| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 15, Number 3, June 2024, pages 129-133
Disparity in the Under-Utilization of Novel P2Y12 Inhibitors in ST-Elevation Myocardial Infarction Following Percutaneous Coronary Intervention
Chad Nicholsona, c, Maxim Zlatopolskyb, Jared Steinbergera, Jacob Alexa, Marcel Zughaiba
aDepartment of Cardiology, Ascension Providence Hospital, Southfield, MI 48075, USA
bDepartment of Cardiology, Garden City Hospital, Garden City, MI 48135, USA
cCorresponding Author: Chad Nicholson, Department of Cardiology, Ascension Providence Hospital, Southfield, MI 48075, USA
Manuscript submitted September 6, 2023, accepted May 20, 2024, published online June 25, 2024
Short title: P2Y12 Inhibitors Use in STEMI Following PCI
doi: https://doi.org/10.14740/cr1528
| Abstract | ▴Top |
Background: The most recent guidelines (European Society of Cardiology (ESC) and American College of Cardiology/American Heart Association (ACC/AHA)) all favor prasugrel/ticagrelor over clopidogrel in the setting of acute coronary syndrome (ACS). We therefore sought to investigate which P2Y12 inhibitors were being prescribed in our community hospital setting upon discharge among patients undergoing percutaneous coronary intervention (PCI) in the setting of ST-elevation myocardial infarction (STEMI).
Methods: We identified patients presenting to two Metro Detroit Michigan hospitals with STEMI between January 1, 2018, to December 31, 2021 using the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) PCI registry. The primary outcome was the choice of P2Y12 inhibitor prescribed on day of discharge following hospitalization for STEMI, and baseline characteristics were compared including race, sex and type of insurance.
Results: A total of 366 patients presented to these two Metro Detroit hospitals from January 1, 2018, to December 31, 2021. Female and non-White patients were more likely to be discharged on clopidogrel than ticagrelor or prasugrel (odds ratio (OR): 1.56, confidence interval (CI): 0.99 - 2.45, and OR: 1.43, CI: 0.91 - 2.25, respectively), however, did not reach statistical significance. Patients without private insurance presenting with STEMI were more likely to be discharged on clopidogrel (OR: 1.83, CI: 1.22 - 2.74), which did reach statistical significance in our cohort.
Conclusions: In this retrospective single-center study evaluating BMC2 registry, we demonstrate a clinically significant disparity in prescribing patterns based on insurance, with trends for disparity based on gender and ethnicity.
Keywords: Gender disparities; P2Y12 inhibitors; ST elevation myocardial infarction; Racial disparities; Socioeconomic disparities
| Introduction | ▴Top |
The treatment of ST-elevation myocardial infarction (STEMI) and specifically the use of newer generation P2Y12 inhibitors has evolved over the past 20 years. Prasugrel and ticagrelor were approved by the Food and Drug Administration (FDA) for the reduction of thrombotic cardiovascular events following percutaneous intervention in 2009 and 2011, respectively. With the proven greater efficacy of ticagrelor and prasugrel compared to clopidogrel, there has been a gradual shift of prescribing habits among interventional cardiologists. The most recent European Society of Cardiology (ESC) guidelines favor prasugrel over ticagrelor and both have greater efficacy compared to clopidogrel, with prasugrel receiving a class IIa recommendation as the preferred P2Y12 agent when feasible [1]. However, as with relatively all newer medications, their adoption has not been uniform, and in some cases, there has been a reluctance to prescribe these medications based on cost concerns or associated side effects such as intracranial bleeding (prasugrel), dyspnea (ticagrelor), and bradyarrhythmias (ticagrelor). There are also socioeconomic factors that guide prescribing patterns which have been demonstrated, as well as patient nonadherence related to higher out-of-pocket costs for ticagrelor and prasugrel [2-5]. We therefore sought to investigate which P2Y12 inhibitors were being prescribed in a single center community hospital setting upon discharge among patients undergoing percutaneous coronary intervention (PCI) in the setting of acute coronary syndrome (ACS), specifically STEMI. Our main objective was to investigate the presence of any potential gender, ethnic and insurance status disparities.
| Materials and Methods | ▴Top |
Cohort selection
We identified patients presenting to the two campuses of Ascension Providence Hospital with STEMI between January 1, 2018, and December 31, 2021 using the Blue Cross Blue Shield of Michigan Cardiovascular Consortium PCI registry, which is a collaborative consortium of healthcare providers dedicated to improving quality of care and outcomes for cardiovascular patients across the state of Michigan [6]. For this cohort, we investigated which P2Y12 inhibitors were prescribed on discharge. The study was approved by our Institutional Review Board. Ethical compliance with human/animal study is not applicable.
Outcomes
The primary outcome was the choice of P2Y12 inhibitor prescribed on day of discharge following index hospitalization for STEMI. We examined patients being discharged on clopidogrel versus the more potent P2Y12 inhibitors prasugrel and ticagrelor, comparing demographic characteristics including gender, race (Caucasian versus non-Caucasian), and type of insurance (commercial vs. CMS). We also looked at baseline characteristics such as age, weight, comorbidities, as well as if the patients were on oral anticoagulants which could affect the decision on which of the P2Y12 inhibitors was prescribed as well as duration of therapy.
Statistical analysis
We compared baseline characteristics of age, sex, race, health insurance, weight, comorbidities, and current prescription for oral anticoagulation using analysis of variance for continuous variables and Chi-square test for categorical variables. We used logistic regression to assess the association between sex, race, and type of insurance among patients receiving clopidogrel versus prasugrel or ticagrelor.
| Results | ▴Top |
A total of 366 patients were admitted between January 1, 2018, and December 31, 2021, with STEMI fulfilled inclusion criteria, and demographic characteristics are outlined in Table 1. Among those patients, 243 (66.4%) were Caucasian, 256 (70%) were male, and 288 (78.7%) had private insurance. Two hundred forty-nine (68%) patients had hypertension, and 205 (56%) had dyslipidemia. The mean age in patients receiving clopidogrel was higher than that of ticagrelor or prasugrel (65 ± 12.5 versus 60 ± 12 and 54 ± 9.9, respectively). No patients above the age of 75 received prasugrel, and only 13 patients above the age of 75 received ticagrelor. The average body mass index (BMI) among the patients receiving clopidogrel, ticagrelor and prasugrel was 30 ± 6.2 vs. 28 ± 5.4 vs. 29 ± 5.2 kg/m2, respectively. Only 18 (4.9%) patients were under 60 kg and 11 of those patients received clopidogrel, six received ticagrelor, and one was prescribed prasugrel. Thirty-six (9.8%) patients were taking oral anticoagulants, and 30 of those patients were prescribed clopidogrel compared to ticagrelor and prasugrel (Table 1).
 Click to view | Table 1. Baseline Characteristics of Patients Presenting With STEMI (From January 1, 2018 to December 31, 2021 in Our Cohort) |
On discharge, patients were more likely to be prescribed clopidogrel, 188 (51.4%) versus ticagrelor 125 (34.1%) or prasugrel 53 (14.5%). To assess the primary outcome of the study, the ticagrelor and prasugrel groups were combined as the guidelines do not give preference to one of these more potent P2Y12 inhibitors (Table 2) at the time of our publication. This was also done to improve the power of the study.
 Click to view | Table 2. Percentage of Patients Being Prescribed Clopidogrel and Ticagrelor or Prasugrel at Discharge Following Admission for STEMI |
Female patients presenting with STEMI were more likely to be discharged on clopidogrel than ticagrelor or prasugrel (odds ratio (OR): 1.56, confidence interval (CI): 0.99 - 2.45), a difference that almost reached statistical significance. Non-White patients were also more likely to be discharged on clopidogrel than ticagrelor or prasugrel (OR: 1.43, CI: 0.91 - 2.25), however, this did not reach statistical significance. Patients without private insurance presenting with STEMI were more likely to be discharged on clopidogrel (OR: 1.83, CI: 1.22 - 2.74), and this was statistically significant (Fig. 1).
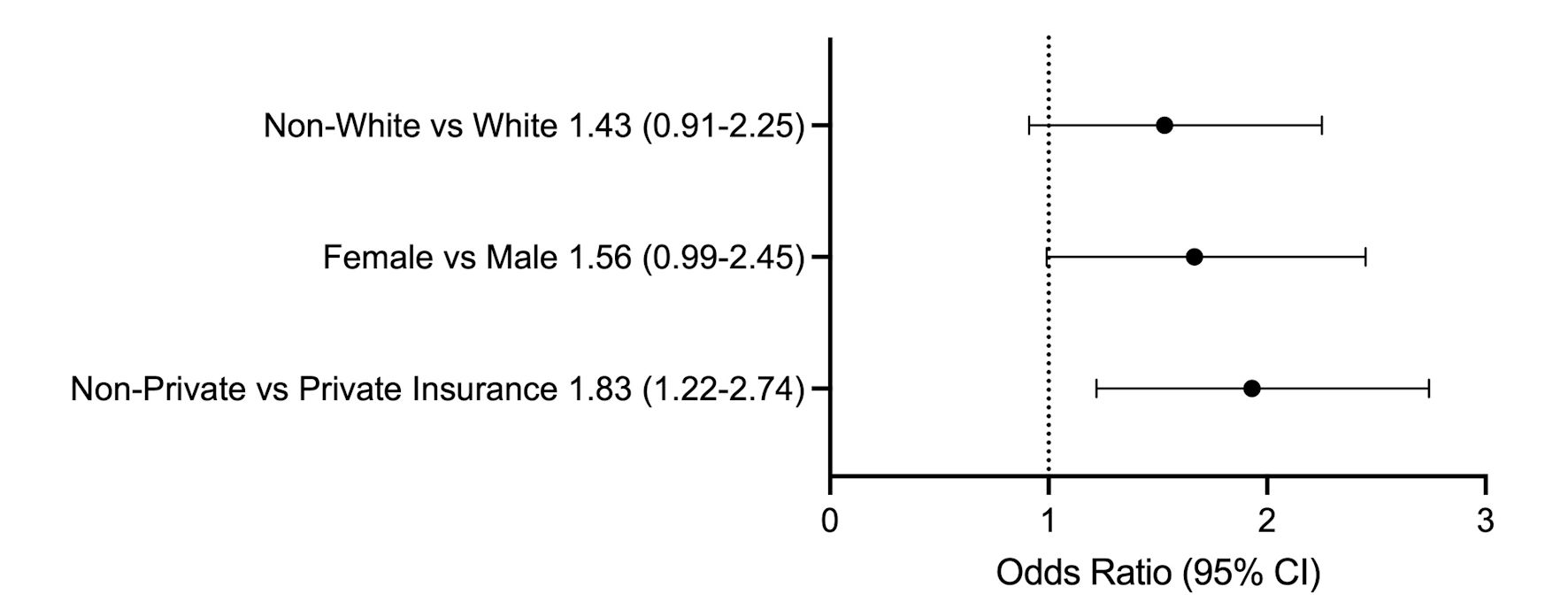 Click for large image | Figure 1. Odds ratio of being discharged on clopidogrel following STEMI. Numbers represented next to the group are odds ratio (confidence interval). STEMI: ST-elevation myocardial infarction; CI: confidence interval. |
| Discussion | ▴Top |
In the 2016 American College of Cardiology/American Heart Association (ACC/AHA) guideline-focused update on management of STEMI, a class IIa recommendation was given to the use of ticagrelor in preference to clopidogrel for maintenance P2Y12 inhibitor therapy in the setting of ACS treated with a drug-eluting stent, as well as prasugrel in preference to clopidogrel if the patient does not have high risk of bleeding complications or history of stroke/transient ischemic attack (TIA) [7]. These recommendations were based on the PLATO [7] and TRITON-TIMI 38 [8] clinical trials which showed significantly fewer ischemic complications and in-stent thrombosis, but a higher likelihood of bleeding with the newer, more potent P2Y12 inhibitors. Subsequent to the completion of our study, the updated 2023 ESC Guidelines for the Management of ACS were published and gave preference to prasugrel over ticagrelor (IIa) [1].
Using the Blue Cross Blue Shield of Michigan Cardiovascular Consortium PCI registry, patients presenting with STEMI were more likely to be discharged on clopidogrel and aspirin than the more potent P2Y12 inhibitors, prasugrel and ticagrelor. Furthermore, we found that patients without private insurance are also more likely overall to receive clopidogrel over the more potent P2Y12 inhibitors. There were strong trends, albeit not statistically significant for women and non-Caucasian to receive clopidogrel preferentially.
Because this is an observational study, it is difficult to discern prescriber rationale when deciding among P2Y12 agents. One possible hypothesis is the perceived lack of coverage or out of pocket expense reducing rates of adherence. The newer agents prasugrel and ticagrelor have historically had higher prices, especially in the context of Medicare. If patients were prescribed these newer generation medications but failed to take them due to insurance/cost restrictions, the risk of in-stent thrombosis would be higher leading to poor patient outcomes. Interestingly, the Affordability and Real-World Antiplatelet Treatment Effectiveness after Myocardial Infarction Study found a slight improvement in patient-reported medication adherence with P2Y12 agents given to patients following ACS once barriers to copayment were removed, however, no difference was found in clinical outcomes [9]. Therefore, a potential strategy to eliminate disparities given to patients without private insurance could be medication vouchers or normalization of patient co-pays.
There is an abundance of data indicating gender and racial disparities. Ya’qoub et al [10] showed that minority and female demographics are less likely to receive life-saving therapy such as revascularization and mechanical support in the setting of STEMI and cardiogenic shock and have increased odds of in-hospital mortality, compared to their Caucasian male counterparts. Harjai et al [11] looked at female patients with impaired left ventricular (LV) systolic function and found that females were less likely to receive optimal medical therapy compared to their male counterparts. Cram et al [12] reviewed patients admitted with acute myocardial infarction and found that Black patients were less likely to receive revascularization than White or Hispanic patients, and this was not explained by lack of insurance coverage [1]. Although not statistically significant, we observed a trend that female and non-White patients were more frequently discharged on clopidogrel. Another aspect is the notion of genetic polymorphisms among African Americans and P2Y12 tailoring. TAILOR-PCI did not achieve significance when implementing a genotype-guided strategy for P2Y12 inhibitor choice but had an extremely low African American demographic (about 2%) [13]. This study is balanced out by the IGNITE trial, which did achieve significance when implementing a genotype-guided approach to P2Y12 therapy and had higher recruitment of the African-American demographic (about 16%) [14]. Due to the current equipoise surrounding the clinical utility of these assays and clinical outcomes, our hospital does not use genetic testing to guide P2Y12 therapy.
There are several limitations to our study. First, because of the observational nature, it is inherently more prone to biases and confounders. Also, only one hospital system on two separate campuses in the Metro Detroit area were involved in the study, and there may be a limited number of operators who have a preference for a specific P2Y12 inhibitor. Because the data were deidentified, we were unable to screen for operators with such preference. Another limitation of the study was many patients had multiple insurances, private and non-private. An example would be a Medicare-insured patient with private secondary co-insurance. These patients were placed in the private insurance pool; however, we could not tease apart which insurance was used in securing prescription drug coverage in this cohort. And due to a lack of follow-up, we were unable to ascertain if patients prescribed a specific P2Y12 inhibitor remained on said therapy. We also did not perform sub-group analysis based on age, which would have been useful especially in the setting of decision to prescribe more potent P2Y12 inhibitors in the setting of higher HAS-BLED scores.
Conclusions
In this retrospective single-center study evaluating Blue Cross Blue Shield PCI Registry Data, we demonstrate a clinically significant disparity in prescribing patterns based on insurance, gender, and ethnicity. While our data are limited based on the retrospective nature and small sample size of our study, we believe it promotes useful dialogue and warrants further research into an important, under-researched area in the arena of cardiovascular outcomes. While previous data assessed prescribing patterns for P2Y12 antagonists, they evaluated patients prior to the updated 2016 ACC/AHA guideline-focused update on management of STEMI. Our data set begins 2 years subsequent to this guideline update, indicating that disparities and barriers persist despite the best available evidence.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable because it is a retrospective study.
Author Contributions
Chad Nicholson: writing, reviewing, editing, data collection, statistical analysis. Maxim Zlatopolsky: writing, reviewing, editing. Jared Steinberger: data collection. Jacob Alex: data collection, statistical analysis. Marcel Zughaib: reviewing, editing, and supervision.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, Claeys MJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720-3826.
doi pubmed - Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001-2015.
doi pubmed - Nathan AS, Geng Z, Eberly LA, Eneanya ND, Dayoub EJ, Khatana SAM, Kolansky DM, et al. Identifying racial, ethnic, and socioeconomic inequities in the use of novel P2Y12 inhibitors after percutaneous coronary intervention. J Invasive Cardiol. 2022;34(3):E171-E178.
pubmed pmc - Faridi KF, Garratt KN, Kennedy KF, Maddox TM, Secemsky EA, Butala NM, Yeh RW. Physician and hospital utilization of P2Y12 inhibitors in ST-segment-elevation myocardial infarction in the United States: a study from the national cardiovascular data Registry's research to practice initiative. Circ Cardiovasc Qual Outcomes. 2020;13(3):e006275.
doi pubmed - Dayoub EJ, Seigerman M, Tuteja S, Kobayashi T, Kolansky DM, Giri J, Groeneveld PW. Trends in platelet adenosine diphosphate P2Y12 receptor inhibitor use and adherence among antiplatelet-naive patients after percutaneous coronary intervention, 2008-2016. JAMA Intern Med. 2018;178(7):943-950.
doi pubmed pmc - Moscucci M, Share D, Kline-Rogers E, O'Donnell M, Maxwell-Eward A, Meengs WL, Clark VL, et al. The Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) collaborative quality improvement initiative in percutaneous coronary interventions. J Interv Cardiol. 2002;15(5):381-386.
doi pubmed - Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, et al. 2016 ACC/AHA Guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: AN UPDATe of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation. 2016;134(10):e123-155.
doi pubmed - Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
doi pubmed - Wang TY, Kaltenbach LA, Cannon CP, Fonarow GC, Choudhry NK, Henry TD, Cohen DJ, et al. Effect of medication co-payment vouchers on P2Y12 inhibitor use and major adverse cardiovascular events among patients with myocardial infarction: the ARTEMIS randomized clinical trial. JAMA. 2019;321(1):44-55.
doi pubmed pmc - Ya'qoub L, Lemor A, Dabbagh M, O'Neill W, Khandelwal A, Martinez SC, Ibrahim NE, et al. Racial, ethnic, and sex disparities in patients with STEMI and cardiogenic shock. JACC Cardiovasc Interv. 2021;14(6):653-660.
doi pubmed - Harjai KJ, Nunez E, Stewart Humphrey J, Turgut T, Shah M, Newman J. Does gender bias exist in the medical management of heart failure? Int J Cardiol. 2000;75(1):65-69.
doi pubmed - Cram P, Bayman L, Popescu I, Vaughan-Sarrazin MS. Racial disparities in revascularization rates among patients with similar insurance coverage. J Natl Med Assoc. 2009;101(11):1132-1139.
doi pubmed - Pereira NL, Farkouh ME, So D, Lennon R, Geller N, Mathew V, Bell M, et al. Effect of genotype-guided oral P2Y12 inhibitor selection vs conventional clopidogrel therapy on ischemic outcomes after percutaneous coronary intervention: the TAILOR-PCI randomized clinical trial. JAMA. 2020;324(8):761-771.
doi pubmed pmc - Cavallari LH, Lee CR, Beitelshees AL, Cooper-DeHoff RM, Duarte JD, Voora D, Kimmel SE, et al. Multisite investigation of outcomes with implementation of CYP2C19 genotype-guided antiplatelet therapy after percutaneous coronary intervention. JACC Cardiovasc Interv. 2018;11(2):181-191.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


