| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 13, Number 5, October 2022, pages 289-296
Carotid Artery Revascularization Improves Cardiac Sympathetic Nerve Activity in Patients With Carotid Artery Stenosis
Tsukasa Katoa, Wakana Satoa, Teruki Satoa, Hiroaki Shimizub, Hiroyuki Watanabea, c
aDepartment of Cardiovascular Medicine, Akita University Graduate School of Medicine, Akita, Japan
bDepartment of Neurosurgery, Akita University Graduate School of Medicine, Akita, Japan
cCorresponding Author: Hiroyuki Watanabe, Department of Cardiovascular Medicine, Akita University Graduate School of Medicine, Akita 010-8543, Japan
Manuscript submitted July 7, 2022, accepted September 3, 2022, published online October 25, 2022
Short title: Cardiac Effects of Carotid Revascularization
doi: https://doi.org/10.14740/cr1402
| Abstract | ▴Top |
Background: The carotid sinus baroreceptor reflex controls the neural regulation of blood pressure. Baroreceptor disorders due to carotid sinus atherosclerosis have detrimental cardiovascular effects. This study investigated the medium-term effects of carotid artery revascularization (CAR) on sympathetic and cardiac function and systemic blood pressure variability in patients with carotid artery stenosis.
Methods: This study included 21 consecutive patients (median age 70 years, 18 men) with carotid artery stenosis scheduled for CAR. 123I metaiodobenzylguanidine (MIBG) scintigraphy, echocardiography, brain natriuretic peptide levels, 24-h Holter electrocardiography (ECG), and ambulatory blood pressure monitoring assessed approximately 3 months postoperatively were compared to preoperative data.
Results: All 21 enrolled patients underwent CAR. Carotid artery stenting was done in three patients with cardiovascular risk or anatomical difficult for carotid endarterectomy. The mean common carotid artery end-diastolic velocity improved significantly (P < 0.01) by 1.6-fold, from 10.8 ± 3.2 to 16.1 ± 7.1 cm/s. In 123I-MIBG scintigraphy, the heart-to-mediastinum (H/M) count ratio was significantly higher than preoperatively (from 2.66 ± 0.48 to 2.86 ± 0.56, P = 0.03). Holter ECG analysis revealed a significant decrease in the low-frequency/high-frequency (LF/HF) ratio compared to preoperatively (from 2.17 ± 1.20 to 1.62 ± 0.68, P = 0.04). These findings suggest decreased myocardial sympathetic activation. In echocardiography, the tissue Doppler-derived e’ increased, and E/e’ decreased significantly (P < 0.05) from 11.7 ± 5.1 to 10.1 ± 4.0, suggesting an improved left ventricular diastolic capacity. The mean 24-h and nighttime blood pressures were unchanged.
Conclusions: CAR in patients with carotid stenosis may provide medium-term improvement in cardiac sympathetic nerve activity and left ventricular diastolic dysfunction.
Keywords: Carotid sinus baroreceptor; Carotid artery stenosis; Carotid artery stenting; Carotid endarterectomy; Cardiac sympathetic nerve activity; HFpEF; 123I-MIBG scintigraphy; Echocardiography
| Introduction | ▴Top |
The carotid sinus baroreceptor (CSB) reflex controls the neural regulation of blood pressure. When the CSB senses an increase in blood pressure, a signal is propagated along afferent nerves to the central nervous system and serves as negative feedback, leading to bradycardia and hypotension. The molecular nature of the CSB is ion channels at the nerve endings within the artery adventitia. The location enables external stimulation of the CSB. In a study of conscious dogs, electrodes implanted around both carotid sinuses and electrical activation of the CSB using an externally adjustable pulse generator reduced the mean arterial pressure and heart rate [1]. Recently, baroreflex activation therapy (BAT) devices have been developed for treating hypertension and heart failure [2]. Abraham et al demonstrated that BAT significantly improved the quality of life, exercise capacity, N-terminal pro-brain natriuretic peptide (BNP) level, left ventricular ejection fraction (LVEF), and the burden of heart failure hospitalization in patients with guideline-directed medical and device-treated New York Heart Association Class III heart failure [3].
Conversely, baroreceptor failure has detrimental effects on the cardiovascular system. Rats with baroreceptor failure cannot buffer the volume load and develop heart failure [4]. Carotid sinus atherosclerosis is one cause of baroreceptor failure. Patients with carotid stenosis (CS) are at high risk for cerebrovascular events [5], and severe CS is a risk factor for stroke. The treatment of CS includes medical therapy, carotid artery stenting (CAS), and carotid endarterectomy (CEA). Studies have shown the acute effects of carotid artery revascularization (CAR), including CEA and CAS, in which CAR alters the mechanical properties of the arterial wall and affects carotid sinus nerve activity and systemic blood pressure [6-8]. However, no study has evaluated its medium-term effects on cardiac sympathetic nerve activity (CSNA) and the cardiovascular system.
This study investigated the medium-term effects of CAR on sympathetic function, cardiac function, and blood pressure variability in patients with CS.
| Materials and Methods | ▴Top |
Study patients and protocol
The study was approved by our ethics review board and was conducted in compliance with the institutional ethical standards for studies of human subjects and the Declaration of Helsinki. The study included 21 consecutive patients scheduled for CAR at Akita University School of Medicine between December 2014 and August 2018. The patients were aged 69.5 ± 6.8 years; there were 18 men (86%) and three women (14%) with cardiovascular disease risk factors, such as hypertension and diabetes. Three patients on beta-blockers, which can affect cardiac autonomic activity, were included. Although sleep apnea syndrome is commonly associated with increased sympathetic nervous system activity, none of the patients were affected. Table 1 shows the patient characteristics.
 Click to view | Table 1. Patient Characteristics |
Figure 1 shows the study protocol. Before CAR, all patients underwent cerebral perfusion single-photon emission computed tomography and carotid artery ultrasonography. The surgery indications followed the 2009 Society for Stroke Medicine guidelines. The assignment to either CAS or CEA was not random. CAS was selected as an alternative therapy in patients who were considered high risk for CEA [9]. Patients who consented to each examination underwent 123iodine metaiodobenzylguanidine (123I-MIBG) scintigraphy, Holter electrocardiography (ECG), 24-h ambulatory blood pressure monitoring (ABPM), transthoracic echocardiography, and BNP measurements immediately before CAR. Each examination was repeated approximately 3 months later to assess the effects of CAR on CSNA and the cardiovascular system.
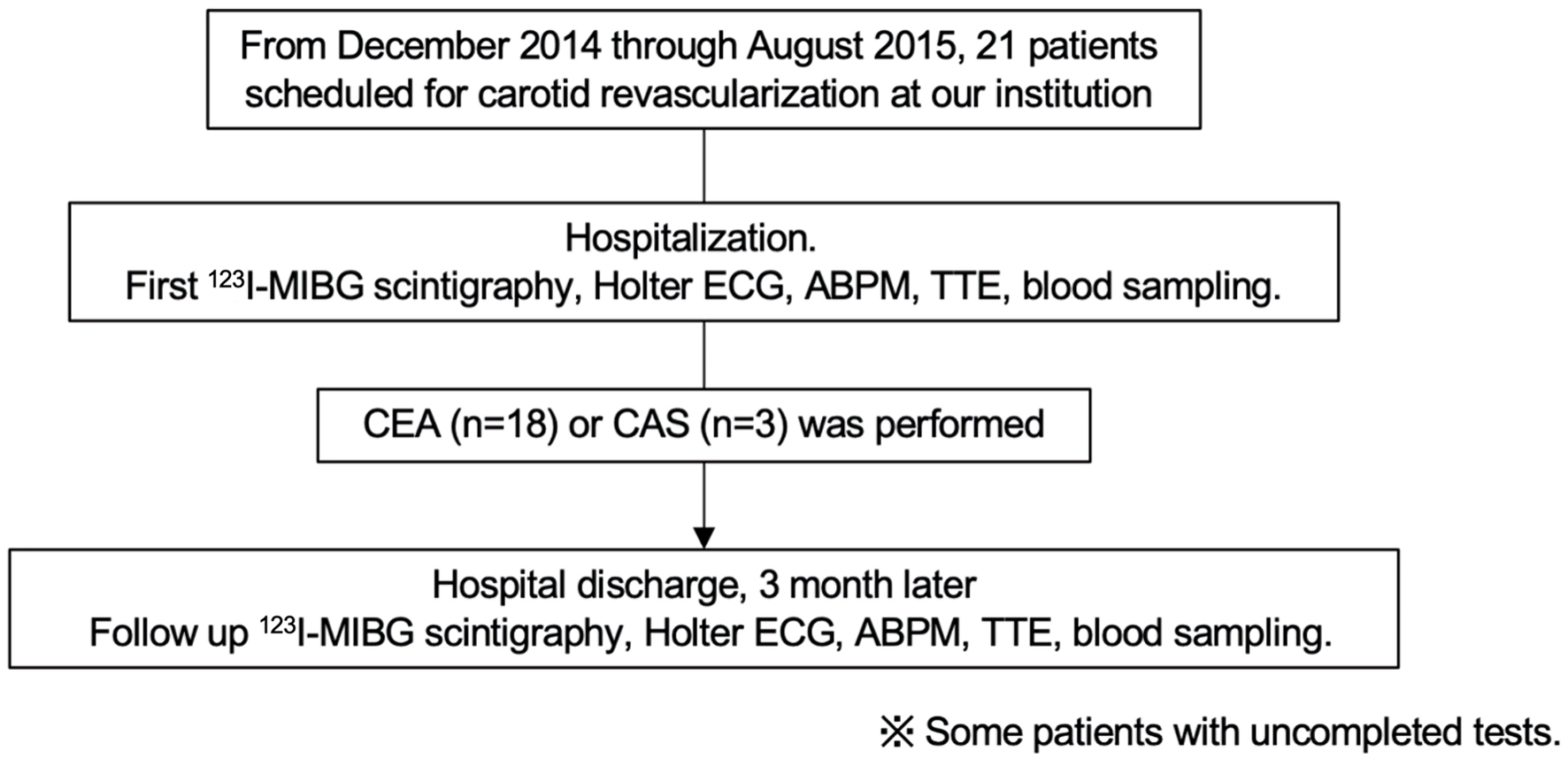 Click for large image | Figure 1. Patients and protocol. ECG: electrocardiography; 123I-MIBG scintigraphy: iodine-123-metaiodobezylguanidine scintigraphy; ABPM: ambulatory blood pressure monitoring; TTE: transthoracic echocardiography; CEA: carotid endarterectomy; CAS: carotid artery stenting. |
123I-MIBG scintigraphy
MIBG, an analog of norepinephrine, is transported into the presynaptic nerve terminals primarily by the sodium- and ATP-dependent transporter uptake-1. MIBG is not degraded; instead, it accumulates at nerve terminals. Labeling of MIBG with 123iodine allows visualization of its uptake into cardiomyocytes and neurons. 123I-MIBG scintigraphy is used extensively to obtain diagnostic and prognostic information for patients with heart failure [10-14]. In this study, 123I-MIBG scintigraphy was used as an index of the changes in CSNA caused by CAR. The 123I-MIBG imaging method followed previous reports [11, 14]. Supine patients were injected intravenously with 123I-MIBG (111 MBq). Static image data were acquired 15 min and 4 h after the injection, in the anterior view using a γ-camera (Symbia T2; Siemens Healthcare, Malvern, PA, USA) equipped with a low-middle energy general-purpose parallel-hole collimator. Static images on a 256 × 256 matrix were collected with a 20% window centered on 159 keV, corresponding to the 123I photopeak. The heart-to-mediastinum count (H/M) ratio was determined from the anterior planar delayed 123I-MIBG image following the method of Merlet et al [15].
24-h Holter ECG
The analysis of heart rate variability and its low-frequency (LF) and high-frequency (HF) components are commonly used as an autonomic index and its relevance has been reported [16]. The R-R series was resampled at 4 Hz by cubic spline interpolation to obtain the time series of evenly spaced samples. The resampled signal was split into 50% overlapping epochs of 1,024 points that corresponded to 4.27 min of recording. Linear trends were removed and a Hanning window was applied to each epoch. The power spectra of all epochs were computed using Fast Fourier Transform and ensemble averaged. The LF and HF powers were computed as areas under the averaged power spectrum at the corresponding frequency bands. Total power (TP) was calculated as TP = LF + HF, and the LF and HF spectra were normalized to TP (normalized LF (nLF) = LF/TP; normalized HF (nHF) = HF/TP). The LF/HF ratio was calculated.
Transthoracic echocardiography
Echocardiography was performed using an iE33 echocardiography system (Phillips Medical Systems, Bothell, WA, USA). LVEF, left ventricular mass index (LVMI), and diameter were calculated from standard M-mode echocardiograms. Mitral inflow velocity was traced, and we derived the peak early (E) and late (A) trans-mitral flow velocities and ratio of early to late peak velocities (E/A). The early peak diastolic annular velocity (e’) was determined from spectral pulsed-wave tissue Doppler imaging recordings and the mitral E/e’ ratio was calculated. The sample volume at the septal corner of the mitral annulus was used for the apical four-chamber view.
24-h ABPM
The 24-h ABPM was performed according to the Japanese Circulation Society (JCS) guidelines [17], with measurements at 10-min intervals during the day and 30-min intervals at night. According to the conventional definition, we classified the diurnal variation in blood pressure into four types as follows: extreme dippers if the nocturnal systolic blood pressure fall was ≥ 20%, dippers if the fall was ≥ 10% but < 20%, non-dippers if it was ≥ 0% but < 10%, and risers if it was < 0% [17, 18].
Statistical analysis
Continuous variables with normal distributions are expressed as the mean ± standard deviation (SD). Variables with nonnormal distributions are expressed as the median (interquartile range). Paired t-tests were used to compare the pre- and postoperative individual test data. A P value < 0.05 was considered to indicate statistical significance. JMP ver.16.0.0 (SAS Institute, Cary, NC, USA) and GraphPad PRISM ver. 7.03 (GraphPad, San Diego, CA, USA) were used for the statistical analyses.
| Results | ▴Top |
All 21 enrolled patients underwent carotid revascularization. CAS was selected for three patients with cardiovascular risk or anatomical difficulty for CEA. The mean common carotid artery end-diastolic velocity (CCA-EDV (cm/s)) improved significantly by 1.6-fold (P < 0.01), from 10.8 ± 3.2 to 16.1 ± 7.1 cm/s (Table 2). There was a significant increase in cerebral blood flow compared to preoperatively. Figure 2 shows a representative case with improved CSNA and left ventricular diastolic capacity after CAR.
 Click to view | Table 2. Comparison of Common Carotid Artery Flow Before and After Revascularization |
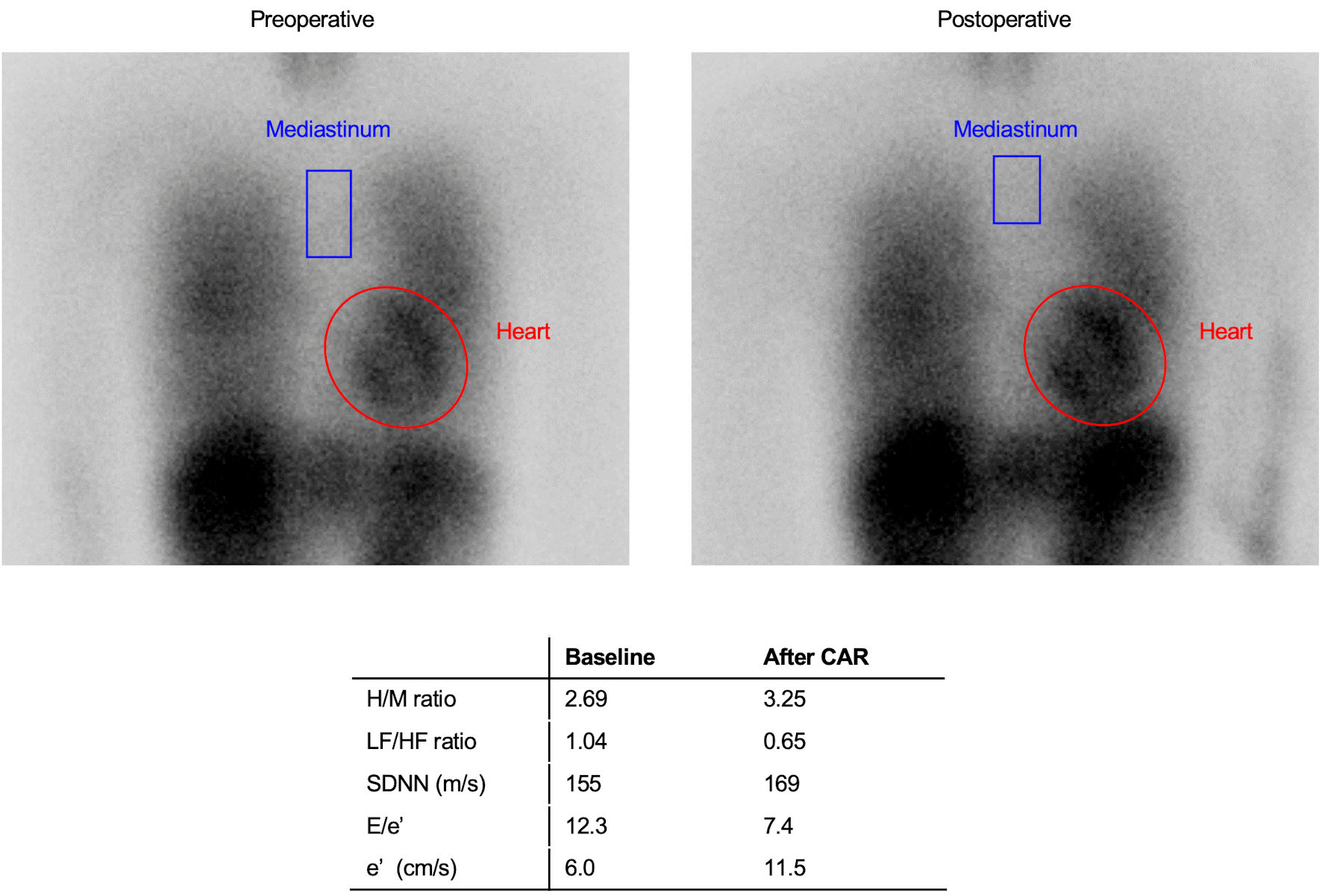 Click for large image | Figure 2. Representative case of improvement in sympathetic function after CAR. A 57-year-old woman with general cardiovascular risk factors, including hypertension and dyslipidemia was not taking beta-blockers. The H/M ratio on 123I-MIBG scintigraphy was calculated by dividing the mean pixel value within the myocardium by the mean pixel value within the mediastinum, using the region of interest (ROI) of the entire heart and the upper mediastinum on the planar image. Compared to pre-CAR, MIBG uptake in the heart was higher than in the upper mediastinum, suggesting decreased sympathetic nerve activity. CAR: carotid artery revascularization; H/M: heart-to-mediastinum; 123I-MIBG: iodine-123-metaiodobezylguanidine; LF: low-frequency; HF: high-frequency; SDNN: standard deviation of the N-N interval. |
First, the pre- and postoperative changes in the H/M ratio on 123I-MIBG scintigraphy and the LF/HF ratio and SD of the N-N interval (SDNN) on the 24-h Holter ECG, which are indicators of sympathetic activation, were reviewed. 123I-MIBG scintigraphy was performed on 15 patients and the H/M ratio was significantly higher postoperatively than preoperatively (from 2.66 ± 0.48 to 2.86 ± 0.56, P < 0.05) (Fig. 3a), suggesting decreased myocardial sympathetic activation. Holter ECG performed on 15 patients revealed a significant decrease in the LF/HF ratio compared to preoperatively (from 2.17 ± 1.20 to 1.62 ± 0.68, P < 0.04), while SDNN tended to increase compared to preoperatively, albeit not significantly (Fig. 3b).
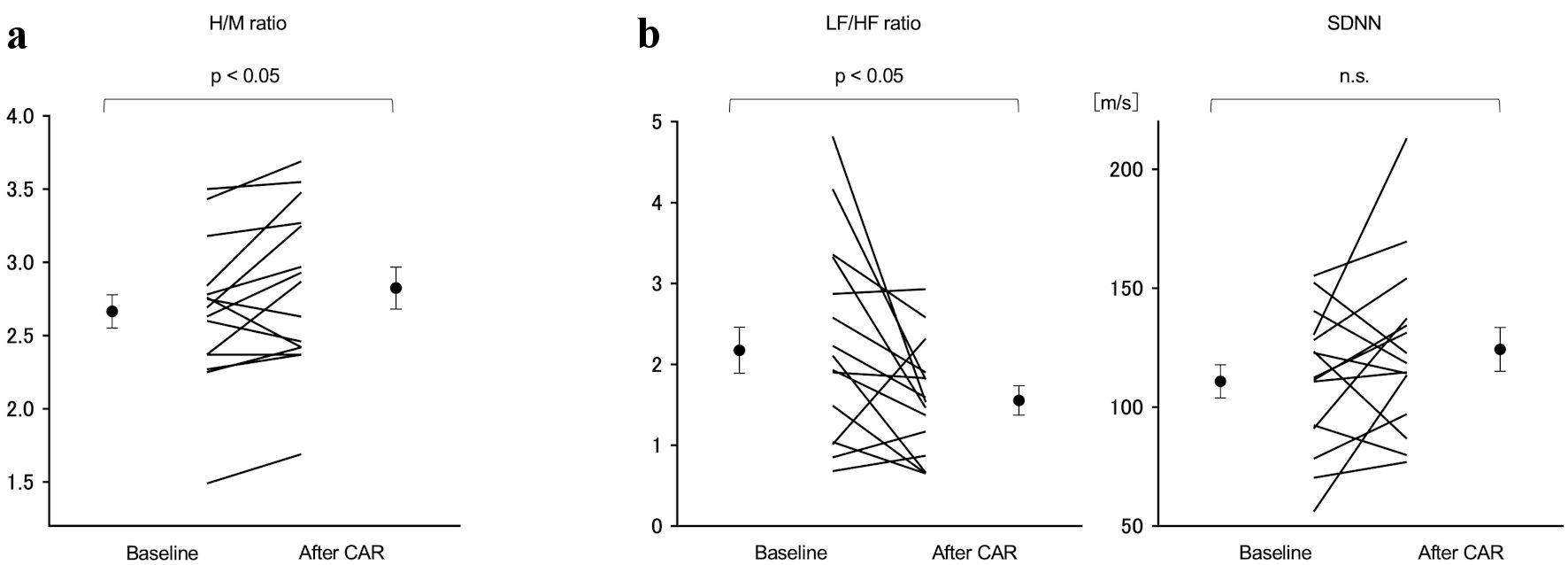 Click for large image | Figure 3. Comparison of the H/M ratio on the 123I MIBG scintigraphy and LF/HF ratio and SDNN on 24-h Holter ECG pre- and post-CAR. (a) The H/M ratio increased significantly from 2.66 ± 0.48 preoperatively to 2.86 ± 0.56 postoperatively (P < 0.05). (b) The LF/HF ratio decreased significantly from 2.17 ± 1.20 preoperatively to 1.62 ± 0.68 postoperatively (P < 0.04). SDNN showed no change. H/M: heart-to-mediastinum; 123I-MIBG: iodine-123-metaiodobezylguanidine; LF: low-frequency; HF: high-frequency; SDNN: standard deviation of the N-N interval; CAR: carotid artery revascularization. |
Echocardiography was performed in 17 patients and no obvious changes in left ventricular end-diastolic diameter (LVDd), left ventricular end-systolic diameter (LVDs), or the LVMI were observed (Table 3). The LVEF decreased significantly from 67.8±7.7% preoperatively to 64.8±7.2% (Fig. 4a). However, the tissue Doppler-derived e’ increased and E/e’ decreased significantly from 11.7 ± 5.1 to 10.1 ± 4.0 (P < 0.05) (Fig. 4b). These findings indicated improved left ventricular diastolic capacity. BNP levels were measured in 16 patients, but the values did not change significantly before and after CAR (Table 3).
 Click to view | Table 3. Comparison of Pre- and Postoperative Echocardiographic Data and Laboratory Data |
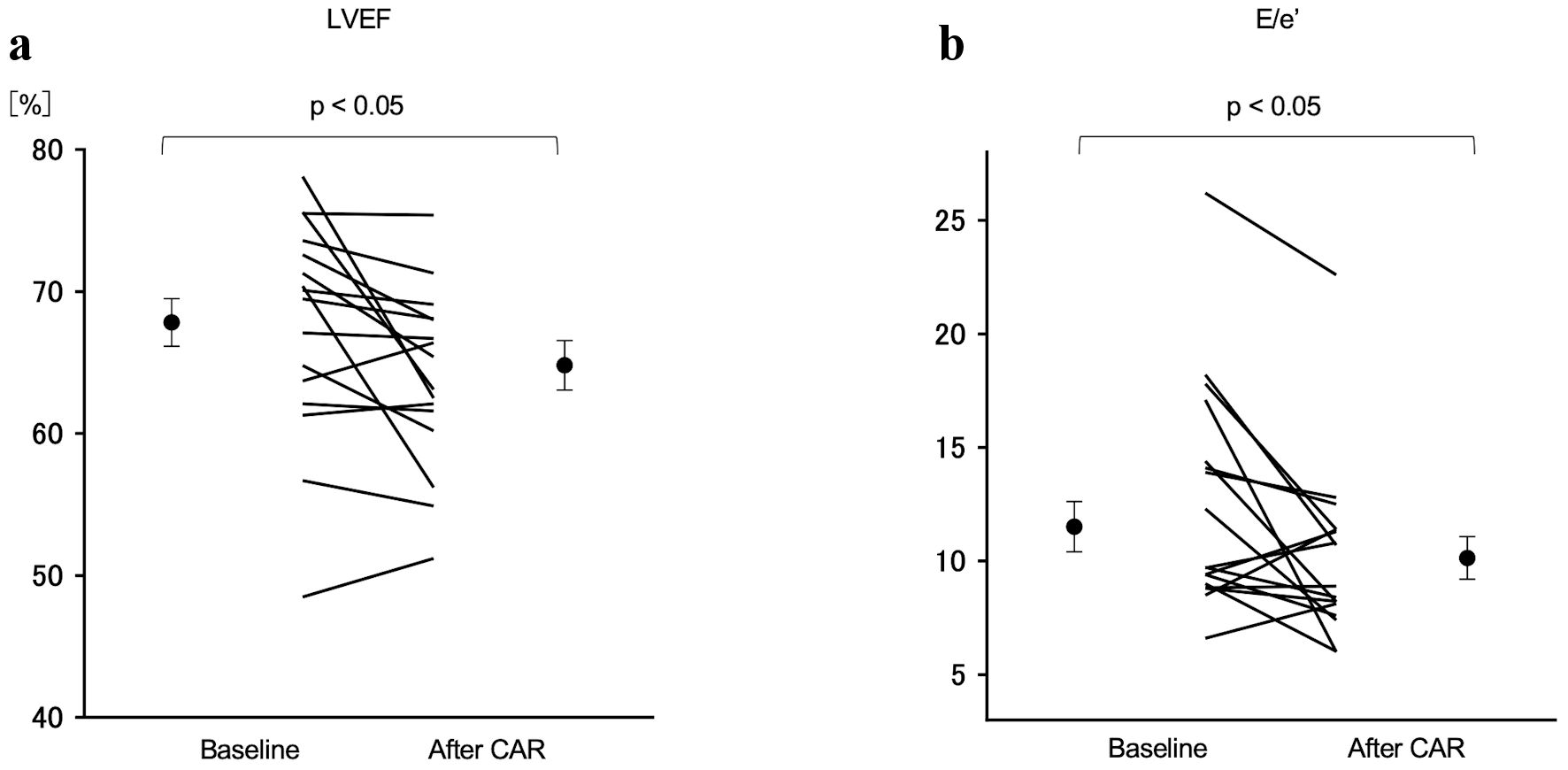 Click for large image | Figure 4. Comparison of LVEF and E/e’ between pre- and post-CAR. (a) The LVEF decreased significantly from 67.8±7.7% preoperatively to 64.8±7.2% postoperatively (P < 0.05). (b) The E/e’ decreased significantly from 11.7 ± 5.1 preoperatively to 10.1 ± 4.0 postoperatively (P < 0.05). LVEF: left ventricular ejection fraction; CAR: carotid artery revascularization. |
Finally, ABPM was performed in 16 patients. The mean 24-h and nighttime blood pressures were unchanged. Classifying the patients according to their nocturnal systolic blood pressure reduction pattern as extreme dipper, dipper, non-dipper, and riser, no significant change in the dipping pattern was seen (Table 4).
 Click to view | Table 4. Comparison of Pre- and Postoperative ABPM Data |
| Discussion | ▴Top |
This study is the first to examine the medium-term effects of CAR on CSNA and cardiac function in patients with carotid artery stenosis. We found that the H/M ratio in 123I-MIBG myocardial scintigraphy was significantly increased, while the LF/HF ratio in 24-h Holter ECG was significantly decreased, suggesting that CAR decreased CSNA. In echocardiography, E/e’ decreased significantly, which implies improved left ventricular diastolic capacity. The 24-h mean and nocturnal blood pressures did not improve in ABPM.
There have been many reports on the effects of CEA on CSB activity [7, 19, 20]. CEA is thought to improve CSB activity because removing pathologically thickened intima and tunica media enhances the vessel wall extensibility. However, the CSNA may be hyperactive due to damage to the carotid sinus nerve during CEA and local edema in the early postoperative period. However, these reports only show the intra- and acute postoperative responses. Demirci et al investigated the effects of CEA and CAS on heart rate variability and noted a decrease in LF/HF ratio in assessments up to 4 days after CAS [6]. They attributed this to several reasons, including the fact that there is no risk of damaging the carotid sinus nerve with CAS, and that stent expansion increases the tension on the carotid artery baroreceptors. However, the medium-term effects of CAS are unclear because the carotid artery baroreceptor tension may decrease as the arterial wall reconstructs and atherosclerosis may progress after stenting. Although only three CAS cases were enrolled in this study and its effects cannot be evaluated statistically, all had an increased H/M ratio or decreased LF/HF ratio. Therefore, we expect that CAS has the potential to decrease CSNA, as well as CEA. The novelty of our study was the combined use of 123I-MIBG scintigraphy to assess CSNA and the medium-term effects of the procedure at 3 months postoperatively. While use of the LF/HF ratio for direct assessment of CSNA is controversial [21, 22], it is widely accepted as a measure of CSB reflex sensitivity and is an important indicator of the effect of CAR on efficacy. Our results suggest that CAR decreases CSNA by first removing the carotid plaque just below the carotid sinus, which improves the carotid sinus wall extensibility, as reported previously [7]. In addition, the proximal release of CS, such as in the common carotid artery, increases the pulse pressure in the carotid sinus. The increased cerebral blood flow due to revascularization may also have an effect. Recent studies have shown that a decrease in cerebral blood flow activates the sympathetic nervous system in patients with orthostatic tachycardia syndrome [23]. Paradoxically, an increase in cerebral blood flow may inhibit the sympathetic nervous system.
In echocardiography, the LVEF decreased after CAR, but within the normal range; the three patients with a reduction of more than 10% had a hyper-contracted LVEF exceeding 70% preoperatively. Interestingly, we found that the e’ wave increased and E/e’ decreased. E/e’ is not affected by LVEF and correlates well with left atrial pressure, so it is considered helpful in diagnosing heart failure. The elevated E/e’ and decreased e’ wave are also indicators of left ventricular diastolic dysfunction are used to assess the heart failure preserved ejection fraction (HFpEF) [24, 25]. Seven patients enrolled in this study had left ventricular diastolic dysfunction with E/e’ > 14.0 and e’ < 7.0; surprisingly, six had E/e’ normalization after CAR. HFpEF is associated with various pathological conditions and is related to CSNA [26]. In hypertensive patients, cardiac sympathetic hyperactivity may lead not only to elevated blood pressure, but also to the development of left ventricular diastolic dysfunction [27]. If CAR decreases CSNA, left ventricular diastolic dysfunction may be improved in HFpEF patients with carotid artery stenosis.
In contrast, we did not find any beneficial effects of CAR in lowering blood pressure. Unexpectedly, the mean 24-h and nighttime blood pressures remained unchanged. Nocturnal systolic BP reduction pattern was also unaltered except all three patients who were risers preoperatively changed to dippers or non-dippers postoperatively. The results agree with the previous report described by Demirci et al although they limited the observation to acute phase (about 4 days), in which they could not find the significant changes in systolic and diastolic blood pressures after CAR despite a decrease in the LF/HF ratio [6]. Possible explanations for the discrepancy on the sympathoinhibitory effects of CAR between heart and peripheral arteries are as follows. In the first place, the blood pressure is controlled by not only CSB reflex but also a variety of vasoactive substances including the renin-angiotensin-aldosterone system, antidiuretic hormone, and atrial natriuretic peptide [28, 29], which might change and influence blood pressure levels after CAR. Likewise, the previous study mainly focused on the effects of BAT on ambulatory blood pressure in patients with resistant hypertension has shown that approximately half of the patients treated with BAT had no decrease in ABPM [30]. These findings imply that different regulatory factors other than CSB reflex involve in the blood pressure control. It is interesting to follow up this point further, but that is beyond the scope of this paper. Second, in our study, the preoperative ABPM measurements were performed under conditions of inpatient monitoring, while the follow-up ABPM measurements were performed in an outpatient setting. A variety of the environmental and lifestyle factors [31, 32], including physical activities, salt intake, ambient temperature and medication adherence in the outpatient setting may have also affected blood pressure after CAR. At present, we have no clear answer regarding this important issue. Further studies are needed to determine the effects of CAR on mean and nocturnal blood pressure.
Study limitations
This study had several limitations. First, relatively few subjects were evaluated; therefore, the statistical validity of the results may be low. Second, although the initial examinations were performed in the hospital, the 3-month follow-up examinations were performed on an outpatient basis, which may have affected the results, particularly for ABPM and Holter ECG. In addition, the longer-term effects are unknown because follow-up after 3 months postoperatively was not possible in this study. Third, we did not examine the influence of the environmental and lifestyle factors on blood pressure after CAR. It was too complicated to be examined in detail here.
Conclusions
CAR in patients with CS may lead to medium-term improvement in CSNA and left ventricular diastolic dysfunction.
Acknowledgments
We thank the neurosurgeons from Akita University School of Medicine who supported the surgical procedure and data collection.
Financial Disclosure
This study was supported by Grants for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan (18K15878).
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
All subjects provided written informed consent.
Author Contributions
Tsukasa Kato: concept design, data collection, data analysis, and manuscript draft; Wakana Sato: concept design, data collection, data analysis, and manuscript revision; Teruki Sato: data collection, data analysis, and manuscript revision; Hiroaki Shimizu: concept design and data collection; Hiroyuki Watanabe: concept design, data analysis and manuscript revision. All authors give final approval of this manuscript and agree to be accountable for all aspects of the work.
Data Availability
The authors declare that data supporting the findings of this study are available from the corresponding author on request.
| References | ▴Top |
- Lohmeier TE, Irwin ED, Rossing MA, Serdar DJ, Kieval RS. Prolonged activation of the baroreflex produces sustained hypotension. Hypertension. 2004;43(2):306-311.
doi pubmed - Todoran TM, Zile MR. Neuromodulation device therapy for treatment of hypertensive heart disease. Circ J. 2013;77(6):1351-1363.
doi pubmed - Abraham WT, Zile MR, Weaver FA, Butter C, Ducharme A, Halbach M, Klug D, et al. Baroreflex Activation Therapy for the Treatment of Heart Failure With a Reduced Ejection Fraction. JACC Heart Fail. 2015;3(6):487-496.
doi pubmed - Funakoshi K, Hosokawa K, Kishi T, Ide T, Sunagawa K. Striking volume intolerance is induced by mimicking arterial baroreflex failure in normal left ventricular function. J Card Fail. 2014;20(1):53-59.
doi pubmed - Yuan Y, Liao SY, Xin WQ. Carotid endarterectomy should be performed early or delayed in patients with symptomatic carotid stenosis? Clin Neurol Neurosurg. 2020;199:106317.
doi pubmed - Demirci M, Saribas O, Uluc K, Cekirge S, Boke E, Ay H. Carotid artery stenting and endarterectomy have different effects on heart rate variability. J Neurol Sci. 2006;241(1-2):45-51.
doi pubmed - Angell-James JE, Lumley JS. The effects of carotid endarterectomy on the mechanical properties of the carotid sinus and carotid sinus nerve activity in atherosclerotic patients. Br J Surg. 1974;61(10):805-810.
doi pubmed - Hirschl M, Kundi M, Hirschl MM, Liebisch B, Magometschnigg D. Blood pressure responses after carotid surgery: relationship to postoperative baroreceptor sensitivity. Am J Med. 1993;94(5):463-468.
doi - Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, Bajwa TK, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004;351(15):1493-1501.
doi pubmed - Martins da Silva MI, Vidigal Ferreira MJ, Morao Moreira AP. Iodine-123-metaiodobenzylguanidine scintigraphy in risk stratification of sudden death in heart failure. Rev Port Cardiol. 2013;32(6):509-516.
doi pubmed - Kasama S, Toyama T, Sumino H, Nakazawa M, Matsumoto N, Sato Y, Kumakura H, et al. Prognostic value of serial cardiac 123I-MIBG imaging in patients with stabilized chronic heart failure and reduced left ventricular ejection fraction. J Nucl Med. 2008;49(6):907-914.
doi pubmed - Zhou W, Chen J. I -123 metaiodobenzylguanidine imaging for predicting ventricular arrhythmia in heart failure patients. J Biomed Res. 2013;27(6):460-466.
- Kasama S, Toyama T, Kumakura H, Takayama Y, Ichikawa S, Suzuki T, Kurabayashi M. Effects of nicorandil on cardiac sympathetic nerve activity after reperfusion therapy in patients with first anterior acute myocardial infarction. Eur J Nucl Med Mol Imaging. 2005;32(3):322-328.
doi pubmed - Boogers MJ, Borleffs CJ, Henneman MM, van Bommel RJ, van Ramshorst J, Boersma E, Dibbets-Schneider P, et al. Cardiac sympathetic denervation assessed with 123-iodine metaiodobenzylguanidine imaging predicts ventricular arrhythmias in implantable cardioverter-defibrillator patients. J Am Coll Cardiol. 2010;55(24):2769-2777.
doi pubmed - Merlet P, Valette H, Dubois-Rande JL, Moyse D, Duboc D, Dove P, Bourguignon MH, et al. Prognostic value of cardiac metaiodobenzylguanidine imaging in patients with heart failure. J Nucl Med. 1992;33(4):471-477.
- Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17(3):354-381.
- J. C. S. Joint Working Group. Guidelines for the clinical use of 24 hour ambulatory blood pressure monitoring (ABPM) (JCS 2010): - digest version. Circ J. 2012;76(2):508-519.
doi pubmed - Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38(4):852-857.
doi pubmed - Landesberg G, Adam D, Berlatzky Y, Akselrod S. Step baroreflex response in awake patients undergoing carotid surgery: time- and frequency-domain analysis. Am J Physiol. 1998;274(5):H1590-1597.
doi pubmed - Sigaudo-Roussel D, Evans DH, Naylor AR, Panerai RB, London NL, Bell P, Gaunt ME. Deterioration in carotid baroreflex during carotid endarterectomy. J Vasc Surg. 2002;36(4):793-798.
doi - Goldstein DS, Bentho O, Park MY, Sharabi Y. Low-frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Exp Physiol. 2011;96(12):1255-1261.
doi pubmed - Martelli D, Silvani A, McAllen RM, May CN, Ramchandra R. The low frequency power of heart rate variability is neither a measure of cardiac sympathetic tone nor of baroreflex sensitivity. Am J Physiol Heart Circ Physiol. 2014;307(7):H1005-1012.
doi pubmed - Del Pozzi AT, Schwartz CE, Tewari D, Medow MS, Stewart JM. Reduced cerebral blood flow with orthostasis precedes hypocapnic hyperpnea, sympathetic activation, and postural tachycardia syndrome. Hypertension. 2014;63(6):1302-1308.
doi pubmed - Pieske B, Tschope C, de Boer RA, Fraser AG, Anker SD, Donal E, Edelmann F, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. 2019;40(40):3297-3317.
doi pubmed - Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, 3rd, Dokainish H, Edvardsen T, Flachskampf FA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29(4):277-314.
doi pubmed - Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: Part II: causal mechanisms and treatment. Circulation. 2002;105(12):1503-1508.
doi pubmed - Grassi G, Seravalle G, Quarti-Trevano F, Dell'Oro R, Arenare F, Spaziani D, Mancia G. Sympathetic and baroreflex cardiovascular control in hypertension-related left ventricular dysfunction. Hypertension. 2009;53(2):205-209.
doi pubmed - Nishikimi T, Maeda N, Matsuoka H. The role of natriuretic peptides in cardioprotection. Cardiovasc Res. 2006;69(2):318-328.
doi pubmed - Munoz-Durango N, Fuentes CA, Castillo AE, Gonzalez-Gomez LM, Vecchiola A, Fardella CE, Kalergis AM. Role of the renin-angiotensin-aldosterone system beyond blood pressure regulation: molecular and cellular mechanisms involved in end-organ damage during arterial hypertension. Int J Mol Sci. 2016;17(7):797.
doi pubmed - Wallbach M, Lehnig LY, Schroer C, Luders S, Bohning E, Muller GA, Wachter R, et al. Effects of Baroreflex Activation Therapy on Ambulatory Blood Pressure in Patients With Resistant Hypertension. Hypertension. 2016;67(4):701-709.
doi pubmed - Cappelleri C, Janoschka A, Berli R, Kohler S, Braun-Dullaeus RC, Heuss LT, Wolfrum M. Twenty-four-hour ambulatory blood pressure monitoring in very elderly patients: Comparison of in-hospital versus home follow-up results. Medicine (Baltimore). 2017;96(34):e7692.
doi pubmed - Pikilidou MI, Tsirou E, Stergiou GS, Konstas AG, Sarafidis PA, Ptinopoulou A, Hadjistavri LS, et al. Effect of hospitalization on 24-h ambulatory blood pressure of hypertensive patients. Hypertens Res. 2010;33(10):995-999.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


