Screening for patients at increased risk as well as peri-procedural attempts at minimizing the risk of esophageal injury needs to be pursued. Ultimately, survival after post-ablative esophageal injury is likely correlated to high diagnostic suspicion for such injury, prompt diagnosis, and urgent surgical intervention rather than stent placement or medical management for this dreaded complication.
Conflict of Interest
No authors involved in this project have any disclosures to report.
Source of Funding
None.
| References | ▴Top |
- Sorgente A, Chierchia GB, de Asmundis C, Sarkozy A, Capulzini L, Brugada P. Complications of atrial fibrillation ablation: when prevention is better than cure. Europace. 2011;13(11):1526-1532.
doi pubmed - Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(1):32-38.
doi pubmed - Ganesan AN, Shipp NJ, Brooks AG, Kuklik P, Lau DH, Lim HS, Sullivan T, et al. Long-term outcomes of catheter ablation of atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(2):e004549.
doi pubmed - Qumseya BJ, Kusumoto F, Wolfsen H. Esophageal injury following left atrial ablation. Gastroenterol Hepatol (N Y). 2012;8(6):414-416.
- Eitel C, Rolf S, Zachaus M, John S, Sommer P, Bollmann A, Arya A, et al. Successful nonsurgical treatment of esophagopericardial fistulas after atrial fibrillation catheter ablation: a case series. Circ Arrhythm Electrophysiol. 2013;6(4):675-681.
doi pubmed - Mohr FW, Fabricius AM, Falk V, Autschbach R, Doll N, Von Oppell U, Diegeler A, et al. Curative treatment of atrial fibrillation with intraoperative radiofrequency ablation: short-term and midterm results. J Thorac Cardiovasc Surg. 2002;123(5):919-927.
doi pubmed - Kottkamp H, Hindricks G, Autschbach R, Krauss B, Strasser B, Schirdewahn P, Fabricius A, et al. Specific linear left atrial lesions in atrial fibrillation: intraoperative radiofrequency ablation using minimally invasive surgical techniques. J Am Coll Cardiol. 2002;40(3):475-480.
doi - Doll N, Borger MA, Fabricius A, Stephan S, Gummert J, Mohr FW, Hauss J, et al. Esophageal perforation during left atrial radiofrequency ablation: Is the risk too high? J Thorac Cardiovasc Surg. 2003;125(4):836-842.
doi pubmed - Sonmez B, Demirsoy E, Yagan N, Unal M, Arbatli H, Sener D, Baran T, et al. A fatal complication due to radiofrequency ablation for atrial fibrillation: atrio-esophageal fistula. Ann Thorac Surg. 2003;76(1):281-283.
doi - Pappone C, Oral H, Santinelli V, Vicedomini G, Lang CC, Manguso F, Torracca L, et al. Atrio-esophageal fistula as a complication of percutaneous transcatheter ablation of atrial fibrillation. Circulation. 2004;109(22):2724-2726.
doi pubmed - Scanavacca MI, D'Avila A, Parga J, Sosa E. Left atrial-esophageal fistula following radiofrequency catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2004;15(8):960-962.
doi pubmed - Dagres N, Kottkamp H, Piorkowski C, Doll N, Mohr F, Horlitz M, Kremastinos DT, et al. Rapid detection and successful treatment of esophageal perforation after radiofrequency ablation of atrial fibrillation: lessons from five cases. J Cardiovasc Electrophysiol. 2006;17(11):1213-1215.
doi pubmed - Schley P, Gulker H, Horlitz M. Atrio-oesophageal fistula following circumferential pulmonary vein ablation: verification of diagnosis with multislice computed tomography. Europace. 2006;8(3):189-190.
doi pubmed - Cummings JE, Schweikert RA, Saliba WI, Burkhardt JD, Kilikaslan F, Saad E, Natale A. Brief communication: atrial-esophageal fistulas after radiofrequency ablation. Ann Intern Med. 2006;144(8):572-574.
doi pubmed - Gerstenfeld EP, Callans D, Dixit S, Lin D, Cooper J, Russo AM, Verdino R, et al. Characteristics of patients undergoing atrial fibrillation ablation: trends over a seven-year period 1999-2005. J Cardiovasc Electrophysiol. 2007;18(1):23-28.
doi pubmed - Malamis AP, Kirshenbaum KJ, Nadimpalli S. CT radiographic findings: atrio-esophageal fistula after transcatheter percutaneous ablation of atrial fibrillation. J Thorac Imaging. 2007;22(2):188-191.
doi pubmed - Preis O, Digumarthy SR, Wright CD, Shepard JA. Atrioesophageal fistula after catheter pulmonary venous ablation for atrial fibrillation: imaging features. J Thorac Imaging. 2007;22(3):283-285.
doi pubmed - Dixit S, Gerstenfeld EP, Ratcliffe SJ, Cooper JM, Russo AM, Kimmel SE, Callans DJ, et al. Single procedure efficacy of isolating all versus arrhythmogenic pulmonary veins on long-term control of atrial fibrillation: a prospective randomized study. Heart Rhythm. 2008;5(2):174-181.
doi pubmed - Borchert B, Lawrenz T, Hansky B, Stellbrink C. Lethal atrioesophageal fistula after pulmonary vein isolation using high-intensity focused ultrasound (HIFU). Heart Rhythm. 2008;5(1):145-148.
doi pubmed - Ouchikhe A, Maindivide J, Le Bivic JL, Roux L, Vincent JF. [Atrio-oesophageal fistula after radiofrequency ablation: predominant neurological symptoms]. Ann Fr Anesth Reanim. 2008;27(6):499-501.
doi pubmed - Hazell W, Heaven D, Kazemi A, Fourie D. Atrio-oesophageal fistula: an emergent complication of radiofrequency ablation. Emerg Med Australas. 2009;21(4):329-332.
doi pubmed - Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, et al. Prevalence and causes of fatal outcome in catheter ablation of atrial fibrillation. J Am Coll Cardiol. 2009;53(19):1798-1803.
doi pubmed - Ghia KK, Chugh A, Good E, Pelosi F, Jongnarangsin K, Bogun F, Morady F, et al. A nationwide survey on the prevalence of atrioesophageal fistula after left atrial radiofrequency catheter ablation. J Interv Card Electrophysiol. 2009;24(1):33-36.
doi pubmed - Khandhar S, Nitzschke S, Ad N. Left atrioesophageal fistula following catheter ablation for atrial fibrillation: off-bypass, primary repair using an extrapericardial approach. J Thorac Cardiovasc Surg. 2010;139(2):507-509.
doi pubmed - Gilcrease GW, Stein JB. A delayed case of fatal atrioesophageal fistula following radiofrequency ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2010;21(6):708-711.
doi pubmed - Baker MJ, Panchal PC, Allenby PA. Life-threatening GI hemorrhage caused by atrioesophageal fistula: a rare complication after catheter ablation for atrial fibrillation. Gastrointest Endosc. 2010;72(4):887-889.
doi pubmed - Cazavet A, Muscari F, Marachet MA, Leobon B. Successful surgery for atrioesophageal fistula caused by transcatheter ablation of atrial fibrillation. J Thorac Cardiovasc Surg. 2010;140(3):e43-45.
doi pubmed - Neven K, Schmidt B, Metzner A, Otomo K, Nuyens D, De Potter T, Chun KR, et al. Fatal end of a safety algorithm for pulmonary vein isolation with use of high-intensity focused ultrasound. Circ Arrhythm Electrophysiol. 2010;3(3):260-265.
doi pubmed - Siegel MO, Parenti DM, Simon GL. Atrial-esophageal fistula after atrial radiofrequency catheter ablation. Clin Infect Dis. 2010;51(1):73-76.
doi pubmed - Zellerhoff S, Lenze F, Schulz R, Eckardt L. Fatal course of esophageal stenting of an atrioesophageal fistula after atrial fibrillation ablation. Heart Rhythm. 2011;8(4):624-626.
doi pubmed - St Julien J, Putnam JB, Jr., Nesbitt JC, Lambright ES, Petracek MR, Grogan EL. Successful treatment of atrioesophageal fistula by cervical esophageal ligation and decompression. Ann Thorac Surg. 2011;91(6):e85-86.
doi pubmed - Tancevski I, Hintringer F, Stuehlinger M, Gassner EM, Bonaros N, Mueller LC, Mair J. Atrioesophageal fistula after percutaneous transcatheter ablation of atrial fibrillation. Circulation. 2012;125(7):966.
doi pubmed - Haggerty KA, George TJ, Arnaoutakis GJ, Barreiro CJ, Shah AS, Sussman MS. Successful repair of an atrioesophageal fistula after catheter ablation for atrial fibrillation. Ann Thorac Surg. 2012;93(1):313-315.
doi pubmed - Hartman AR, Glassman L, Katz S, Chinitz L, Ross W. Surgical repair of a left atrial-esophageal fistula after radiofrequency catheter ablation for atrial fibrillation. Ann Thorac Surg. 2012;94(4):e91-93.
doi pubmed - Stockigt F, Schrickel JW, Andrie R, Lickfett L. Atrioesophageal fistula after cryoballoon pulmonary vein isolation. J Cardiovasc Electrophysiol. 2012;23(11):1254-1257.
doi pubmed - Tan C, Coffey A. Atrioesophageal fistula after surgical unipolar radiofrequency atrial ablation for atrial fibrillation. Ann Thorac Surg. 2013;95(3):e61-62.
doi pubmed - Rivera GA, David IB, Anand RG. Successful atrioesophageal fistula repair after atrial fibrillation ablation. J Am Coll Cardiol. 2013;61(11):1204.
doi pubmed - Aryana A, Arthur A, O'Neill PG, D'Avila A. Catastrophic manifestations of air embolism in a patient with atrioesophageal fistula following minimally invasive surgical ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24(8):933-934.
doi pubmed - Shim CY, Lee SY, Pak HN. Coronary air embolism associated with atrioesophageal fistula after ablation of atrial fibrillation. Can J Cardiol. 2013;29(10):Pages 1329 e1317-1329 e1319.
- Mohanty S. Outcomes of atrio-esophageal fistula following catheter ablation of atrial fibrillation treated with surgical repair versus esophageal stenting. J Cardiovasc Electrophysiol. 2014;25(9):E6.
doi pubmed - Rajapaksha WR, Cunningham KS, Rose TH. A fatal case of atrioesophageal fistula following radiofrequency ablation of left atrium and pulmonary veins for atrial fibrillation. Cardiovasc Pathol. 2014;23(4):238-240.
doi pubmed - Vilades Medel D, Marti-Almor J, Montiel Serrano J, Sionis A, Leta Petracca R. Atrioesophageal fistula secondary to pulmonary vein cryo-ablation. Eur Heart J Cardiovasc Imaging. 2014;15(1):116.
doi pubmed - Lim HW, Cogert GA, Cameron CS, Cheng VY, Sandler DA. Atrioesophageal fistula during cryoballoon ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2014;25(2):208-213.
doi pubmed - Shiraishi M, Morita H, Muramatsu K, Sato A, Nitta J, Yamaguchi A, Adachi H. Successful non-operative management of left atrioesophageal fistula following catheter ablation. Surg Today. 2014;44(8):1565-1568.
doi pubmed - Kawasaki R, Gauri A, Elmouchi D, Duggal M, Bhan A. Atrioesophageal fistula complicating cryoballoon pulmonary vein isolation for paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2014;25(7):787-792.
doi pubmed - Schouver ED, Moceri P, Chiche O, Havet J, Lanfranchi P, Ferrari E. Multiple organ dysfunction syndrome 2 weeks after radiofrequency ablation of atrial fibrillation. Int J Cardiol. 2014;174(3):760-761.
doi pubmed - Koa-Wing M, Jamil-Copley S, Ariff B, Kojodjojo P, Lim PB, Whinnett Z, Rajakulendran S, et al. Haemorrhagic cerebral air embolism from an atrio-oesophageal fistula following atrial fibrillation ablation. Perfusion. 2015;30(6):484-486.
doi pubmed - Hirji SA, Haney JC, Welsby I, Lombard FW, Berry MF. Hyperbaric oxygen therapy for treatment of neurologic sequela after atrioesophageal fistula. Ann Thorac Surg. 2015;99(2):681-682.
doi pubmed - Keshishian J, Young J, Hill E, Saloum Y, Brady PG. Esophageal injury following radiofrequency ablation for atrial fibrillation: injury classification. Gastroenterol Hepatol (N Y). 2012;8(6):411-414.
- Mohanty S, Santangeli P, Mohanty P, Di Biase L, Trivedi C, Bai R, Horton R, et al. Outcomes of atrioesophageal fistula following catheter ablation of atrial fibrillation treated with surgical repair versus esophageal stenting. J Cardiovasc Electrophysiol. 2014;25(6):579-584.
doi pubmed - Stollberger C, Pulgram T, Finsterer J. Neurological consequences of atrioesophageal fistula after radiofrequency ablation in atrial fibrillation. Arch Neurol. 2009;66(7):884-887.
doi pubmed - Ellis CR, Streur M, Scharf AW, Nesbitt JC. Successful treatment of esophageal perforation following atrial fibrillation ablation with a fully covered esophageal stent: Prevention of atrial-esophageal fistula. J In- nov Cardiac Rhythm Management. 2012;3:874-878.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


