| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Review
Volume 14, Number 4, August 2023, pages 243-249
Hypertrophic Cardiomyopathy: A Cardiovascular Challenge Becoming a Contemporary Treatable Disease
Stefanos G. Sakellaropoulosa, c, Benedict Schulte Steinbergb
aDepartment of Internal Medicine, Cardiology Clinic, Kantonsspital Baden, Baden, Switzerland
bDepartment of Cardiology and Angiology, Robert Bosch Hospital, Baden-Wurttemberg, Germany
cCorresponding Author: Stefanos G. Sakellaropoulos, Department of Internal Medicine, Cardiology Clinic, Kantonsspital Baden, Baden, Switzerland
Manuscript submitted May 15, 2023, accepted June 30, 2023, published online July 12, 2023
Short title: Hypertrophic Cardiomyopathy
doi: https://doi.org/10.14740/cr1514
- Abstract
- Introduction
- Pathophysiology
- Clinical Aspects
- Diagnostics
- Treatment
- Family Screening
- The Future
- Conclusions
- References
| Abstract | ▴Top |
Hypertrophic cardiomyopathy is one of the most common genetic inherited diseases of myocardium, which is caused by mutation in genes encoding proteins for the cardiac sarcomere. It is the most frequent cause of sudden death in young people and trained athletes. All diagnostic methods, including heart catheterization, transthoracic and transesophageal echocardiography, magnetic resonance imaging, genetic counseling and tissue biopsy are required for risk and therapy stratification and should be individualized depending on phenotype and genotype. Current therapy has not been tested adequately. Beta-blockers and verapamil can cause hypotension which can make hypertrophic cardiomyopathy worse. Disopyramide has been inadequately studied, and mavacamten was only studied in small trials. More definitive trials are currently ongoing. Novel invasive and noninvasive diagnostics, medical therapies, interventional and surgical approaches tend to influence the natural history of the disease, favoring a better future for this patient population.
Keywords: Hypertrophic cardiomyopathy; Obstruction; Myectomy; Alcohol ablation
| Introduction | ▴Top |
Hypertrophic cardiomyopathy (HCM) is the hypertrophy of the heart muscle of more than 15 mm, without an identifiable cause. It is the most recognized genetic cardiac disease [1]. The prevalence is 1 per 500 [2], and men are mostly affected. In young adults, it is the most common cause of sudden cardiac death (SCD) [3].
Over the last 30 years, 11 genes and more than 2,100 mutations have been identified [4]: a-tropomyosin (TPM1), cardiac troponin T (TNNT2) [5], cardiac myosin binding protein-C (MYBPC3) [6], myosin regulatory light chain (MYL2), myosin essential light chain (MYL3), cardiac troponin I (TNNI3) [7], and cardiac a-actin (ACTC1) [8]. Combined, MYBPC3 and MYH7 account for up to 50% of all patients [9].
Adrenergic overstimulation (e.g., amphetamine use) in long term can give rise to hypertrophy. However, hypertrophy, even due to apparently obvious causes, should be considered as a red flag, and a further diagnostic downstream should take place [10].
| Pathophysiology | ▴Top |
The pathophysiology of HCM is highly complex. Due to the genetic defects respectively genetic mutations in structural proteins of the smallest contractile muscle unit, the sarcomere, an unstructured reorganization of the myocyte pattern occurs long before clinical symptoms appear. This myocyte reorganization leads to a significant impairment of functional and structural properties of the cardiac myocyte [11].
By analogy with other structural heart diseases, some of which are associated with HCM, in which remodeling takes the central role in the disease process, there are three major histological components that have been described in HCM. The first is myocardial hypertrophy. Depending on the location, this leads to subaortic or midventricular obstruction associated with anterior displacement of the papillary muscles or mitral valve apparatus, inadequate coaptation, and altered pressure and flow conditions. For example, in subaortic obstruction, a direct correlation between magnitude of the pressure gradient and extent of mitral regurgitation is a measurable and visible aspect of myocyte restructuring that can often be correlated with clinical symptoms, especially under physical stress. Different is the pathology of midventricular obstruction, which is at the level of the papillary muscles and may be associated with apical infarct areas [12].
The second histologic component is fibrosis. Remodulation of the intracellular connective tissue between the myocardial fibers or myocardial ischemia may result in thinning of the myocardial wall segments, which may lead to a reduction in ejection fraction, especially in very late stages of the disease.
Furthermore, in the context of increased collagen deposition due to the mismatch between myocardial oxygen supply and demand, consecutive subendocardial or myocardial ischemia leads to the third, no less relevant histological component, so-called “small vessel disease”, which also may trigger supraventricular tachycardia. However, in addition to small vessel disease, other mechanisms such as myocardial bridging [13] or decreased coronary perfusion pressure may lead to myocardial ischemia. Of clinical significance is the hypertrophy-associated occurrence of abnormalities of the mitral valve, such as anterior displacement of mitral valve or elongated respectively altered mitral valve leaflets [14].
A distal residual anterior mitral leaflet and abnormal leaflet coaptation give rise to systolic anterior motion (SAM) and left ventricular outflow tract (LVOT) obstruction (Table 1) [1, 15]. The SAM gives rise to dynamic LVOT. This happens, because increased flow through an already narrowed LVOT along with drag forces across the leaflets, which are pulled anteriorly. Obstruction can exist at rest or upon provocative maneuvers (i.e., Valsalva, exercise, sudden upright position, amyl nitrite). Location and severity of hypertrophy are also important factors for the presence of obstruction [16].
 Click to view | Table 1. SAM-Grading and Echocardiographic Criteria |
All three histological components (myocardial hypertrophy, myocardial fibrosis, and small vessel disease) may lead to impaired diastolic function with increase of LVOT gradient, which consequently cause a dilation of left atrium and induction of supraventricular tachycardias, mostly atrial fibrillation.
Of importance, the physiological progression of diastolic dysfunction has a restrictive pattern. Based on the above-mentioned major components with the hypertrophy-associated structural and hemodynamic sequelae and considering a possible genetic predisposition, there is an increased risk for malignant ventricular arrhythmias as well as for SCD, which makes understanding the underlying pathophysiology even more significant.
Finally, abnormalities in mitral valve (elongated mitral leaflets, displacement of papillary muscles, and SAM) may be the primary pathognomonic elements, even in the absence of hypertrophy [17].
| Clinical Aspects | ▴Top |
Signs and symptoms
Symptoms are more closely associated with the severity and extent of both mitral regurgitation and diastolic dysfunction and not entirely with obstruction. Dyspnea is the most common symptom [18]. A group of patients may have increased fatigue, chest pain, palpitations and fainting or near fainting. Heart failure may develop due to diastolic impairment from severe hypertrophy that may lead to dilation of left ventricle and systolic dysfunction. Diastolic impairment can result in the development of cardiac arrhythmias such as atrial fibrillation in addition to cerebral insult from cerebral embolism, ventricular arrhythmias, chest discomfort and SCD. The postprandial state may even exacerbate symptoms of HCM due to splanchnic vasodilation, resulting in a decrease in cardiac preload [19].
Palpating the carotid pulse can help to distinguish HCM from other conditions. With HCM, the carotid upstroke is brisk. During late systole, the LVOT obstruction increases, and as a result there is a decrease in the pulse followed by a secondary increase; a finding termed a bisferiens pulse [20].
Provocation and Valsalva maneuver
Performing Valsalva maneuver leads to decrease in venous return to the right side of the heart (due to elevation of intrathoracic pressures) and therefore, a decreased filling of the left ventricle. Similar conditions that can lead to decreased filling are consumption of alcohol due to vasodilation, postprandial status, due to increased blood flow in splanchnic circulation and vasodilation, as well as standing from a squatting to upright position [21].
HCM and atrial fibrillation
Atrial fibrillation is common, with an incidence of 2% per year and prevalence of 20% (one in five patients will develop atrial fibrillation). The mortality risk accounts for 3% per year, in contrast with 1% in case of normal sinus rhythm [22]. The risk factors/clinical perspectives of developing atrial arrhythmias, which may lead to stroke or other vascular events in case of HCM are functional class III/IV at initial evaluation, history of atrial fibrillation, left atrium dimension (≥ 45 mm), outflow obstruction (≥ 30 mm Hg) and age > 60 at initial evaluation. Exploratory analyses have shown evidence for a reduction of thromboembolism with vitamin K antagonist treatment. The CHA2DS2-VASc score should not be used to assess thromboembolism risk in this population [23].
| Diagnostics | ▴Top |
Echocardiography
Maximal wall thickness > 15 mm in any myocardial segment is the criterion according to definition. In some cases, patients with positive genotype may have normal wall thickness. Assessing the hypertrophy must include the measurement of maximal wall thickness in all segments of the left ventricle from base to apex. Moreover, therapeutic strategies are largely dependent on the presence or absence of obstruction, as well as of symptoms. Approximately 30% of patients will have rest obstruction (≥ 30 mm Hg). Another 30% will have physiologic provoked gradients, e.g., after eating, and alcohol consumption [24] (< 30 mm Hg at rest and ≥ 30 mm Hg) (Fig. 1) [17]. The final one-third will have the non-obstructive form of HCM. Gradients more than 50 mm Hg represent the threshold for intervention, in case of failing to ameliorate symptoms under medications. During the last two decades, two-dimensional speckle tracking echocardiography, a new angle-independent imaging modality, has been employed for evaluating myocardial deformation indices in patients with HCM. A strong inverse correlation between left ventricular (LV) myocardial strain and the extent of myocardial fibrosis has been demonstrated [25]. Notably, the myocardial areas with the lowest regional strain values have been correlated with the greatest myocardial hypertrophy and fibrosis in HCM patients [26, 27].
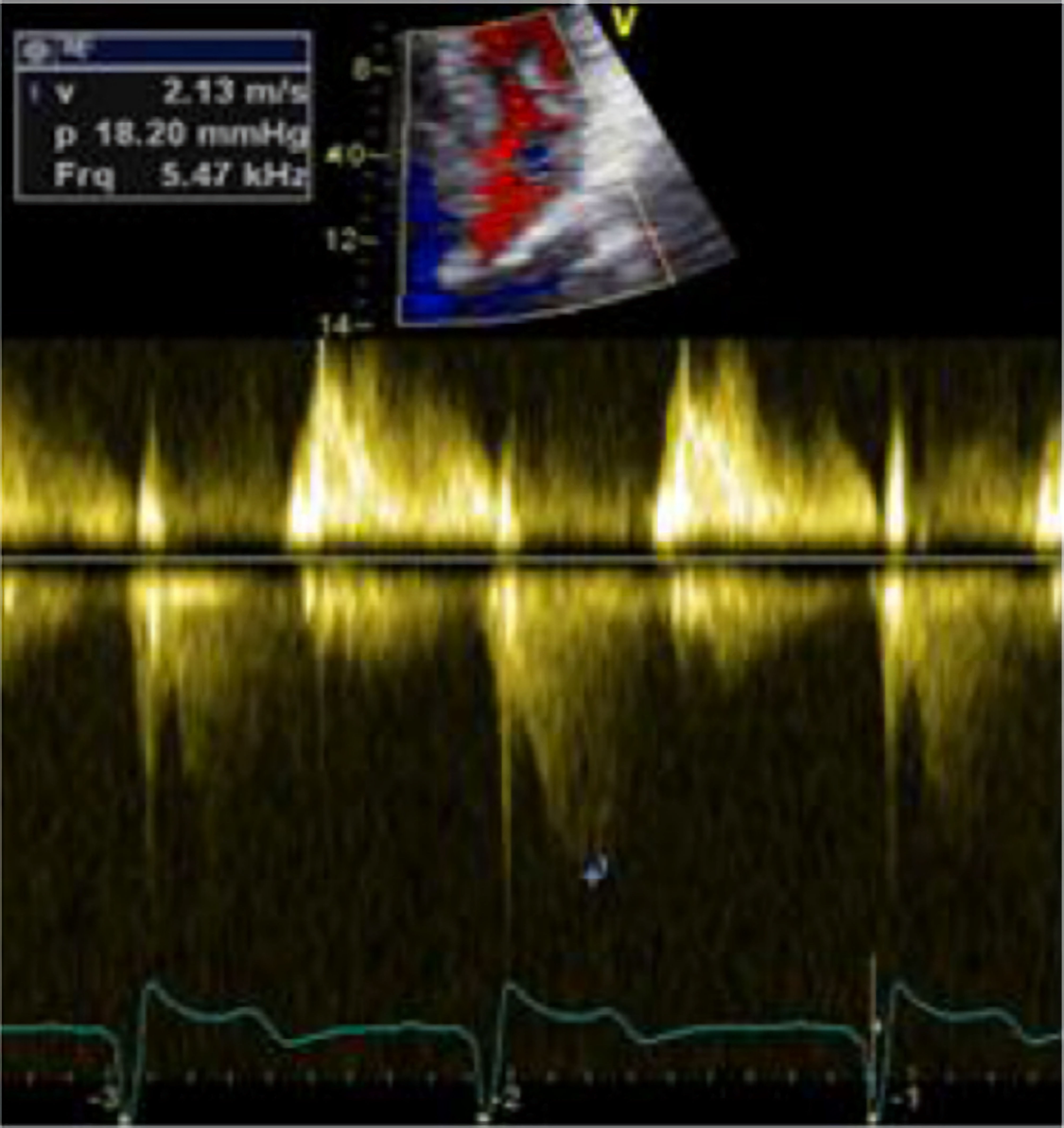 Click for large image | Figure 1. Apical four-chamber view, TTE, LVOTO with a peak gradient of 18 mm Hg without Valsalva maneuver. A typical dagger-shaped CW-signal can be appreciated. TTE: transthoracic echocardiography; LVOTO: left ventricular outflow tract obstruction; CW: continuous wave. |
Cardiac catheterization
Cardiac catheterization is mainly performed in patients who undergo alcohol septal ablation. Diagnosis or exclusion of coronary artery disease, coronary anatomy, and proper selection of the branch for alcohol injection is crucial for the evaluation and planning of a possible alcohol septal ablation. Ventriculography is not routinely performed, because sufficient information and assessment can be acquired from cardiac magnetic resonance (CMR) and echocardiography. A classic finding is the Brockenbrough-Braunwald-Morrow sign, in which the left ventricle-to-aortic gradient increases while the aortic pulse pressure decreases following premature ventricular contraction. This group of patients often has no obstructive atherosclerosis but small vessel disease, a typical histologic finding [28].
Magnetic resonance imaging (MRI)
As already mentioned, diagnosis of HCM will incorporate information obtained also from cardiac MRI. This examination provides useful means for evaluating cardiac components, cardiac structure assessment, cardiac function assessment, flow assessment, perfusion assessment, as also as highly important is the late gadolinium enhancement (LGE). Extensive assessment provides additional information for assessing SCD event risk among HCM patients [29].
Stress echocardiography
There are four main aspects of HCM, which could be assessed with stress echocardiography: 1) LVOT obstruction; 2) detection of latent systolic and diastolic dysfunction; 3) differentiating athlete’s heart vs. HCM; 4) follow-up. Exercise can provoke significant LVOT gradient in patients previously diagnosed as non-obstructive HCM with potential increase of LVOT velocity. High velocities can appear in the LVOT and are associated with basal septal hypertrophy and SAM of the mitral valve. Their appearance can be correlated closely with the development of symptoms, suggesting a potential causative link. Concerning detection of latent systolic and diastolic impairment, under stress echocardiography, there is the possibility to detect new wall motion abnormalities in 50% if left ventricular ejection fraction (LVEF) decreases (> 5%), and 16% if LVEF increases. Stress echocardiography can also detect latent systolic and diastolic dysfunction (24-44%), and detection of LV dilation and systolic dysfunction (5-year follow-up). Concerning the differentiation of athlete’s heart from HCM, through stress echocardiography, there is evidence of no LVOT gradient under exercise with increase if LVEF, as also a normal diastolic velocity in the case of an athlete’s heart [30].
| Treatment | ▴Top |
Risk stratification and treatment strategy
As a very first step, patients with diagnosed HCM should stop taking vasodilatory, increasing afterload or decreasing preload medications. Then, initiating pharmacologic therapy, such as beta-blocker, verapamil and/or disopyramide is indicated for symptom relief. These agents primarily reduce the heart rate, to increase as much as possible the preload during diastole. Beta-blockers and verapamil should first be used in the absence of non-cardiac contraindications. If there is a persistent LVOT gradient and persistent symptoms, as well as absence of contraindication of disopyramide, then adding disopyramide to a beta-blocker or to verapamil would be next step. Disopyramide is a type I antiarrhythmic drug with strong negative inotropic effect, decreases resting LVOT gradients and is efficacious in relieving symptoms in two-thirds of patients with severe obstruction. It has a IIa recommendation according to the American College of Cardiology/American Heart Association (ACC/AHA) guidelines, IIb recommendation according to European Society of Cardiology (ESC) guidelines [13]. Furthermore, they reduce the arrhythmogenic substrate of this cardiomyopathy, such as atrial fibrillation or ventricular arrhythmias. Medications that are highly contraindicated to obstructive HCM are nitrates, angiotensin-converting enzyme (ACE)-blocker or AT-II inhibitors, dihydropyridine calcium blockers, alpha blockers, PDE5 inhibitors, dobutamine, dopamine and especially digitalis, which may give rise to severe obstruction [13]. As a very last step, in case of non-response to medical therapy, surgical septal myectomy, alcohol septal ablation, DDD (dual-mode, dual-pacing, dual-sensing) pacing with short atrioventricular (AV) delay and (largely untested) mitral clip should take place [13].
Alcohol ablation vs. septal myectomy
An intraventricular/LVOT pressure gradient of minimum 50 mm Hg is considered the criterium for intervention. Over the last years, it was often questioned whether alcohol septal ablation is preferable to surgical myectomy. Several criteria have been implemented, in order to select the patient group properly for each option, such as age, comorbidities and clinical image. In the case of myectomy, younger patients are the main candidates, without other comorbidities, with need for immediate symptom relief. Septal myectomy is associated postoperatively with left bundle branch block. In the other flipside of the coin, alcohol ablation has mainly been chosen for older patients with comorbidities and more modest left ventricular hypertrophy (LVH). Alcohol ablation is associated with right bundle branch block, and postoperatively in case of high-grade AV-block with pacemaker-implantation. Percutaneous transluminal alcohol septal ablation has been increasingly preferred for septal reduction in patients with drug refractory patients. Data on medium- and long-term survival show improved prognosis with survival being like the general population. Current guidelines have supported its use by experienced operators in specialized centers [31].
| Family Screening | ▴Top |
First-degree relatives should get a screening with a detailed medical history, physical examination, electrocardiogram (ECG), and echocardiography. According to AHA guidelines, screening should start at age 12. If the child has a growth spurt or signs of puberty, is symptomatic, has activities in high-intensity sports, or there is a positive history of SCD in the family, screening should be performed earlier. The ESC recommends screening beginning at age 10. From age 12 to 18 years, a yearly screening with ECG and transthoracic echocardiography is recommended. After 18 years of age, screening can be spaced to every 5 years, in the absence of symptoms [11, 13].
| The Future | ▴Top |
Transcatheter echo-guided mitral valve repair with NeoChord implantation
Initial results with this procedure in a small number of patients indicated that transapical off-pump mitral valve repair is feasible and safe. Efficacy is maintained up to the 30-day follow-up with significant clinical benefit for patients [32].
Biomarker
Galectin-3, a prognostic biomarker, could be evolved as a prognostic tool in patients with HCM. In terms of pathophysiology, healthy myocytes are replaced with crosslinked collagen. This leads to tissue fibrosis. Levels of > 25.9 ng/mL, independent of symptoms, clinical findings, and other laboratory measures have a predictive value for identifying a high-risk patient [19].
Myosin inhibitors
Myosin inhibitors reduce the force of contraction. It has been demonstrated that mavacamten leads to stabilization of relaxation of β-cardiac myosin. Furthermore, it leads to reduction of hypertrophy, myocardial disarray, and myocardial fibrosis. Moreover, it may decrease the LVOT pressure gradient. The PIONEER-HCM trial has demonstrated that mavacamten led to decrease of pressure gradient, as well as increased peak oxygen consumption (VO2). Finally, attention should be paid to the combination with beta-blocker, verapamil or disopyramide, primarily since with myosin inhibitors, it may come to drop in LVEF and hypotension [33]. Ongoing trials may highlight this important aspect. Up to this date, to our concern, ongoing trials will enlighten a possible combination of the current medical treatment with disopyramide and myosin inhibitors.
Exercise oscillatory ventilation (EOV) and SCD
EOV (Fig. 2) [34] has a prevalence between 12% and 30%. There is also evidence that EOV occurrence is similar in diastolic (as in HCM) and systolic heart failure and provides evidence of diastolic heart failure patients at increased risk of adverse events and SCD. Although uncommon in patients with HCM, EOV appears to be a marker of disease severity and could be a potential prognostic indicator [34].
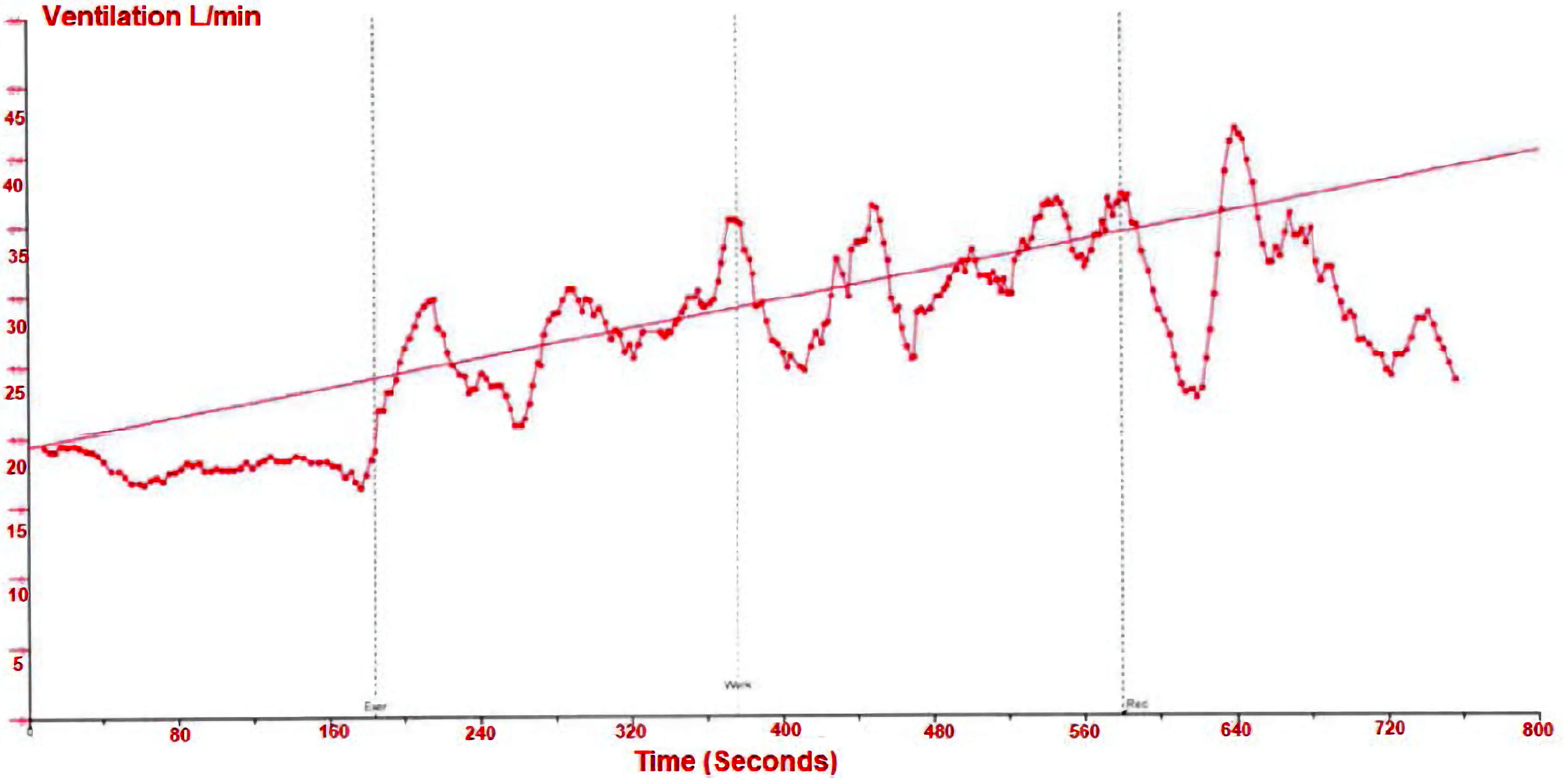 Click for large image | Figure 2. Exercise oscillatory ventilation. |
| Conclusions | ▴Top |
Almost more than half a century, after the very first description of this disease from, among others, Teare and Morrow et al [35, 36], HCM remains a challenging topic in cardiology. In the course of time, improvement of techniques, concerning imaging modalities, genetic engineering, new medical options, as well as the life-saving defibrillator-implantation therapy, continues to provide a better understanding of the natural history and pathophysiology of the disease.
There will be still difficulties and controversies to overcome, from the fact that the disease remains widely unrecognized in clinical practice, till selection of patients for treatment with septal myectomy vs. alcohol ablation or choosing the most optimal pharmaceutical agent combination or the use of biventricular pacing.
However, the upcoming years will bring improvements in all aspects. Particularly, genetic counseling will probably be the cornerstone for enlightenment of undiscovered molecular and pathophysiological mechanics.
Acknowledgments
None to declare.
Financial Disclosure
This review was not supported by any foundation, grant maker or donor.
Conflict of Interest
None to declare.
Author Contributions
Stefanos G. Sakellaropoulos contributed to the main text, article design, providing clinical expertise to revise critically. Benedict Schulte Steinberg contributed to the part of Pathophysiology.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Maron BJ. Hypertrophic cardiomyopathy: a systematic review. JAMA. 2002;287(10):1308-1320.
doi pubmed - Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary Artery Risk Development in (Young) Adults. Circulation. 1995;92(4):785-789.
doi pubmed - Maron BJ. Sudden death in young athletes. N Engl J Med. 2003;349(11):1064-1075.
doi pubmed - Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58(25):e212-260.
doi pubmed - Thierfelder L, Watkins H, MacRae C, Lamas R, McKenna W, Vosberg HP, Seidman JG, et al. Alpha-tropomyosin and cardiac troponin T mutations cause familial hypertrophic cardiomyopathy: a disease of the sarcomere. Cell. 1994;77(5):701-712.
doi pubmed - Watkins H, McKenna WJ, Thierfelder L, Suk HJ, Anan R, O'Donoghue A, Spirito P, et al. Mutations in the genes for cardiac troponin T and alpha-tropomyosin in hypertrophic cardiomyopathy. N Engl J Med. 1995;332(16):1058-1064.
doi pubmed - Brito D, Miltenberger-Miltenyi G, Vale Pereira S, Silva D, Diogo AN, Madeira H. Sarcomeric hypertrophic cardiomyopathy: genetic profile in a Portuguese population. Rev Port Cardiol. 2012;31(9):577-587.
doi pubmed - Varma PK, Neema PK. Hypertrophic cardiomyopathy: part 1 - introduction, pathology and pathophysiology. Ann Card Anaesth. 2014;17(2):118-124.
doi pubmed - Sherrid MV, Gunsburg DZ, Moldenhauer S, Pearle G. Systolic anterior motion begins at low left ventricular outflow tract velocity in obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2000;36(4):1344-1354.
doi pubmed - Misimi V, Mohammed M, Stamou K, Mitsis A, Sakellaropoulos P, Tounissidou D, Sakellaropoulos SG. Amphetamine use revealing hypertrophic cardiomyopathy in a young patient. J Med Cases. 2022;13(4):192-195.
doi pubmed pmc - Authors/Task Force Members, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733-2779.
doi pubmed - O'Mahony C, Jichi F, Pavlou M, Monserrat L, Anastasakis A, Rapezzi C, Biagini E, et al. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD). Eur Heart J. 2014;35(30):2010-2020.
doi pubmed - Fifer MA, Vlahakes GJ. Management of symptoms in hypertrophic cardiomyopathy. Circulation. 2008;117(3):429-439.
doi pubmed - Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;58(25):2703-2738.
doi pubmed - Pollick C, Morgan CD, Gilbert BW, Rakowski H, Wigle ED. Muscular subaortic stenosis: the temporal relationship between systolic anterior motion of the anterior mitral leaflet and the pressure gradient. Circulation. 1982;66(5):1087-1094.
doi pubmed - Maron BJ, Maron MS. Hypertrophic cardiomyopathy. Lancet. 2013;381(9862):242-255.
doi pubmed - Sakellaropoulos S, Svab S, Mohammed M, Dimitra L, Mitsis A. The role of mitral valve in hypertrophic obstructive cardiomyopathy: an updated review. Curr Probl Cardiol. 2021;46(3):100641.
doi pubmed - Coats CJ, Rantell K, Bartnik A, Patel A, Mist B, McKenna WJ, Elliott PM. Cardiopulmonary Exercise Testing and Prognosis in Hypertrophic Cardiomyopathy. Circ Heart Fail. 2015;8(6):1022-1031.
doi pubmed - McCullough PA, Olobatoke A, Vanhecke TE. Galectin-3: a novel blood test for the evaluation and management of patients with heart failure. Rev Cardiovasc Med. 2011;12(4):200-210.
doi pubmed - Leite JJ, Mansur AJ, de Freitas HF, Chizola PR, Bocchi EA, Terra-Filho M, Neder JA, et al. Periodic breathing during incremental exercise predicts mortality in patients with chronic heart failure evaluated for cardiac transplantation. J Am Coll Cardiol. 2003;41(12):2175-2181.
doi pubmed - Corra U, Pistono M, Mezzani A, Braghiroli A, Giordano A, Lanfranchi P, Bosimini E, et al. Sleep and exertional periodic breathing in chronic heart failure: prognostic importance and interdependence. Circulation. 2006;113(1):44-50.
doi pubmed - Pedrosa RP, Drager LF, Genta PR, Amaro AC, Antunes MO, Matsumoto AY, Arteaga E, et al. Obstructive sleep apnea is common and independently associated with atrial fibrillation in patients with hypertrophic cardiomyopathy. Chest. 2010;137(5):1078-1084.
doi pubmed - Guttmann OP, Pavlou M, O'Mahony C, Monserrat L, Anastasakis A, Rapezzi C, Biagini E, et al. Prediction of thrombo-embolic risk in patients with hypertrophic cardiomyopathy (HCM Risk-CVA). Eur J Heart Fail. 2015;17(8):837-845.
doi pubmed pmc - Musat D, Sherrid MV. Echocardiography in the treatment of hypertrophic cardiomyopathy. Anadolu Kardiyol Derg. 2006;6(Suppl 2):18-26.
pubmed - Sonaglioni A, Nicolosi GL, Rigamonti E, Lombardo M, La Sala L. Molecular approaches and echocardiographic deformation imaging in detecting myocardial fibrosis. Int J Mol Sci. 2022;23(18):10944.
doi pubmed pmc - Popovic ZB, Kwon DH, Mishra M, Buakhamsri A, Greenberg NL, Thamilarasan M, Flamm SD, et al. Association between regional ventricular function and myocardial fibrosis in hypertrophic cardiomyopathy assessed by speckle tracking echocardiography and delayed hyperenhancement magnetic resonance imaging. J Am Soc Echocardiogr. 2008;21(12):1299-1305.
doi pubmed - Kim EK, Lee SC, Hwang JW, Chang SA, Park SJ, On YK, Park KM, et al. Differences in apical and non-apical types of hypertrophic cardiomyopathy: a prospective analysis of clinical, echocardiographic, and cardiac magnetic resonance findings and outcome from 350 patients. Eur Heart J Cardiovasc Imaging. 2016;17(6):678-686.
doi pubmed - Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med. 2003;349(11):1027-1035.
doi pubmed - Chan RH, Maron BJ, Olivotto I, Pencina MJ, Assenza GE, Haas T, Lesser JR, et al. Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy. Circulation. 2014;130(6):484-495.
doi pubmed - Henein MY, O'Sullivan C, Sutton GC, Gibson DG, Coats AJ. Stress-induced left ventricular outflow tract obstruction: a potential cause of dyspnea in the elderly. J Am Coll Cardiol. 1997;30(5):1301-1307.
doi pubmed - Rigopoulos AG, Seggewiss H. Twenty years of alcohol septal ablation in hypertrophic obstructive cardiomyopathy. Curr Cardiol Rev. 2016;12(4):285-296.
doi pubmed pmc - Colli A, Manzan E, Rucinskas K, Janusauskas V, Zucchetta F, Zakarkaite D, Aidietis A, et al. Acute safety and efficacy of the NeoChord proceduredagger. Interact Cardiovasc Thorac Surg. 2015;20(5):575-580; discussion 580-571.
doi pubmed - Lekaditi D, Sakellaropoulos S. Myosin Modulators: The new era of medical therapy for systolic heart failure and hypertrophic cardiomyopathy. Cardiol Res. 2021;12(3):146-148.
doi pubmed pmc - Sakellaropoulos SG, Baggish AL, Fifer MA, Lewis GD. Exercise oscillatory ventilation in hypertrophic cardiomyopathy. Curr Probl Cardiol. 2022;47(5):100911.
doi pubmed - Teare D. Asymmetrical hypertrophy of the heart in young adults. Br Heart J. 1958;20(1):1-8.
doi pubmed pmc - Morrow AG, Braunwald E. Functional aortic stenosis; a malformation characterized by resistance to left ventricular outflow without anatomic obstruction. Circulation. 1959;20(2):181-189.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


