| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Case Report
Volume 14, Number 2, April 2023, pages 153-157
Left Axillary Access for Transcatheter Aortic Valve Implantation in a Patient With Two Dependent Internal Mammary Artery Grafts and a Permanent Left-Sided Implanted Pacemaker
Christos Papageorgioua, b, c, Konstantinos Tampakisa, Anastasios Chronopoulosa, Vaios Tzifosa
aDepartment of Interventional and Structural Cardiology, Henry Dunant Hospital Center, Athens 115 26, Greece
bDepartment of Cardiology, Royal Brompton Hospital, London SW3 6NP, UK
cCorresponding Author: Christos Papageorgiou, Department of Interventional and Structural Cardiology, Henry Dunant Hospital Center, Athens 115 26, Greece
Manuscript submitted March 11, 2023, accepted March 25, 2023, published online April 8, 2023
Short title: Left Axillary TAVI in a Nonagenarian Patient
doi: https://doi.org/10.14740/cr1495
| Abstract | ▴Top |
Transfemoral access has been established as the gold standard approach for the majority of patients undergoing transcatheter aortic valve implantation (TAVI). However, in cases with anatomical difficulties or severely diffused peripheral arterial disease, alternative vascular access may be considered such as the transaxillary approach. We present the case of a 92-year-old gentleman with exertional dyspnea due to severe symptomatic aortic stenosis and a history of peripheral femoro-femoral bypass surgery, coronary arterial bypass surgery and a permanent dual-chamber left-side implanted pacemaker. Due to the high surgical risk and the severe anatomical difficulties, the method of TAVI using the left axillary approach was opted. A 14-F vascular sheath was inserted with surgical cutdown and with fluoroscopic guidance while small injections of contrast confirmed the non-occlusive position and the patency of the left internal mammary artery (LIMA) graft. A stiff guidewire was used to cross the heavily calcified aortic valve and subsequently was placed into the left ventricle. Balloon aortic valvuloplasty was performed followed by a successful TAVI with no significant aortic regurgitation or paravalvular leak. The patient recuperated uneventfully and was discharged after 72 h. Axillary access for TAVI is a feasible option for high-risk patients with extended peripheral arteriopathy. To our knowledge this is the first case report describing the implantation of a newer type of intra-annular self-expanding valve platform in a nonagenarian patient with severe comorbidities and such a remarkable history of multiple previous interventions in the selected access site. Meticulous upfront strategy planning and efficient collaboration between specialties is of outmost importance in hybrid procedures for favorable clinical outcomes, especially in cases with challenging anatomies.
Keywords: TAVI; Transaxillary access; Valvular interventions; Aortic stenosis; Hybrid interventions
| Introduction | ▴Top |
Transaxillary approach accounts to approximately 5-10% of patients eligible for transcatheter aortic valve implantation (TAVI) [1, 2]. Patients with severe aorto-iliofemoral artery disease are considered suitable candidates; however, technical considerations arise in cases with previous surgical interventions in the thorax potentially compromising the outcome of a subsequent intervention [2, 3].
| Case Report | ▴Top |
Investigations
We report the case of an active 92-year-old male presenting with exertional dyspnea and exacerbating angina during the past 3 months. From his past medical history, he referred a peripheral femoro-femoral bypass surgery, coronary arterial bypass surgery with two internal mammary arteries (IMAs) and a dual-chamber left-sided pacemaker implantation.
On clinical examination the patient had an oxygen saturation of 94%, blood pressure of 160/70 mm Hg, heart rate 75 beats per minute (bpm) and a late weak pulse. Thorax auscultation revealed regular heart sounds with a holosystolic murmur located in the area of the aortic valve migrating to the apex and the carotids.
Diagnosis
Transthoracic echocardiogram revealed a left ventricle with normal wall thickness and dimensions, grade 1 diastolic dysfunction and diffusely impaired systolic function (ejection fraction (EF) = 30%). A calcified tricuspid aortic valve with low-flow/low-gradient aortic stenosis (peak velocity (Vmax) = 3.1 m/s, AVAi (aortic valve area (AVA) indexed for body surface area) = 0.8 cm2/m2, mean gradient = 23 mm Hg, stroke volume index (SVi) = 33.70 mL/m2) and mild atrioventricular valves regurgitations were recorded. A subsequent low-dose dobutamine stress echo study did not demonstrate adequate flow reserve.
Coronary catheterization demonstrated chronic occlusion of the proximal left anterior descending coronary artery (LAD) and left circumflex coronary artery (LCX) and a patent left internal mammary artery (LIMA) sequentially grafted to the proximal LAD and first obtuse marginal artery (OM1). Right coronary artery (RCA) was occluded, and a patent right internal mammary artery (RIMA) graft was anastomosed to the middle segment of the RCA.
Multislice computed tomography (MSCT) revealed a heavily calcified aortic valve with a calcium score of 2,200 Agatston units. The right superficial femoral artery was occluded distally, the left superficial had a significant stenosis while the femoro-femoral bypass graft was patent. The left iliofemoral artery was completely occluded and the abdominal aorta was severely calcified (Fig. 1a, b). Left subclavian artery had minor calcifications and mild tortuosity with regional mean calculated diameters of over 6 mm (Fig. 1c). The aortic root was moderately calcified with calcium in the left ventricular outflow tract (LVOT) and the aortic annulus had a derived perimeter of 23.4 mm and an area of 415.6 mm2 (Fig. 1d). The sinotubular junction had a diameter of 27 mm, the left coronary artery (LCA) height was 17.9 mm, and the RCA height was 24.8 mm. Right subclavian artery was characterized as a mildly calcified vessel with a tortuous bending course.
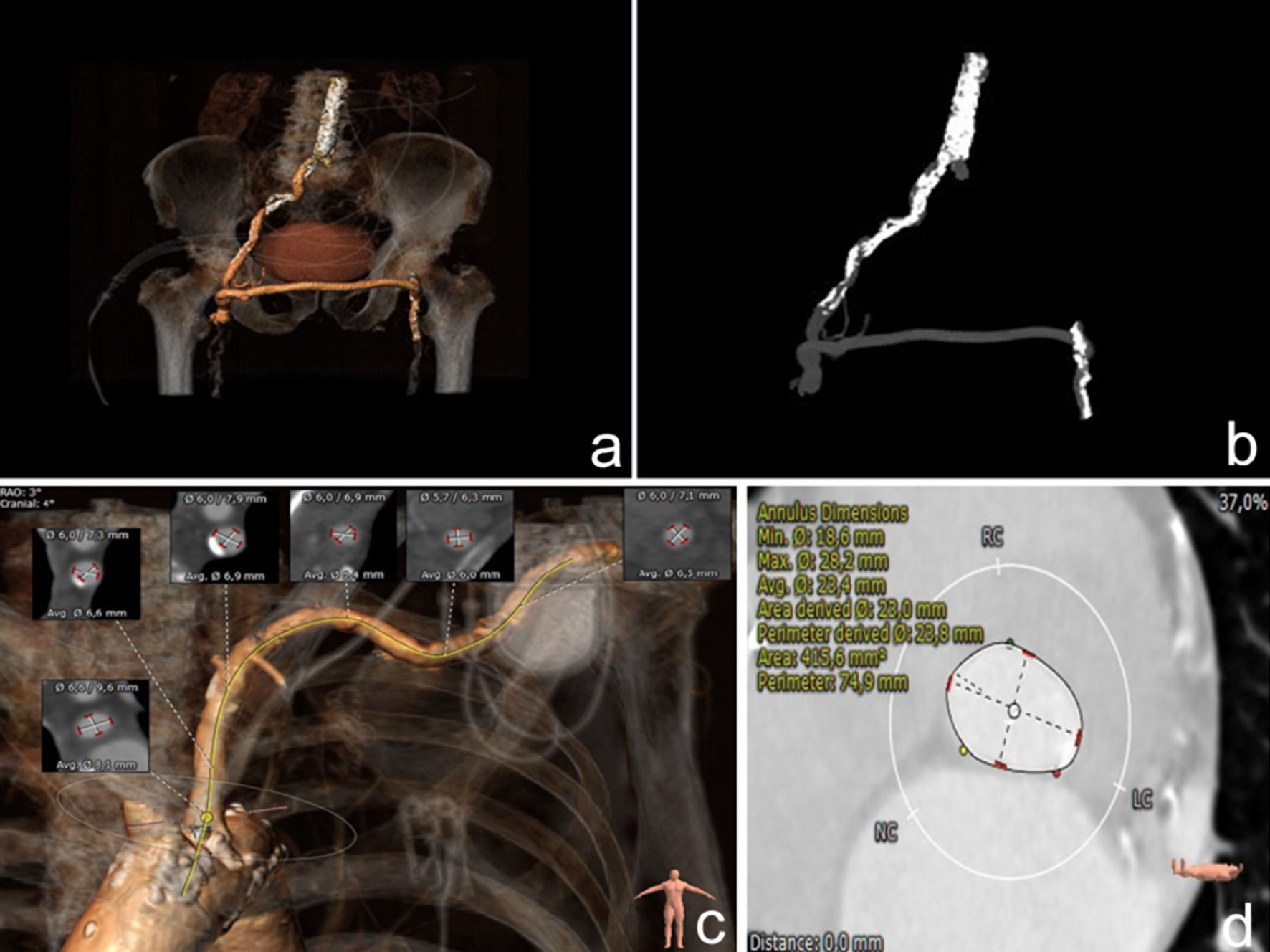 Click for large image | Figure 1. (a) Three-dimensional (3D) reconstruction of the aortoiliofemoral anatomy and (b) intravenous (IV) contrast image from MSCT scanning. Severe bilateral femoral artery disease with a patent femoro-femoral bypass graft and severe calcifications of the right aortoiliac artery and the descending aorta are displayed. (c) 3D reconstruction of the left subclavian artery anatomy and regional vessel diameters, with permanent pacemaker implanted beside the left acromioclavicular joint. (d) Aortic annulus perimeter from MSCT scanning. MSCT: multislice computed tomography. |
The case was presented to the department’s Heart Team meeting. Due to the patient’s declining clinical status and the extremely high surgical risk (Euroscore II = 43.52%), left transaxillary TAVI was opted as the most suitable approach.
The vessel was suitable for the insertion of a 14-F sheath while the calcified aortic valve was appropriate for a Navitor (Abbott, Illinois, USA) 27-mm self-expanding intra-annular valve platform with adequate radial force and compatible with the aforementioned vascular sheath diameter.
Treatment
The procedure was performed using general anesthesia. A temporary pacing lead was inserted into the right ventricle through the right femoral vein and a 5-F pigtail was positioned in the non-coronary cusp through the right femoral artery. The access to the left axillary artery was made through an 8-cm infraclavicular incision. The leads of the permanent pacemaker were detected, and care was taken not to dislodge them. The axillary artery was carefully separated from the branches of the surrounding brachial plexus and was elevated with vessel loops in order to be cannulated. The insertion point was identified, and access was established with direct puncture 4 - 5 cm distally to the origin of the left internal thoracic artery (Fig. 2a).
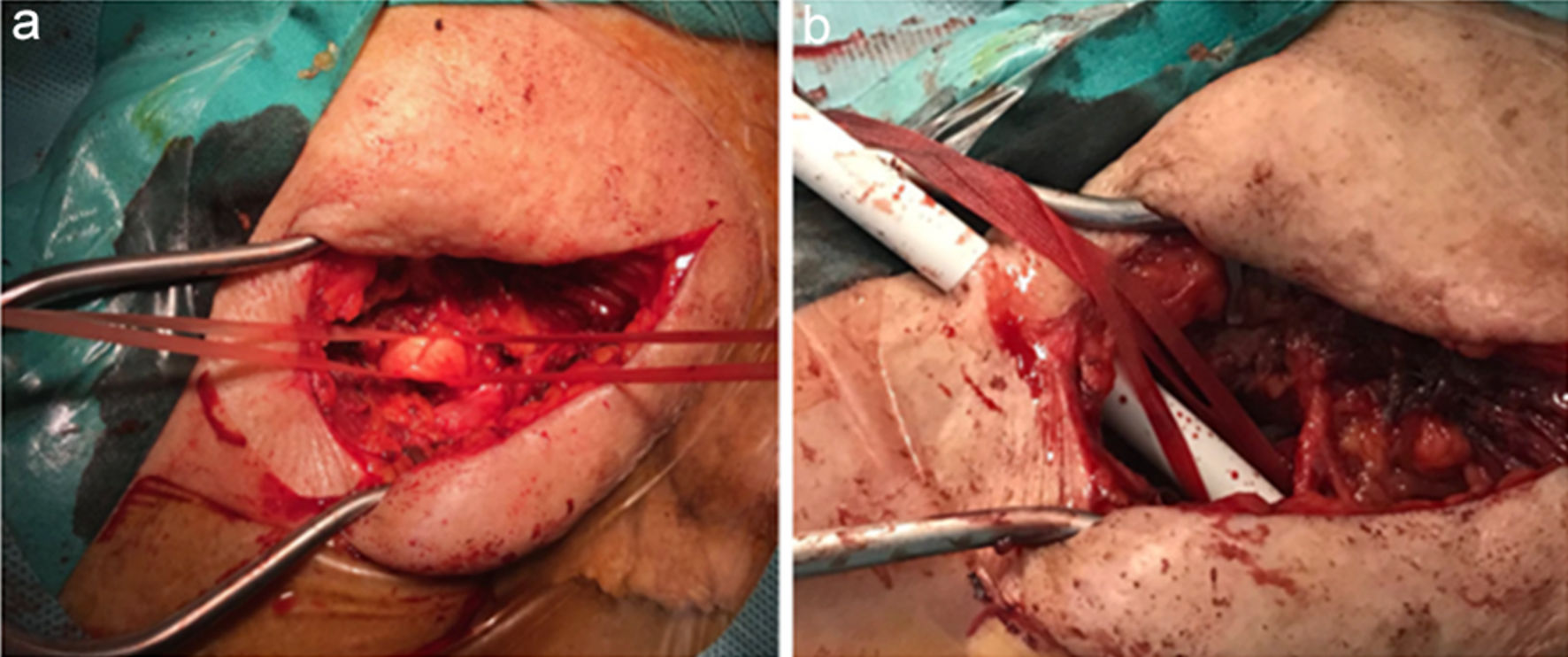 Click for large image | Figure 2. (a) Successful safe cutdown approach of the left axillary artery sparing the surrounding anatomical structures and the pacemaker/lead pocket and (b) subsequent insertion of a 14-F vascular sheath. |
A 14-F vascular sheath was inserted subsequently (Fig. 2b) under fluoroscopy and a non-occlusive position was chosen with small contrast injections confirming the patency of the LIMA graft (Fig. 3a). After successful crossing of the heavily calcified aortic valve, a stiff guide wire (Safari Small, Boston Scientific, MA, USA) was promptly positioned into the left ventricle. A 20-mm compliant balloon was used for aortic valvuloplasty and a 27-mm self-expandable transcatheter aortic valve was carefully stationed and successfully deployed at a 3-mm depth (Fig. 3b). No significant angiographic evidence of paravalvular leak and aortic regurgitation were recorded (Fig. 3c, d) as also confirmed by the bedside transthoracic echocardiogram. Pacemaker interrogation revealed normally functioning leads.
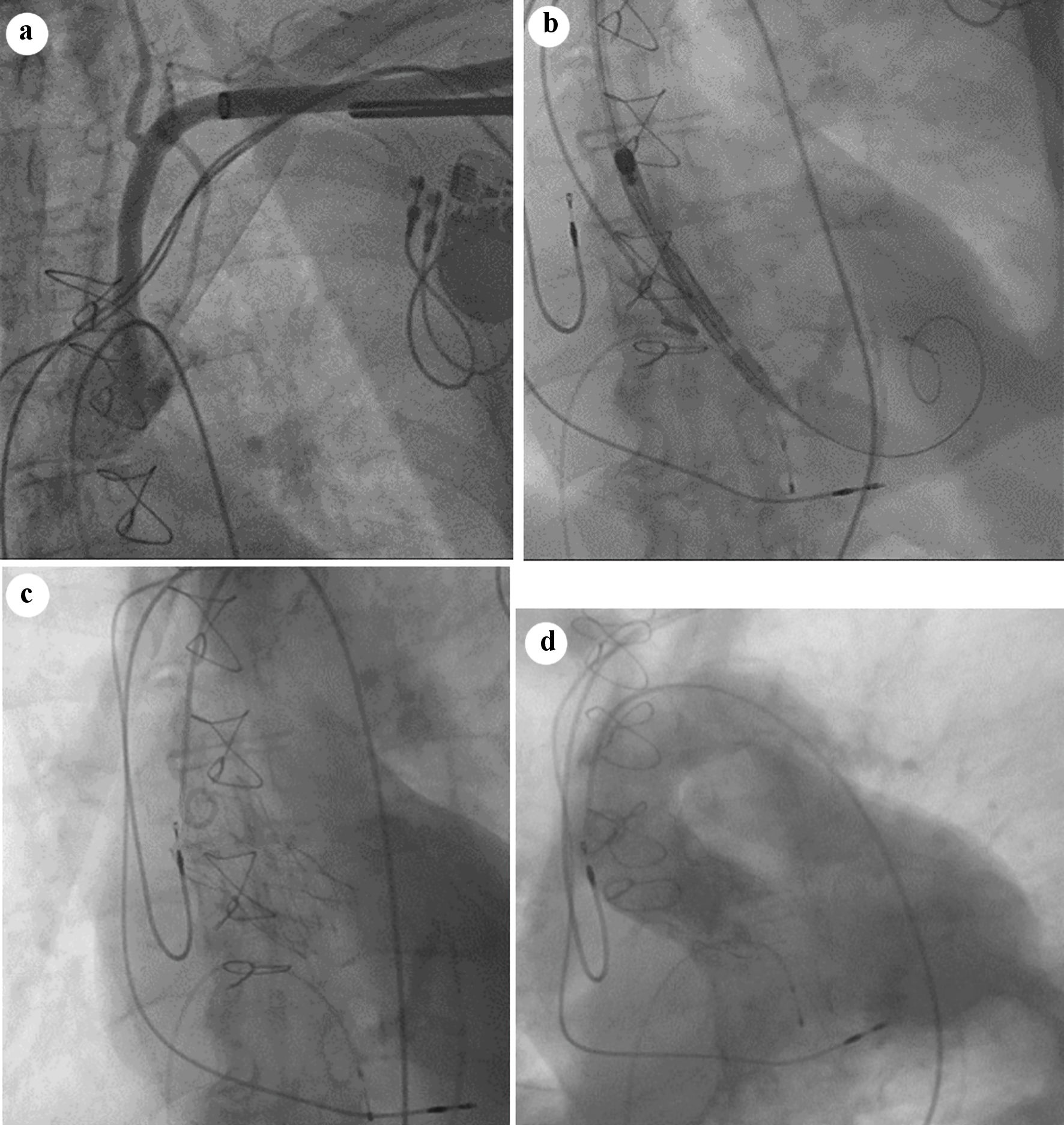 Click for large image | Figure 3. (a) Fluoroscopy injection confirming the non-occlusive position of the sheath and patency of the LIMA graft. (b) A 27-mm self-expandable transcatheter aortic valve stationed over a stiff guide wire at the level of the aortic annulus. (c) Fully expanded valve with (d) no significant angiographic tracings of aortic regurgitation and/or paravalvular leak. LIMA: left internal mammary artery. |
Follow-up and outcomes
The patient was transferred to the intensive care unit (ICU) for monitoring, recovered with no neurological deficit and was uneventfully discharged at 72 h. At the monthly follow-up appointment, he had a clinical and functional status improvement and has been scheduled for an implantable cardioverter-defibrillator (ICD) upgrade.
| Discussion | ▴Top |
Transaxillary access is considered widely as the second vascular approach option for TAVI after the transfemoral route [2-4]. Data derived from large randomized controlled TAVI trials and national registries have confirmed its non-inferiority to the transfemoral access with regards to procedural success, life-threatening bleedings, major vascular complications and comparable end points in terms of cardiovascular death and survival at 2 years [5-8].
A percutaneous approach can be implemented in carefully selected cases minimizing complications such as major bleedings and pneumothorax [9]. In our case and considering the compromised anatomy of the left subclavian area, a cutdown technique was selected as a safer technical approach.
The presence of a dependent LIMA graft, although not a contraindication for transaxillary access, can substantially jeopardize a successful procedure with detrimental effects [10]. Due to the risk of sudden occlusion by the vascular sheath and/or dissection of the axillary/subclavian arteries, related to their brittle elastic fibrous structure, careful maneuvers are required during the procedure [2, 9, 11]. Additionally, fluoroscopy guidance with minimal contrast injections, at the time of insertion of the guiding sheath, facilitates the correct positioning of the device assembly and minimizes the risk of undetected dissections.
Permanent pacemaker implantation to the ipsilateral selected access site for transaxillary TAVI provokes viable concerns regarding patient’s safety. Pacemaker and leads assembly can be damaged during the procedure. Moreover, percutaneous axillary/subclavian approach always encompasses the risk of brachial plexus injury, due to its anatomical adjacency to the axillary artery, with detrimental clinical ramifications for the patient [12-14]. Hence, we decided that a safer vascular access would be secured via cutdown while the positioning of a temporary pacing lead into the right ventricle would serve as a bailout, in case of an iatrogenic permanent pacemaker dysfunction during the procedure.
Vascular approach through the axillary artery has been corroborated to a higher rate of stroke events in comparison to the standard transfemoral access and frequently in cases with balloon expandable valve platforms [4, 15]. Implementation of cerebral vascular protection devices, especially in cases at high risk for stroke (small vessel diameters, left subclavian access, history of stroke, excessive atherosclerotic burden, vertebral artery anatomy prompting possible occlusion by the vascular sheath) is of critical importance [12]. Nevertheless, our patient displayed unfavorable right subclavian artery anatomy with a dependent RIMA graft to the RCA rendering the use of such protective device unsuitable.
Conclusions
More than two decades after the first successful implantation of a transcatheter aortic valve in humans the rapidly evolving field of TAVI offers a wide range of treatment options in patients with severe symptomatic aortic stenosis deemed at high surgical risk. Transaxillary vascular access, under circumstances, can be a safe and viable alternative option, with regards to the standard femoral approach, in cases with compromised peripheral anatomy and past interventions in the thorax.
Learning points
We demonstrated the safety of left axillary/subclavian access for TAVI in elderly patients with compromised aortoiliofemoral anatomies.
Transaxillary approach can be used with caution in cases with dependent IMA grafts and a tortuous right subclavian artery.
Previous permanent pacemaker implantation ipsilateral to the access site is not an absolute contraindication for transaxillary TAVI.
Acknowledgments
None to declare.
Financial Disclosure
No funding was received from any source for the presented work.
Conflict of Interest
The authors would like to declare no conflict of interest.
Informed Consent
Written consent was obtained from the patient.
Author Contributions
CP, VT designed the present work and contributed to data acquisition and interpretation, manuscript conceptualization, drafting and writing of the case report. KT, AC contributed to data acquisition and interpretation, drafting, and writing of the case report. All authors contributed to final review and formation of the present work.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Di Mario C, Eltchaninoff H, Moat N, Goicolea J, Ussia GP, Kala P, Wenaweser P, et al. The 2011-12 pilot European Sentinel Registry of Transcatheter Aortic Valve Implantation: in-hospital results in 4,571 patients. EuroIntervention. 2013;8(12):1362-1371.
doi - Biasco L, Ferrari E, Pedrazzini G, Faletra F, Moccetti T, Petracca F, Moccetti M. Access sites for TAVI: patient selection criteria, technical aspects, and outcomes. Front Cardiovasc Med. 2018;5:88.
doi pubmed pmc - Tagliari AP, Saadi RP, Ferrari E, Taramasso M, Saadi EK. The role of the axillary artery as a second access choice in TAVI procedures. Braz J Cardiovasc Surg. 2021;36(2):237-243.
doi pubmed pmc - Gleason TG, Schindler JT, Hagberg RC, Deeb GM, Adams DH, Conte JV, Zorn GL, 3rd, et al. Subclavian/axillary access for self-expanding transcatheter aortic valve replacement renders equivalent outcomes as transfemoral. Ann Thorac Surg. 2018;105(2):477-483.
doi - Petronio AS, De Carlo M, Bedogni F, Maisano F, Ettori F, Klugmann S, Poli A, et al. 2-year results of CoreValve implantation through the subclavian access: a propensity-matched comparison with the femoral access. J Am Coll Cardiol. 2012;60(6):502-507.
doi - Reardon MJ, Van Mieghem NM, Popma JJ, Kleiman NS, Sondergaard L, Mumtaz M, Adams DH, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321-1331.
doi - Thyregod HG, Steinbruchel DA, Ihlemann N, Nissen H, Kjeldsen BJ, Petursson P, Chang Y, et al. Transcatheter versus surgical aortic valve replacement in patients with severe aortic valve stenosis: 1-year results from the all-comers NOTION randomized clinical trial. J Am Coll Cardiol. 2015;65(20):2184-2194.
doi - Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, Tuzcu EM, Webb JG, et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015;385(9986):2477-2484.
doi - Schafer U, Ho Y, Frerker C, Schewel D, Sanchez-Quintana D, Schofer J, Bijuklic K, et al. Direct percutaneous access technique for transaxillary transcatheter aortic valve implantation: "the Hamburg Sankt Georg approach". JACC Cardiovasc Interv. 2012;5(5):477-486.
doi - Modine T, Sudre A, Collet F, Delhaye C, Lemesles G, Fayad G, Koussa M. Transcutaneous aortic valve implantation using the axillary/subclavian access with patent left internal thoracic artery to left anterior descending artery: feasibility and early clinical outcomes. J Thorac Cardiovasc Surg. 2012;144(6):1416-1420.
doi - Petronio AS, De Carlo M, Giannini C, De Caro F, Bortolotti U. Subclavian TAVI: more than an alternative access route. EuroIntervention. 2013;9(Suppl):S33-37.
doi - Bapat V, Tang GHL. Axillary/subclavian transcatheter aortic valve replacement: the default alternative access? JACC Cardiovasc Interv. 2019;12(7):670-672.
doi - Watson DR, Yakubov SJ, Lyons JM, Soto CES, Kander NH, Chapekis AT, Arshi A, et al. Trans-subclavian approach for transcatheter aortic valve replacement. Ann Cardiothorac Surg. 2017;6(5):565-567.
doi pubmed pmc - Bruschi G, Colombo P, Botta L, Nava S, Merlanti B, Belli O, Musca F, et al. Portico sheathless transcatheter aortic valve implantation via distal axillary artery. Ann Thorac Surg. 2017;103(2):e175-e177.
doi - Dahle TG, Kaneko T, McCabe JM. Outcomes following subclavian and axillary artery access for transcatheter aortic valve replacement: Society of the Thoracic Surgeons/American College of Cardiology TVT Registry Report. JACC Cardiovasc Interv. 2019;12(7):662-669.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


