| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 8, Number 5, October 2017, pages 232-235
Polymorphic Ventricular Tachycardia Secondary to Subarachnoid Haemorrhage: A Rare Occurrence in the Setting of Normal QTc
Siddharth Paresh Shaha, e, Priyanka Pitrodab, Kinner Patelc, Rahul Chandakd, Timothy Fordb
aDepartment of Medicine, SUNY Upstate Medical University, 50 Presidential Plaza, Apt#1505, Syracuse, NY 13202, USA
bDepartment of Cardiovascular Medicine, SUNY Upstate Medical University, 750 East Adams Street, Syracuse, NY 13210, USA
cDepartment of Medicine, SUNY Upstate Medical University, 750 East Adams Street, Syracuse, NY 13210, USA
dSUNY Upstate Medical University, 750 East Adams Street, Syracuse, NY 13210, USA
eCorresponding Author: Siddharth Paresh Shah, Department of Medicine, SUNY Upstate Medical University, 50 Presidential Plaza, Apt#1505, Syracuse, NY 13202, USA
Manuscript submitted July 9, 2017, accepted August 15, 2017
Short title: VT Secondary to SAH
doi: https://doi.org/10.14740/cr574w
| Abstract | ▴Top |
Subarachnoid hemorrhage (SAH) is a neurologic emergency associated with high mortality rate. Polymorphic ventricular tachycardia (VT) is a rare arrhythmia. It can occur in any setting of a long QT interval and bradycardia. This may result from a cardiomyopathy (both ischemic and non-ischemic), acute coronary ischemia, congenital long QT syndrome, electrolyte disturbances and cerebrovascular diseases. We report a rare case of polymorphic VT of unclear etiology with a normal corrected QT, likely secondary to SAH. Reports associating ventricular arrhythmias and SAH have been described, yet the mechanism of this association remains unclear. Previous observations of VT seen in patients with SAH suggest a relationship with QT prolongation. The QT interval, however, remained normal in our patient, suggesting an alternative and unknown mechanism for the polymorphic VT.
Keywords: Polymorphic ventricular tachycardia; Subarachnoid hemorrhage; Normal QTc
| Introduction | ▴Top |
Subarachnoid hemorrhage (SAH) is a neurologic emergency associated with high mortality rate. Causes include traumatic brain injury, rupture of aneurysm and arteriovenous malformation. Polymorphic ventricular tachycardia (VT) is a rare arrhythmia. It can occur in any setting of a long QT interval and bradycardia. This may result from a cardiomyopathy (both ischemic and non-ischemic), acute coronary ischemia, congenital long QT syndrome, electrolyte disturbances and cerebrovascular diseases. We report a rare case of polymorphic VT of unclear etiology with a normal corrected QT, likely secondary to SAH.
| Case Report | ▴Top |
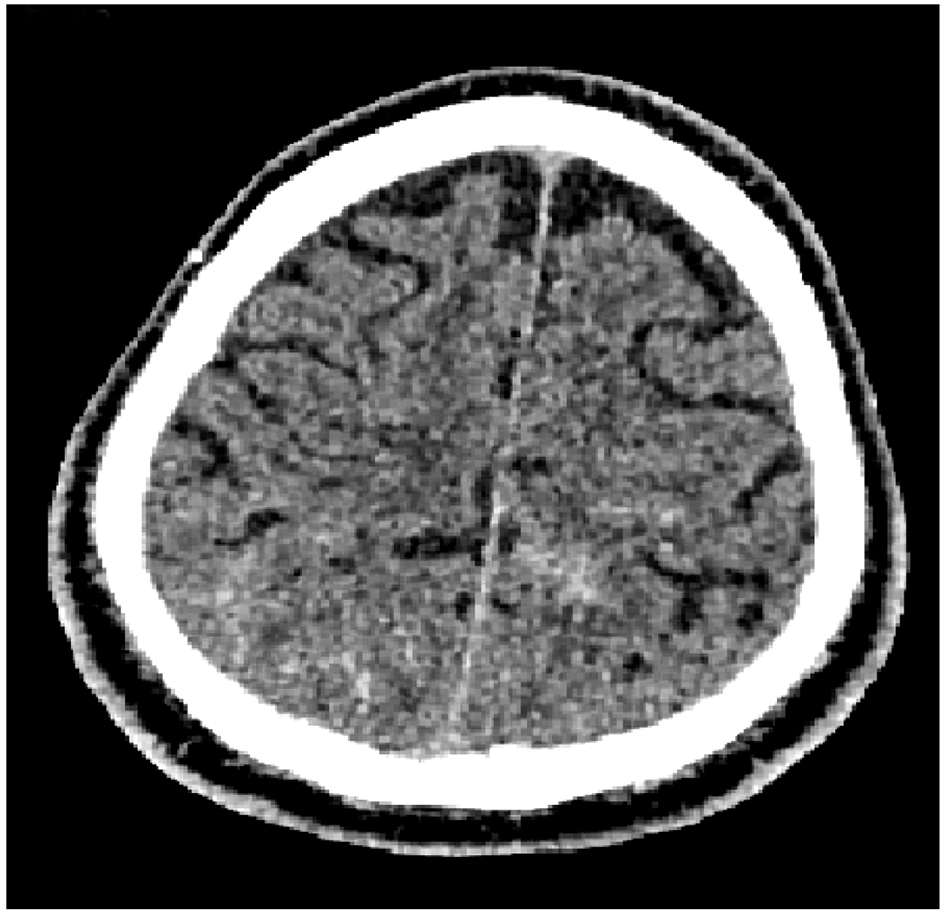
A 71-year-old man with no known past medical history presented to the emergency department (ED) after he was found down by bystanders. The patient was disoriented and extremely agitated. He was intubated for acute respiratory failure secondary to acute encephalopathy. Vitals were within normal limits. Physical examination was unremarkable for the cardiovascular, respiratory and gastrointestinal systems. Neurologic exam was limited but no focal neurologic signs were noted except for positive Babinski’s reflex bilaterally. CBC and BMP were unremarkable except for platelets of 97,000/µL. Baseline electrocardiogram (EKG) from admission revealed normal sinus rhythm with PVCs, non-specific T wave abnormality, QT interval of 432 ms and QTc of 464 ms by Framingham criteria (Fig. 1). Chest X-ray was unremarkable (Fig. 2). Computed tomography (CT) of the head revealed diffuse bilateral SAH, more pronounced in the frontal, parietal and temporal regions (Figs. 3-5). There were also small areas of intraparenchymal hemorrhage in the bilateral frontal and temporal lobes. CT angiogram of the head and neck did not reveal any anomalies in the vasculature. No acute neurosurgical intervention was deemed necessary.
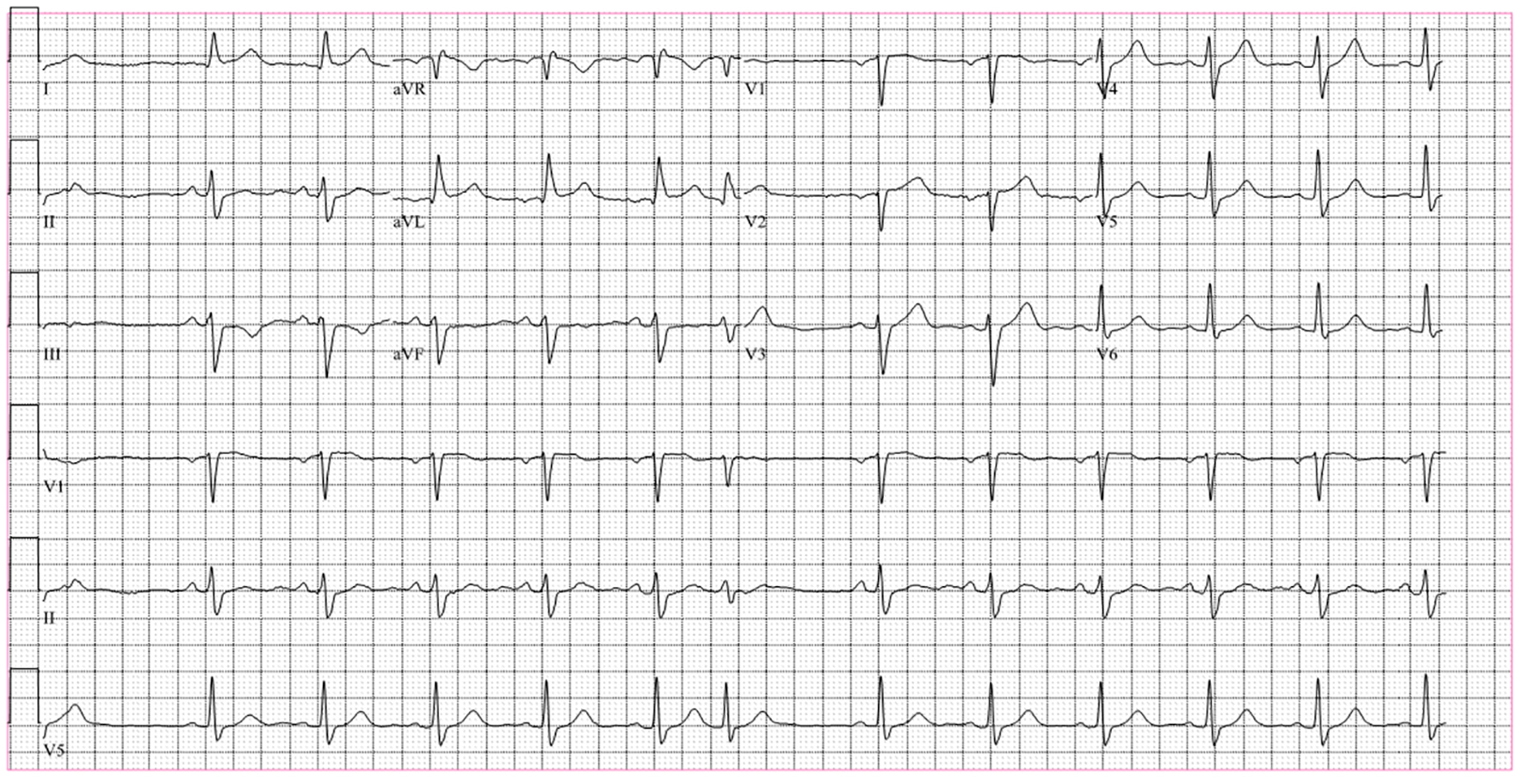 Click for large image | Figure 1. Baseline EKG on admission shows normal sinus rhythm with few premature ventricular contractions. QT interval is 432 ms and corrected QT is 464 ms. |
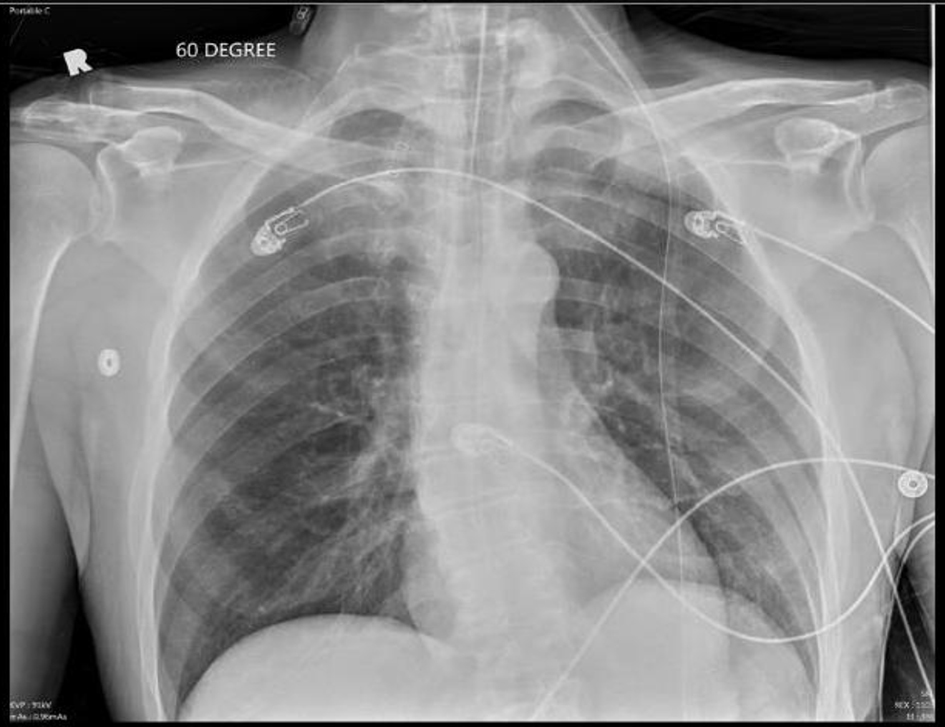 Click for large image | Figure 2. Chest X-ray (AP view) perfromed following the endotracheal intubation in this patient on admission shows the satisfactory position of the endotracheal tube. The lungs are clear with no clear infiltrates or any evidence of pneumothorax. |
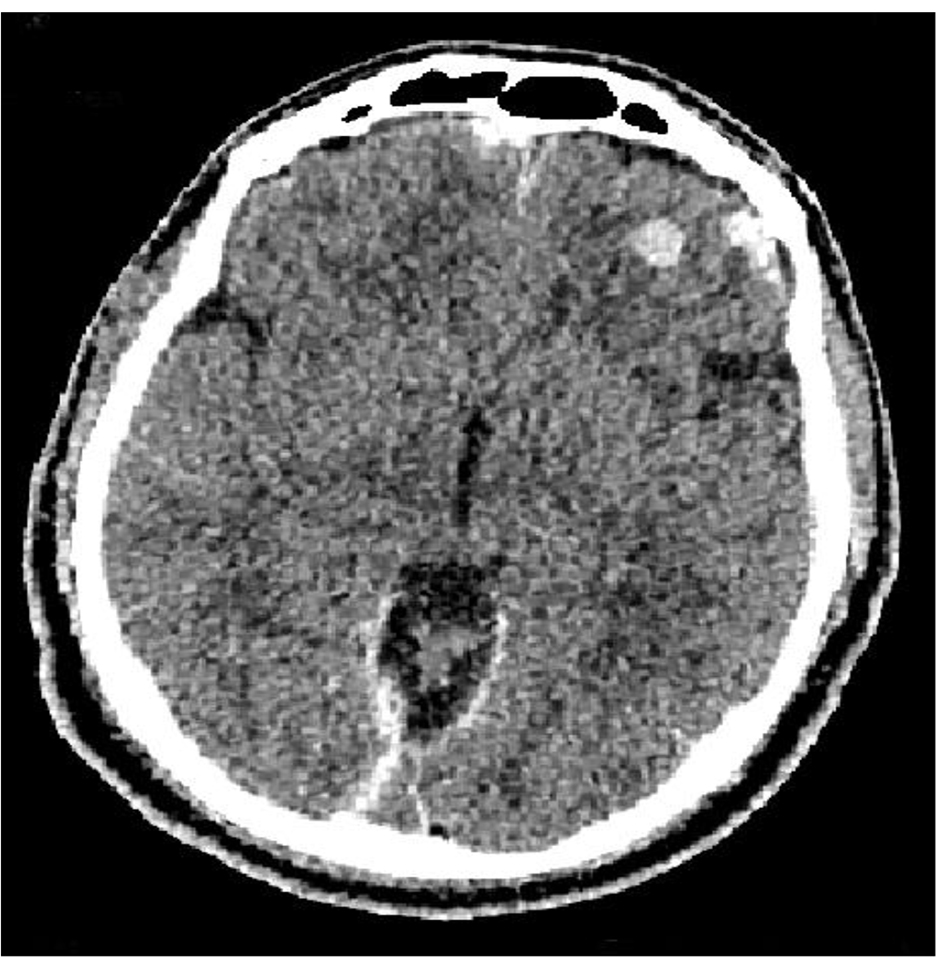 Click for large image | Figure 3. CT of head showing left frontal contusion with diffuse SAH along the falx cerebri. |
 Click for large image | Figure 4. CT of head showing diffuse SAH. |
 Click for large image | Figure 5. CT of head showing SAH with B/L temporal contusions. |
The patient was admitted to the neurology intensive care unit (ICU). On the first hospital day, the patient was noted to have several episodes of non-sustained polymorphic VT. He also had a cardiac arrest due to sustained polymorphic VT. Cardiopulmonary resuscitation for 3 min and defibrillation resulted in return of spontaneous circulation. A repeat EKG showed sinus rhythm with intermittent polymorphic VT but no new ST or T wave changes. The QT interval was normal (410 ms) as was the corrected QT interval (422 ms) (Fig. 6). Acute coronary syndrome was ruled out with three sets of troponin T measurements. Serum electrolytes were within normal limits with a serum potassium of 4.4 mmol/L and a serum magnesium of 2.1 mg/dL. A 2D echocardiogram showed normal left ventricular ejection fraction of 55-60% and impaired LV relaxation.
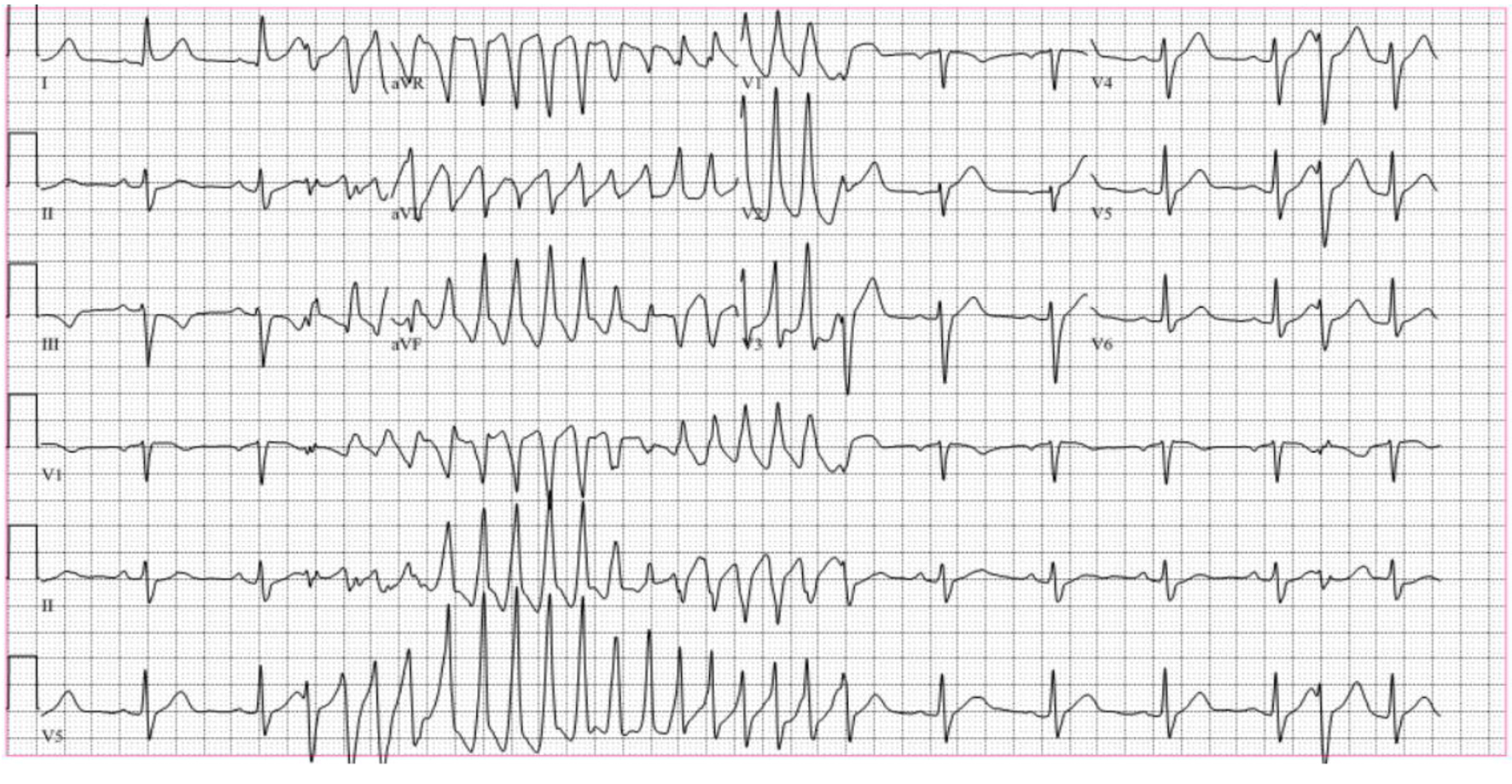 Click for large image | Figure 6. EKG reveals initial sinus rhythm followed by the polymorphic ventricular tachycardia and some intermittent premature ventricular complexes. |
A repeat CT of head showed stability of the SAH. He was managed with lidocaine drip. The patient was also noted to have a few intermittent episodes of sinus bradycardia. Because this was felt to be a potential trigger for the VT, he was started on isoproterenol drip to maintain heart rate between 80 and 100 beats per minute. Additionally, he received mexiletine to control the VT. A nuclear stress test performed to evaluate for ischemia showed a very small fixed perfusion defect in the inferior apical wall. Coronary CT angiogram revealed non-calcified plaque and suggested significant stenosis in the proximal right coronary artery and mid left anterior descending artery.
The patient was weaned from the lidocaine and isoproterenol drips and the frequency of non-sustained polymorphic VT decreased over next 2 weeks. He was transitioned to oral metoprolol. The patient underwent left heart catheterization after 1 month of stability from the bleed, and this showed insignificant coronary artery disease (CAD). The patient declined implantable cardioverter defibrillator (ICD) or implantable loop recorder (ILP) placement. He continues to follow up with cardiology on outpatient basis and is doing well.
| Discussion | ▴Top |
SAH has been linked to ventricular arrhythmias and torsades de pointes (TdP). Studies that have looked for an association between the two are limited due to confounding factors, including medications affecting QTc. The occurrence of ventricular arrhythmias in patients with SAH is thought to be multifactorial [1]. Observations have reported female sex as an independent risk factor for severe QTc prolongation related to SAH. Proposed mechanisms for this finding include hormonal changes (estrogen effect) and increased susceptibility to hypokalemia. One proposed mechanism for increased susceptibility to hypokalemia in females was the sex-specific differences in Na+/K+ ATPase pumps. There is increased Na+/K+ ATPase activity in red blood cells in females causing increased intracellular shifts of potassium and thereby hypokalemia [2]. Various EKG changes that have been observed in patients with SAH are ST segment elevation or depression, T wave inversion and QT interval prolongation [3]. Additionally, left ventricular dysfunction and troponin leak have also been reported in patients with SAH [4].
The proposed pathophysiology for ventricular arrhythmias in patients with SAH is the overactivation of the sympathetic nervous system resulting in catecholamine surge, especially noradrenaline. This is likely due to interrupted vascular supply to the hypothalamus in SAH. This in turn results in tachycardia, coronary vasospasm and increased intracellular calcium which can prolong repolarization phase of the cardiac action potential. These changes together can increase the risk for ventricular arrhythmias [5]. One small study suggests increased QT dispersion in patients with SAH. Increased plasma concentration of catecholamines in patients with SAH has been reported [6]. Further, persistence of the QTc prolongation was observed for a longer duration in patients having poor neurological outcome or death from SAH compared to those patients with good recovery. It is suggested there is normalization of the QTc duration as the patients’ neurological status improved [7].
Our patient presented with a primary intracranial CNS bleed and polymorphic VT which was extremely difficult to control. He required aggressive antiarrhythmic therapy. Common etiologies of polymorphic VT were excluded. No structural or ischemic heart disease was identified. The serum electrolytes were normal and no QT prolonging medications were administered. The baseline QT interval was normal making congenital long QT syndrome unlikely. Our patient received propofol for sedation on the first day of hospitalization but this was later discontinued. Propofol should be used with caution in those at risk of VT, but the association between the two remains unclear [8]. It is less likely that the propofol contributed to VT in our case as the patient continued to have recurrent episodes of non-sustained VT despite being off propofol.
The etiology of the recurrent polymorphic VT in our patient thus remains unclear. We suspect it was related to autonomic nervous system dysfunction from his SAH as outlined previously. The VT gradually resolved as his neurologic status improved. Reports associating ventricular arrhythmias and SAH have been described, yet the mechanism of this association remains unclear. Previous observations of VT seen in this setting suggest a relationship with QT prolongation. The QT interval, however, remained normal in our patient, suggesting an alternative and unknown mechanism for the polymorphic VT.
| References | ▴Top |
- Machado C, Baga JJ, Kawasaki R, Reinoehl J, Steinman RT, Lehmann MH. Torsade de pointes as a complication of subarachnoid hemorrhage: a critical reappraisal. J Electrocardiol. 1997;30(1):31-37.
doi - Fukui S, Katoh H, Tsuzuki N, Ishihara S, Otani N, Ooigawa H, Toyooka T, et al. Multivariate analysis of risk factors for QT prolongation following subarachnoid hemorrhage. Crit Care. 2003;7(3):R7-R12.
doi pubmed - Sakr YL, Ghosn I, Vincent JL. Cardiac manifestations after subarachnoid hemorrhage: a systematic review of the literature. Prog Cardiovasc Dis. 2002;45(1):67-80.
doi pubmed - Izurieta C, Curotto-Grasiosi J, Trossero R, Cardus M, Filipini E, Abdala A, Alasia D, et al. [QTc interval prolongation and polymorphic ventricular tachycardia related to subarachnoid hemorrhage]. Arch Cardiol Mex. 2013;83(1):40-44.
doi pubmed - Lorsheyd A, Simmers TA, Robles De Medina EO. The relationship between electrocardiographic abnormalities and location of the intracranial aneurysm in subarachnoid hemorrhage. Pacing Clin Electrophysiol. 2003;26(8):1722-1728.
doi pubmed - Randell T, Tanskanen P, Scheinin M, Kytta J, Ohman J, Lindgren L. QT dispersion after subarachnoid hemorrhage. J Neurosurg Anesthesiol. 1999;11(3):163-166.
doi pubmed - Ichinomiya T, Terao Y, Miura K, Higashijima U, Tanise T, Fukusaki M, Sumikawa K. QTc interval and neurological outcomes in aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2010;13(3):347-354.
doi pubmed - Abrich VA, Ramakrishna H, Mehta A, Mookadam F, Srivathsan K. The possible role of propofol in drug-induced torsades de pointes: A real-world single-center analysis. Int J Cardiol. 2017;232:243-246.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


