| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 12, Number 6, December 2021, pages 340-343
Rate of Recovery of Left Ventricular Ejection Fraction in a Real-World Population of Patients Receiving a Wearable Cardioverter Defibrillator
Lon Abneya, c, Tyler Coombesa, Laylan Shalia, Jared Spoonsa, W. Jeremy Mahlowa, b
aDepartment of Medicine, University of Tennessee Graduate School of Medicine, Knoxville, TN, USA
bHeart Lung Vascular Institute, University of Tennessee Medical Center, Knoxville, TN, USA
cCorresponding Author: Lon Abney, Department of Medicine, University of Tennessee Graduate School of Medicine, 1940 Alcoa Hwy, Suite E-310, Knoxville, TN 37920, USA
Manuscript submitted September 24, 2021, accepted October 26, 2021, published online November 11, 2021
Short title: Early EF Recovery in Patients With a WCD
doi: https://doi.org/10.14740/cr1325
| Abstract | ▴Top |
Background: This study aimed to investigate the rate of early improvement in ejection fraction (EF) within 21 - 60 days among patients with cardiomyopathy who were provided with a wearable cardioverter defibrillator (WCD).
Methods: This was a retrospective study of patients who received a WCD at our institution to determine the rate of improvement in left ventricular EF (LVEF) to ≥ 35-40%. Among 990 patients who received a WCD during the study period, 101 had an echocardiogram performed during the subsequent 21 - 60 days. Patients were stratified according to their initial EF, as well as age, gender, number of heart failure medications, and ischemic vs. nonischemic cardiomyopathy. Multivariate logistic regression analysis was performed to assess the influence of these variables on the subsequent improvement in EF.
Results: There were 39 patients who had improvement in their EF to ≥ 35-40%. The only significant predictor of EF recovery was the initial EF. There was a direct correlation between initial EF category and the likelihood of improvement in EF. For every unit increase in initial EF category, the odds of improvement increased 1.73 times (95% confidence interval (CI): 1.22 - 2.45). Age (P = 0.20), gender (P = 0.10), ischemic cardiomyopathy (P = 0.40), and number of heart failure medications at the time of WCD placement (P = 0.26) were not significant predictors of improved LVEF.
Conclusions: This study showed a rate of improvement in EF to ≥ 35-40% of 39% within 21 - 60 days of placement of a WCD among patients with both ischemic and nonischemic cardiomyopathy. The only significant clinical predictor of EF improvement was initial EF.
Keywords: Wearable cardioverter defibrillator; Ejection fraction recovery; Cardiomyopathy
| Introduction | ▴Top |
Wearable cardioverter defibrillators (WCDs) are currently a class IIb recommendation for patients who are at increased risk of sudden cardiac death but do not yet meet criteria for implantable cardioverter defibrillators (ICDs) [1]. This population includes patients with reduced ejection fraction (EF) that are within 40 days of a myocardial infarction, 90 days of revascularization, or 90 days of newly diagnosed nonischemic dilated cardiomyopathy in which the underlying cause is potentially treatable. These chronological parameters were established by early clinical trials in which patients with ischemic cardiomyopathy that were randomly assigned to ICD implantation early after an acute myocardial infarction did not live longer than controls [2, 3]. While the WCD is a tool that has been shown to reduce mortality after acute myocardial infarction and in patients with newly diagnosed nonischemic cardiomyopathy, it does entail certain financial, physical, and psychological costs to the patient, including the discomfort of wearing the device and the risk of inappropriate shocks [1]. Balancing the costs, risks, and benefits of WCDs can present a significant challenge to both patient and physician. In usual clinical practice, a WCD is prescribed until the patient’s EF is reevaluated after a time interval of 40 or 90 days, at which time a permanent ICD is recommended if appropriate. Occasionally, a patient will receive an echocardiogram prior to the completion of this time interval which reveals that their EF has improved, and the WCD is discontinued at that point. This study sought to identify how many patients have early recovery of EF to ≥ 35-40% (within 21 - 60 days after the placement of a WCD) and any characteristics that might predict such recovery in this real-world population.
| Materials and Methods | ▴Top |
We performed a retrospective chart review of patients who received a WCD at the University of Tennessee Medical Center at Knoxville from January 2013 to September 2020. The study was approved by the Institutional Review Board, and there was no trial sponsor or funding source. Only patients with at least 60 days of follow-up data were included in the study. We performed multivariate logistic regression analysis to determine the impact of the following factors on EF recovery: age, gender, ischemic vs. nonischemic cardiomyopathy, baseline EF prior to placement of the WCD, and number of heart failure medications at the time of WCD placement. EF recovery was defined as achieving an EF of ≥ 35-40%, and patients were stratified according to initial EF as follows: < 15%, 15-20%, 20-25%, 25-30%, 30-35%, and 35-40%.
| Results | ▴Top |
A total of 990 patients received a WCD and had adequate follow-up data, of whom 116 patients had an echo performed within 21 - 60 days after placement of the WCD. Fifteen patients were excluded either because they received the WCD for a diagnosis other than cardiomyopathy with an EF ≤ 35-40%, or they had a structural intervention prior to reassessment of their EF, such as a transcatheter aortic valve replacement or cardiac resynchronization therapy. The mean time from WCD placement to assessment of EF was 40 days. The mean age of all patients was 61 (range: 28 - 85 years), and 38% were female. Patients with nonischemic and ischemic cardiomyopathy were equally represented. Among the 101 patients included in the final analysis, 39 had recovery of their EF within 21 - 60 days after placement of the WCD (Tables 1, 2). When controlling for all variables, the only significant predictor of EF recovery was initial EF (P = 0.002, Fig. 1). A certain percentage of patients in all EF strata did achieve recovery of their EF, and this fraction increased according to increasing baseline EF. For every unit increase in pre-vest EF, the odds of improvement increase 1.73 times (95% confidence interval (CI): 1.22 - 2.45). Age (P = 0.20), gender (P = 0.10), ischemic cardiomyopathy (P = 0.40), and number of heart failure medications at the time of WCD placement (P = 0.26) were not significant predictors of improved left ventricular EF (LVEF). None of the patients died while wearing the cardioverter-defibrillator. We did not collect data on the number of shocks patients received (either appropriate or inappropriate) while wearing the WCD. Over a mean follow-up period of 34 months, 11 patients eventually had an ICD placed. The rate of eventual ICD placement did not exhibit linear correlation with the baseline EF. There were a number of reasons that patients with reduced EF did not go on to eventual ICD placement. These included the presence of comorbid conditions limiting their life expectancy to less than 1 year, being poor candidates for advanced therapies for other reasons, transitioning to hospice or experiencing mortality, or being lost to follow-up. This study was approved by the Institutional Review Board and conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
 Click to view | Table 1. Patient Characteristics |
 Click to view | Table 2. Patients Stratified According to Initial EF |
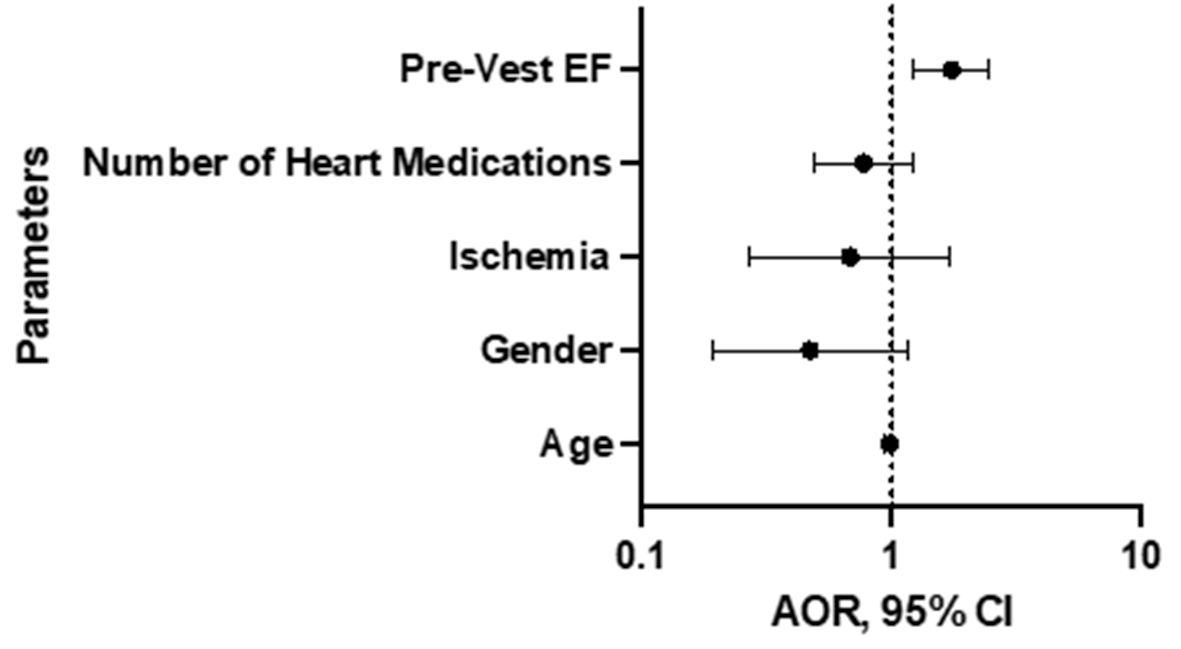 Click for large image | Figure 1. Results of multivariate logistic regression analysis. “Pre-Vest EF” refers to baseline EF prior to placement of wearable cardioverter defibrillator. EF: ejection fraction; AOR: adjusted odds ratio; CI: confidence interval. |
| Discussion | ▴Top |
While the WCD provides significant benefit in terms of protection from sudden cardiac death, there are financial and psychological costs associated with the device, and patients generally prefer to avoid wearing the device any longer than necessary. However, this study showed that in a real-world population, only 12% of patients had an assessment of EF sooner than the usual standard ICD waiting period (21 - 60 days as opposed to 90 days). A certain number of patients who are using a WCD for primary prevention of sudden cardiac death will have improvement in their EF prior to the pre-established waiting period, and this study sought to identify characteristics that would predict early EF recovery and thus determine the patients that may benefit most from having an echocardiogram performed earlier than the typical 90 days. In our study, 39% of patients had recovery of their EF to ≥ 35-40% within 21 - 60 days of placement of the WCD. In two recent large, retrospective analyses of patients with heart failure, 38% and 34% of patients had recovery of their EF (defined as improvement > 10%) after a waiting period of at least 6 months or 9 weeks, respectively, which is similar to the rate of recovery in our population [4, 5]. Previous studies have identified several factors associated with EF recovery, including female sex, younger age, nonischemic cardiomyopathy, lower baseline EF, left ventricle end-diastolic volume, and tricuspid annular plane systolic excursion (TAPSE) [4-6]. The failure to identify any significant factor aside from initial EF in predicting recovery in this study may have been related to the small sample size. Nevertheless, multiple studies have consistently demonstrated that approximately one-third of patients with heart failure can be expected to achieve an improvement in their EF; and one could consider evaluation of the patient’s EF prior to the pre-established waiting period, especially if they possess the characteristics listed above.
Limitations
This was a retrospective, observational, single-center study. Because enrollment depended on patients receiving an echocardiogram for some indication prior to the standard waiting period after placement of a WCD, this may have introduced selection bias resulting in patients who had other conditions or cardiac complications that affected their rate of EF recovery, or lack thereof. This retrospective design also raises the possibility of confounding factors. The echocardiograms were not performed or interpreted by a core laboratory or specific study personnel, which may have affected the overall accuracy of results. Finally, in order to apply any findings to broad classes of patients, we limited the number of variables we assessed, and the inclusion of additional factors may have identified patients whose EF was more likely to recover.
Conclusions
In this retrospective, single-center study, among patients with both ischemic and nonischemic cardiomyopathy who received a WCD, 39% had improvement of their EF to ≥ 35-40% within 21 - 60 days, of which initial EF was the only significant predictor of recovery. The greater the initial EF, the more likely patients would achieve recovery. The following variables did not predict EF recovery: gender, ischemic versus nonischemic cardiomyopathy, or number of heart failure medications.
Acknowledgments
We appreciate the support of Zoll for providing data on patients who have received wearable cardioverter defibrillators at our institution.
Financial Disclosure
There was no specific funding source to be mentioned.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
In accordance with IRB protocol, this study involved only information collection and analysis which did not require consent.
Author Contributions
LA and JM have designed and performed the study. TC, LS, and JS have assisted and supported in data collection. LA has drafted the manuscript and JM carefully supervised the manuscript preparation and writing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon request.
| References | ▴Top |
- Piccini JP, Sr., Allen LA, Kudenchuk PJ, Page RL, Patel MR, Turakhia MP, American Heart Association E, et al. Wearable cardioverter-defibrillator therapy for the prevention of sudden cardiac death: a science advisory from the American Heart Association. Circulation. 2016;133(17):1715-1727.
doi pubmed - Hohnloser SH, Kuck KH, Dorian P, Roberts RS, Hampton JR, Hatala R, Fain E, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med. 2004;351(24):2481-2488.
doi pubmed - Steinbeck G, Andresen D, Seidl K, Brachmann J, Hoffmann E, Wojciechowski D, Kornacewicz-Jach Z, et al. Defibrillator implantation early after myocardial infarction. N Engl J Med. 2009;361(15):1427-1436.
doi pubmed - Ghimire A, Fine N, Ezekowitz JA, Howlett J, Youngson E, McAlister FA. Frequency, predictors, and prognosis of ejection fraction improvement in heart failure: an echocardiogram-based registry study. Eur Heart J. 2019;40(26):2110-2117.
doi pubmed - DeVore AD, Hellkamp AS, Thomas L, Albert NM, Butler J, Patterson JH, Spertus JA, et al. Improvement in left ventricular ejection fraction in outpatients with heart failure with reduced ejection fraction: data from CHAMP-HF. Circ Heart Fail. 2020;13(7):e006833.
doi - Shah MA, Soofi MA, Jafary Z, Alhomrani A, Alsmadi F, Wani TA, Bajwa IA. Echocardiographic parameters associated with recovery in heart failure with reduced ejection fraction. Echocardiography. 2020;37(10):1574-1582.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


