| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 5, October 2023, pages 370-378
Anticoagulation Use as an Independent Predictor of Mortality and Major Adverse Cardiovascular Events in Hospitalized COVID-19 Patients: A Multicenter Retrospective Analysis
Nathan DeRon Jra, d, Lawrence Hoanga, Kristopher Atena, Sri Prathivadab, Manavjot Sidhub, c
aDepartment of Internal Medicine, Methodist Dallas Medical Center, Dallas, TX, USA
bDivision of Cardiology, Methodist Dallas Medical Center, Dallas, TX, USA
cMethodist Dallas Cardiovascular Consultants, Methodist Medical Group, Dallas, TX, USA
dCorresponding Author: Nathan DeRon Jr., Department of Internal Medicine, Methodist Dallas Medical Center, Dallas, TX, USA
Manuscript submitted June 23, 2023, accepted August 7, 2023, published online August 22, 2023
Short title: AC Use in Hospitalized COVID-19 Patients
doi: https://doi.org/10.14740/cr1529
| Abstract | ▴Top |
Background: Coronavirus disease 2019 (COVID-19) is associated with increased incidence of cardiac arrhythmias and thrombotic events. The adverse cardiovascular outcomes related to ambulatory anticoagulation (AC) therapy in COVID-19 patients are unknown. The goal of this study was to identify the effects of AC use in hospitalized COVID-19 patients.
Methods: This is a multicenter, retrospective study that identified 2,801 hospitalized COVID-19 polymerase chain reaction (PCR)-positive patients admitted between March 2020 and July 2021. Of these, 375 (13.4%) were ambulatory AC users. Data were collected from the electronic health records of hospitalized patients. Mortality included in-hospital death and hospice referral. Major adverse cardiovascular events (MACEs) included acute heart failure (HF), myocardial infarction (MI), myocarditis, pulmonary embolism (PE), deep venous thrombosis (DVT), pericardial effusion, pericarditis, stroke, shock, and cardiac tamponade. A Chi-square test was used to analyze categorical variables, and multivariate logistic regression analysis was performed to account for comorbidities.
Results: AC non-users exhibited a higher incidence of mortality than AC users (13.9% vs. 7.7%, P = 0.001). However, MACE incidence was higher in AC users than AC non-users (44.8% vs. 26.8%, P < 0.001). The higher MACE incidence was driven by higher rates of acute HF (8.3% vs. 2.5%, P < 0.001), MI (26.9% vs. 18.2%, P < 0.001), PE/DVT (16.3% vs. 2.7%, P < 0.001), pericardial effusion (1.6% vs. 0.5%, P = 0.025), and stroke (2.9% vs. 1.2%, P = 0.018). After multivariate logistic regression, MACE incidence remained higher (odds ratio (OR) = 1.61, 95% confidence interval (CI): 1.27 - 2.05, P < 0.001) and all-cause mortality rate lower (OR = 0.34, 95% CI: 0.23 - 0.52, P < 0.001) in AC users.
Conclusions: Ambulatory AC use is associated with increased MACEs but decreased all-cause mortality in patients hospitalized with COVID-19. This study will help physicians identify patients at risk of cardiovascular mortality and direct management based on the identified risk.
Keywords: Anticoagulation; Mortality; Major adverse cardiac events; COVID-19; Ambulatory anticoagulation
| Introduction | ▴Top |
Cardiovascular disease is the most common cause of mortality in the world [1]. It is also associated with increased incidence of morbidity and mortality in hospitalized coronavirus disease 2019 (COVID-19) patients [2]. Additionally, COVID-19 causes inflammatory and prothrombotic states, which increase the incidence of major adverse cardiovascular events (MACEs) and cardiovascular mortality [3]. Atrial fibrillation has also been shown to increase the incidence of MACEs and cardiovascular mortality in COVID-19 patients [4]. COVID-19 has been linked to the development of new arrhythmias [5] and an overall elevated incidence of MACEs during hospitalization [6]. Also, COVID-19 patients not vaccinated against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are at increased risk of endothelial dysfunction, and therefore negative cardiovascular outcomes, compared to patients without COVID-19 and those vaccinated against SARS-CoV-2 [7]. More data are required regarding unvaccinated individuals given their elevated risk of complications from COVID-19 infection [8]. Given the prothrombotic and proarrhythmic states caused by COVID-19 and the prevalence of atrial fibrillation in the hospitalized COVID-19 population, the question of whether to provide anticoagulation (AC) therapy to this cohort of patients arose. This consideration is especially pertinent in the subgroup of patients currently compliant with ambulatory AC medications. Recent data showed AC therapy is beneficial to non-intensive care unit (ICU) COVID-19 patients, reducing their need for cardiovascular and respiratory organ support [9], as well as reducing instances of major thromboembolism and death [10]. However, there remains a shortage of data regarding cardiovascular outcomes of AC therapy in hospitalized COVID-19 patients. In this study, we aimed to determine whether hospitalized ambulatory AC users with COVID-19 are at increased risks for MACEs and all-cause mortality.
| Materials and Methods | ▴Top |
This is a multicenter, retrospective study that included 2,801 unvaccinated adults over the age of 18 years with COVID-19 confirmed by polymerase chain reaction (PCR). Patients were admitted to four hospitals within the Methodist Health System in Dallas, Texas between March 2020 and July 2021. All patients who were hospitalized and diagnosed with COVID-19 by PCR were included. Data were de-identified prior to analysis. Data abstraction was approved by WCG/Aspire Institutional Review Board (IRB) (IRB#: 20201424).
Data were collected from the electronic medical records and included demographics, vitals and symptoms on arrival, laboratory measurements, inpatient medications, comorbidities (e.g., congestive heart failure (HF), diabetes, stroke, chronic obstructive pulmonary disease (COPD), hypertension, chronic kidney disease (CKD), asthma, and hepatic cirrhosis), and outcomes including all-cause MACEs and mortality which included in-hospital death and hospice referral. MACE was defined as a composite of acute HF, myocardial infarction (MI), myocarditis, pulmonary embolism (PE), deep venous thrombosis (DVT), pericardial effusion, pericarditis, stroke, shock, and cardiac tamponade. Patients were determined to be ambulatory AC users based on outpatient medication lists and history of medication compliance.
Depending on normal variable distribution, continuous variables were characterized by either median and interquartile range or mean and standard deviation. Chi-square testing was used to analyze categorical variables. One-way analysis of variance or Kruskal-Wallis’s test was used for normal variables for multiple means or medians. Multivariate logistic regression analysis was performed to account for demographics and comorbidities such as coronary artery disease, chronic HF, stroke, diabetes, hypertension, COPD, and CKD. Base regression included variables with data available for > 90% of patients. Imputation was not performed for absent laboratory values due to the probability that those values were non-random. Statistical analysis was performed in R version 4.2.2 using the EZR package version 1.61 (Saitama Medical Center, Jichi Medical University) [11]. A P value ≤ 0.05 was considered significant.
| Results | ▴Top |
Among 2,801 patients with PCR-positive COVID-19, 375 (13.4%) were ambulatory AC users and 2,426 (86.6%) were not (Fig. 1). There was a greater proportion of males than females in both the AC users (54.4% vs. 45.6%) and AC non-users (51.7% vs. 48.3%) (Table 1). The mean age was greater (68.2 ± 15.1 vs. 60.4 ± 17.4 years, P < 0.001) and the median body mass index (BMI) was slightly lower (29.95 (25.40 - 35.10) vs. 30.00 (25.50 - 35.50) kg/m2, P = 0.826) in the AC users compared to the AC non-users. AC users had a significantly higher prevalence of coronary artery disease (21.9% vs. 13.5%, P < 0.001), CKD (20.0% vs. 14.8%, P = 0.011), COPD/asthma (21.1% vs. 15.2%, P = 0.005), diabetes (45.1% vs. 39.1%, P = 0.031), HF (28.0% vs. 12.0%, P < 0.001), hypertension (68.8% vs. 61.1%, P = 0.004), and history of stroke (12.8% vs. 8.8%, P = 0.017).
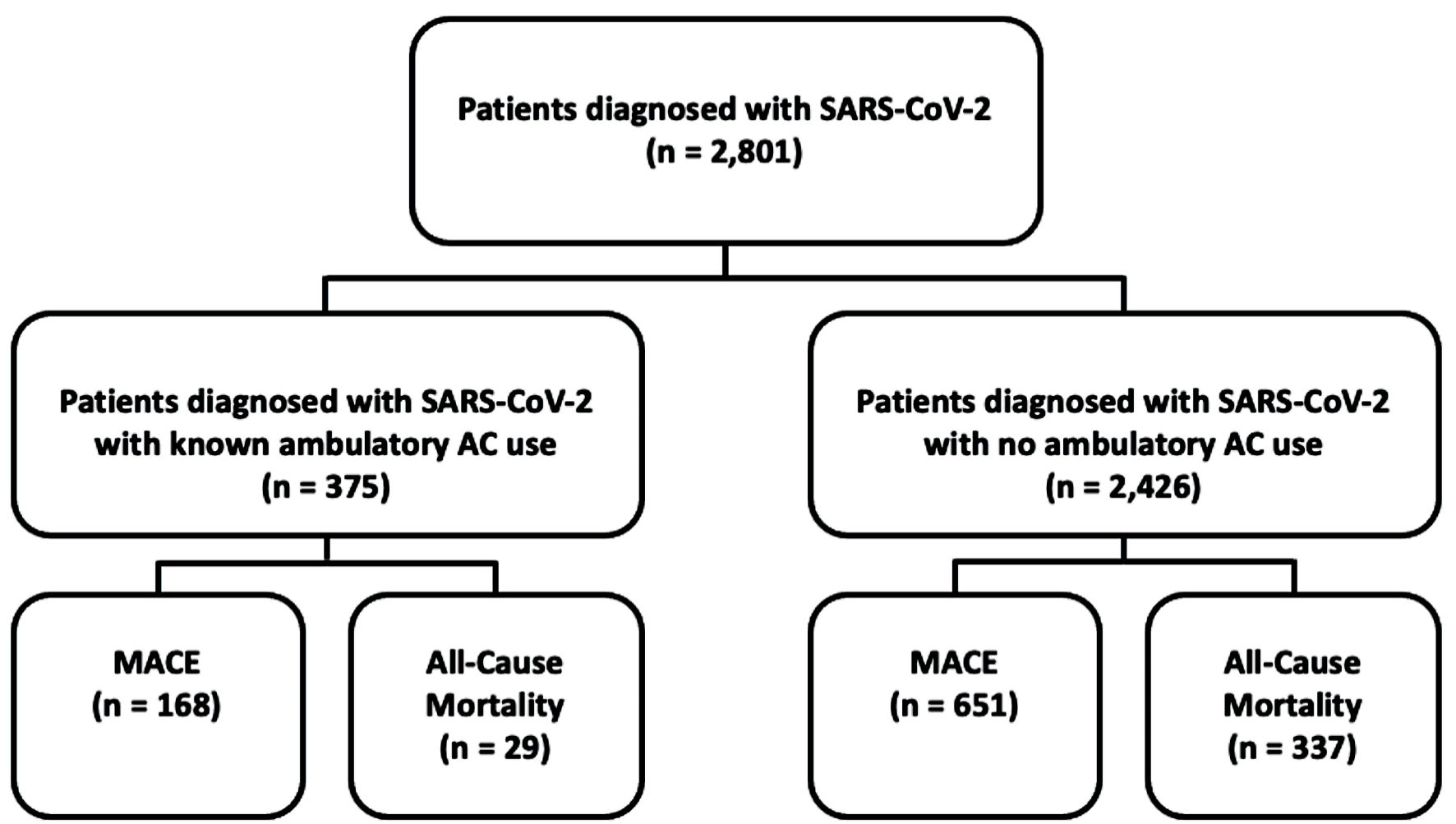 Click for large image | Figure 1. Flow chart of the study’s patient population. SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; AC: anticoagulation; MACE: major adverse cardiovascular event. |
 Click to view | Table 1. Demographics of the Study Cohort |
The incidence of MACE was higher in the AC users compared to non-users (44.8% vs. 26.8%, P < 0.001) (Fig. 2). The higher MACE incidence was driven by higher rates of acute HF (8.3% vs. 2.5%, P < 0.001) (Fig. 3), MI (27.0% vs. 18.2%, P < 0.001) (Fig. 4), PE/DVT (16.3% vs. 2.7%, P < 0.001) (Fig. 5), pericardial effusion (1.6% vs. 0.5%, P = 0.025) (Fig. 6), and stroke (2.9% vs. 1.2%, P = 0.018) (Fig. 7) in the AC user cohort. Logistic regression analysis accounting for underlying comorbidities determined that AC use was associated with increased risk of MACEs (odds ratio (OR) = 1.61, 95% confidence interval (CI): 1.27 - 2.05, P < 0.001).
 Click for large image | Figure 2. Major adverse cardiovascular event incidence by use of anticoagulation. Bars illustrate mean ± SD. MACEs: major adverse cardiovascular events; AC: anticoagulation; SD: standard deviation. |
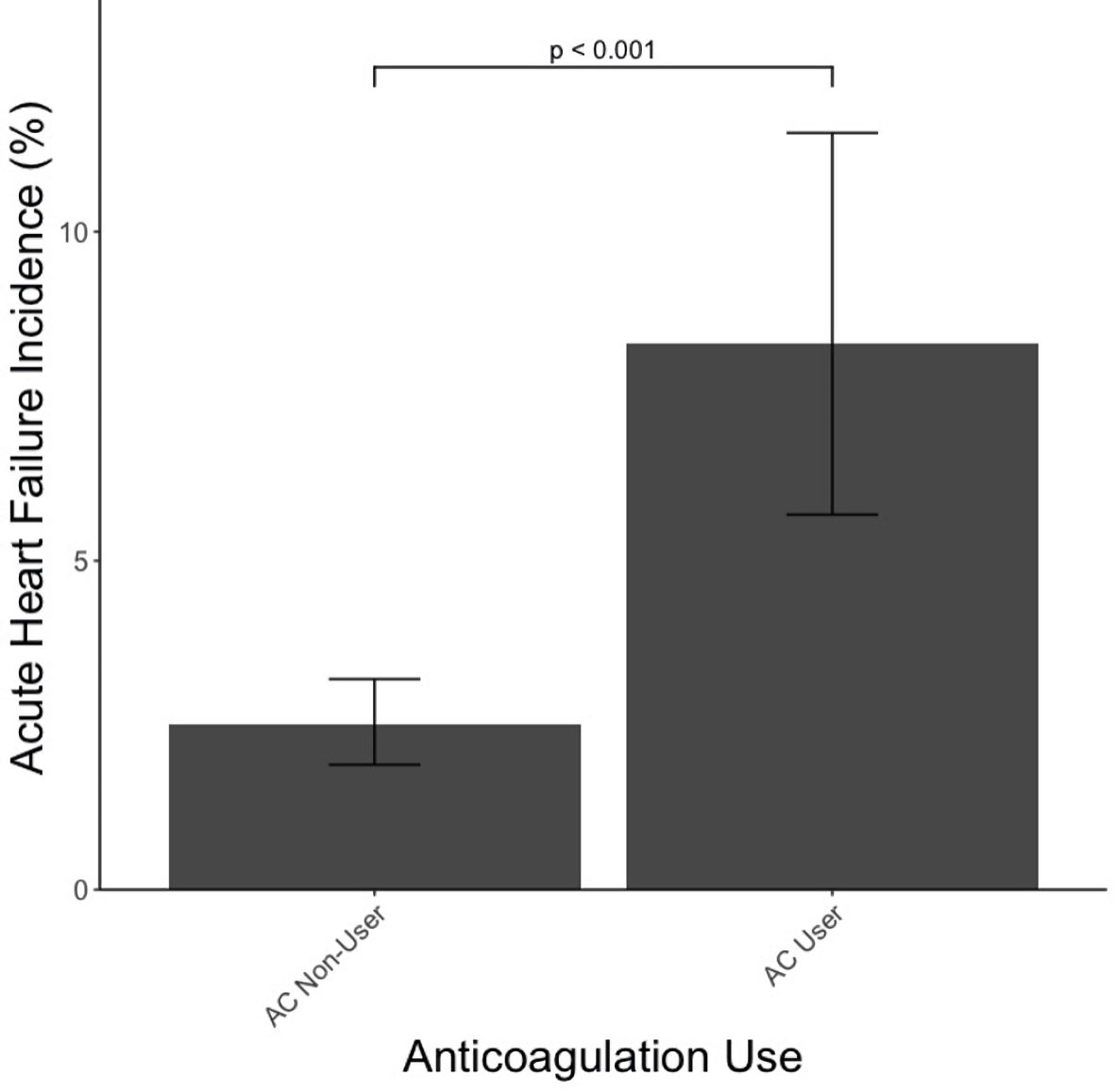 Click for large image | Figure 3. Acute heart failure incidence by use of anticoagulation. Bars illustrate mean ± SD. AC: anticoagulation; SD: standard deviation. |
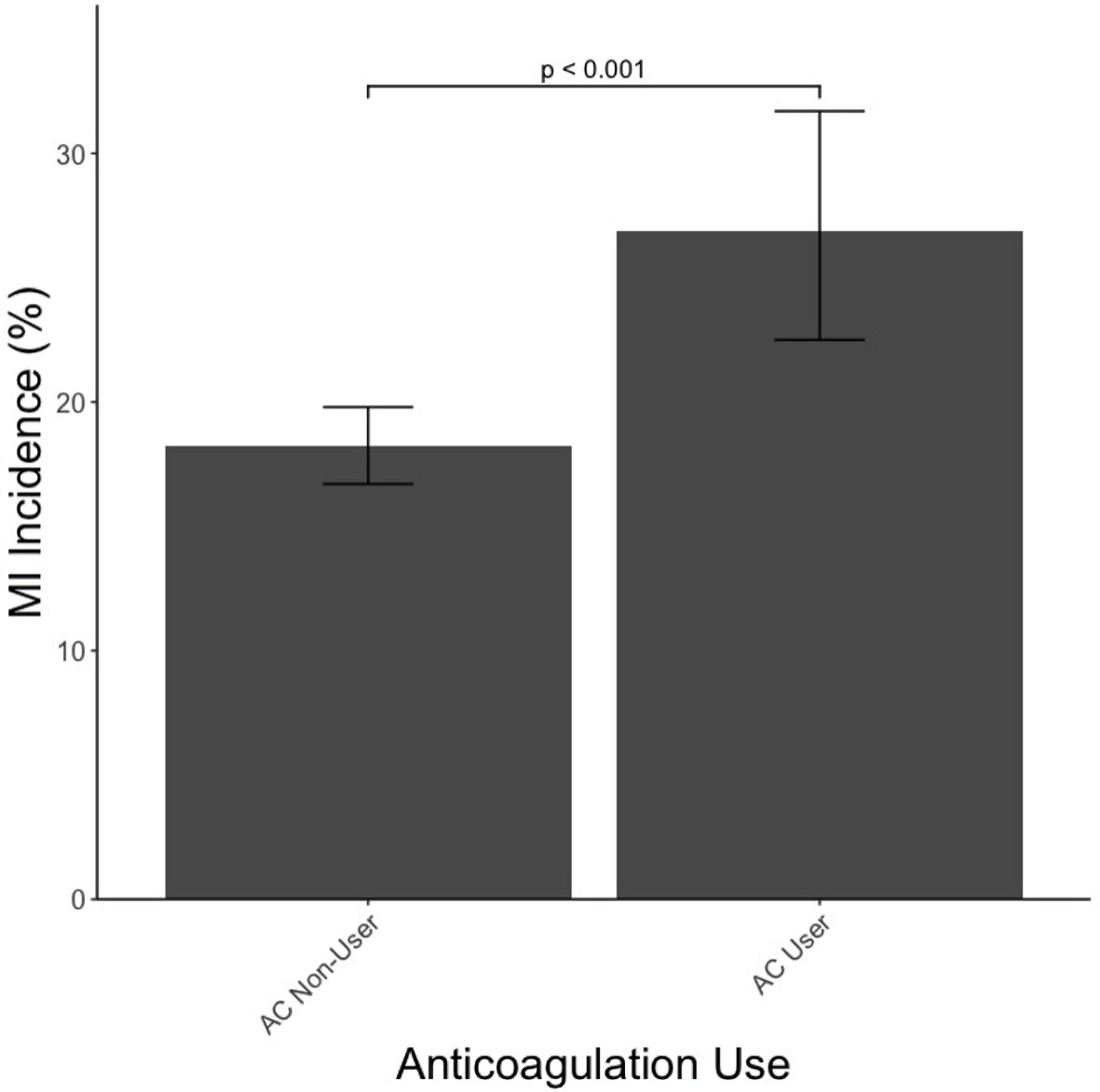 Click for large image | Figure 4. Myocardial infarction (MI) incidence by use of anticoagulation. Bars illustrate mean ± SD. AC: anticoagulation; SD: standard deviation. |
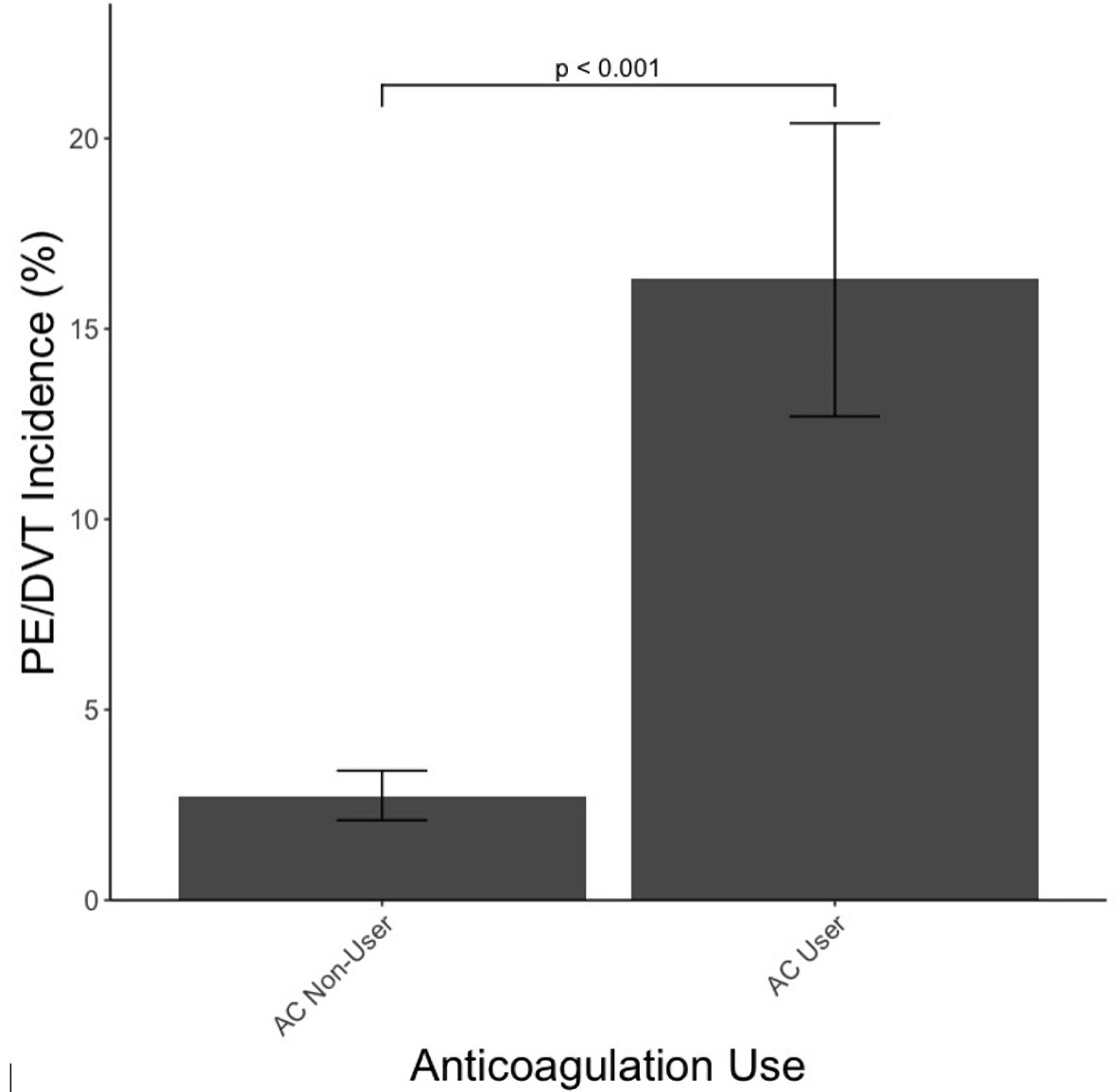 Click for large image | Figure 5. Incidence of pulmonary embolism (PE) and deep venous thrombosis (DVT) by use of anticoagulation. Bars illustrate mean ± SD. AC: anticoagulation; SD: standard deviation. |
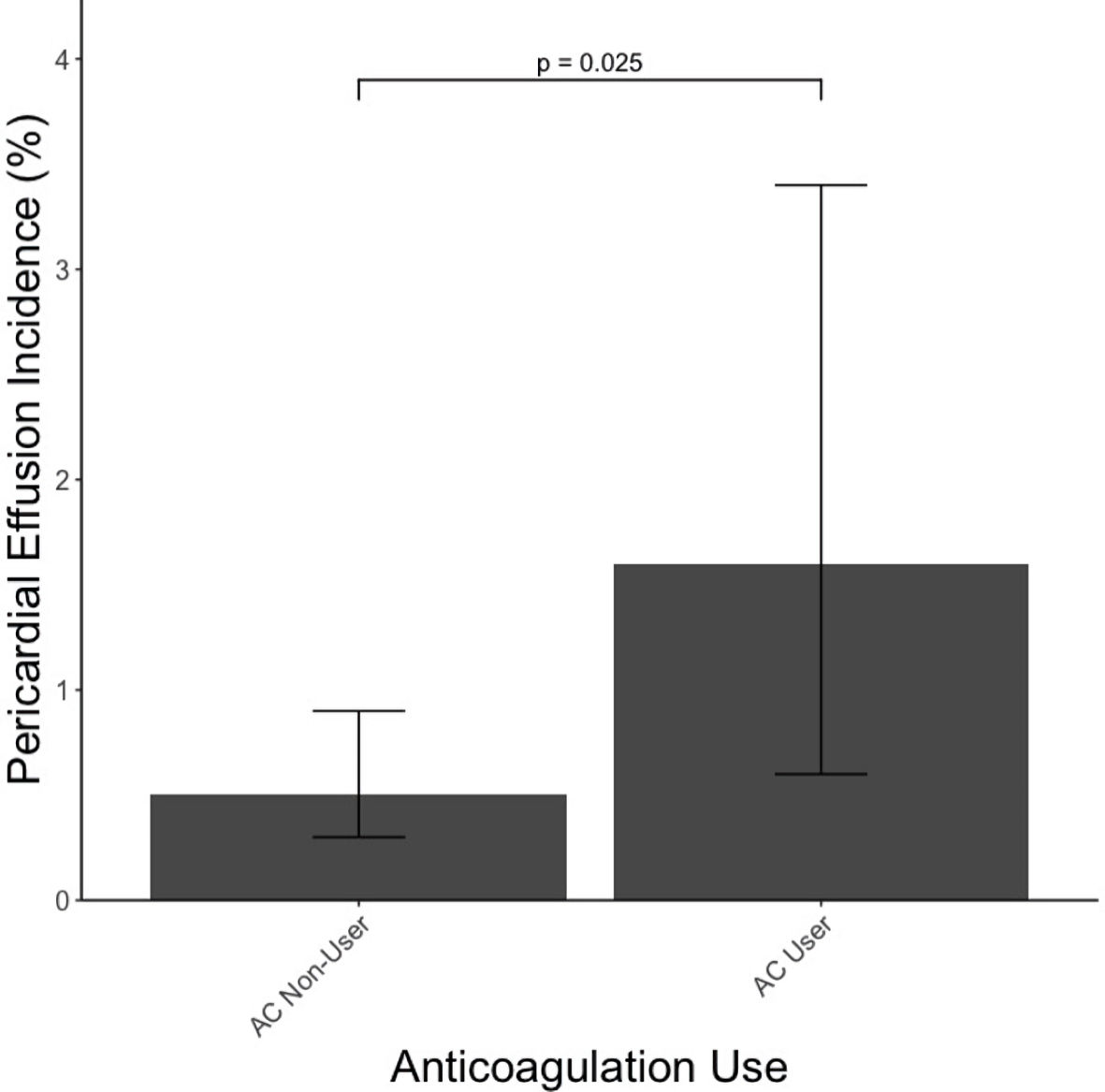 Click for large image | Figure 6. Pericardial effusion incidence by use of anticoagulation. Bars illustrate mean ± SD. AC: anticoagulation; SD: standard deviation. |
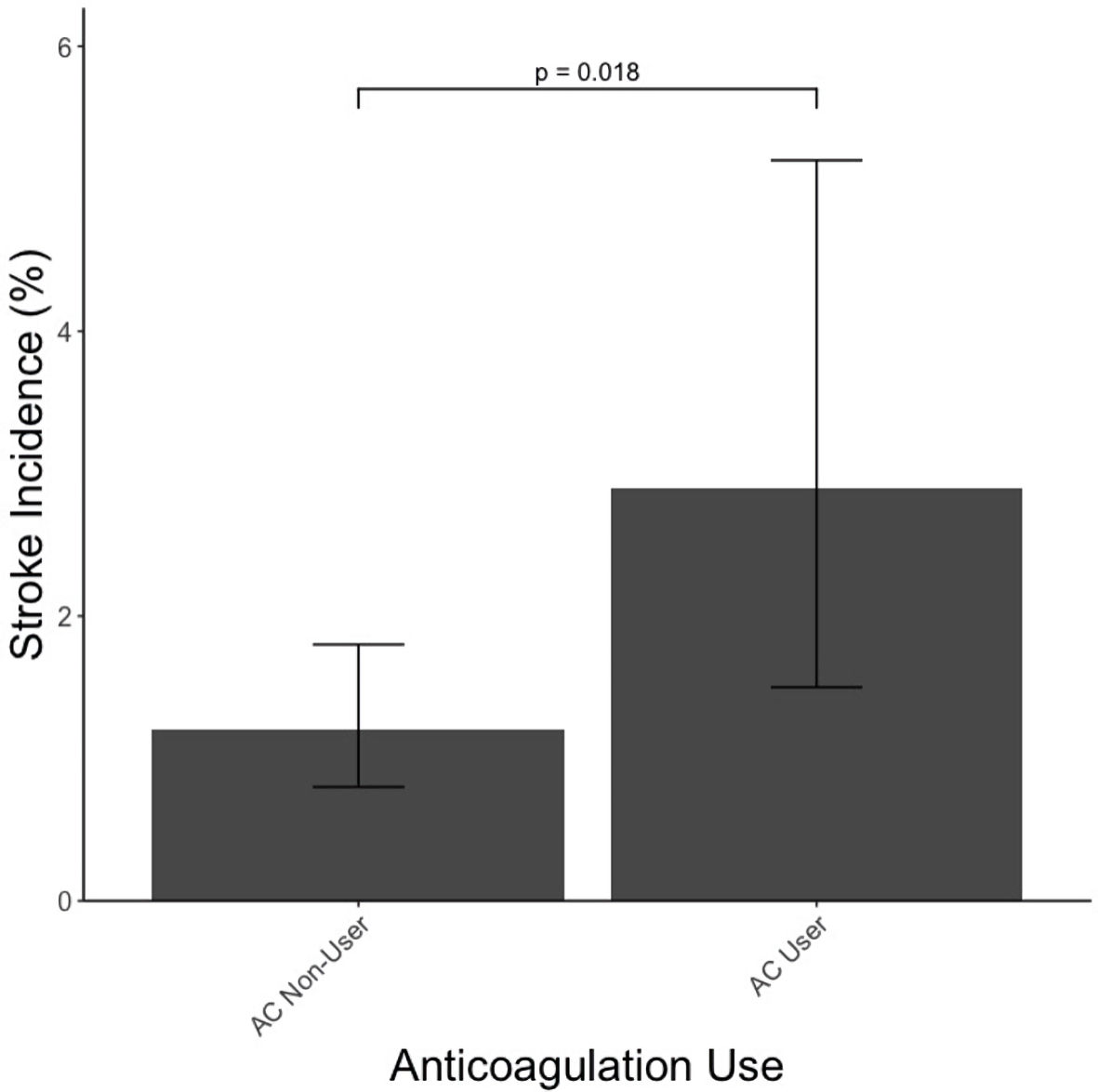 Click for large image | Figure 7. Stroke incidence by use of anticoagulation. Bars illustrate mean ± SD. AC: anticoagulation; SD: standard deviation. |
Examination of all-cause mortality showed that AC non-users had higher incidence of all-cause mortality compared to AC users (13.9% vs. 7.7%, P = 0.001) (Fig. 8). Logistic regression analysis confirmed that AC use was associated with decreased risk of all-cause mortality (OR = 0.34, 95% CI: 0.23 - 0.52, P < 0.001).
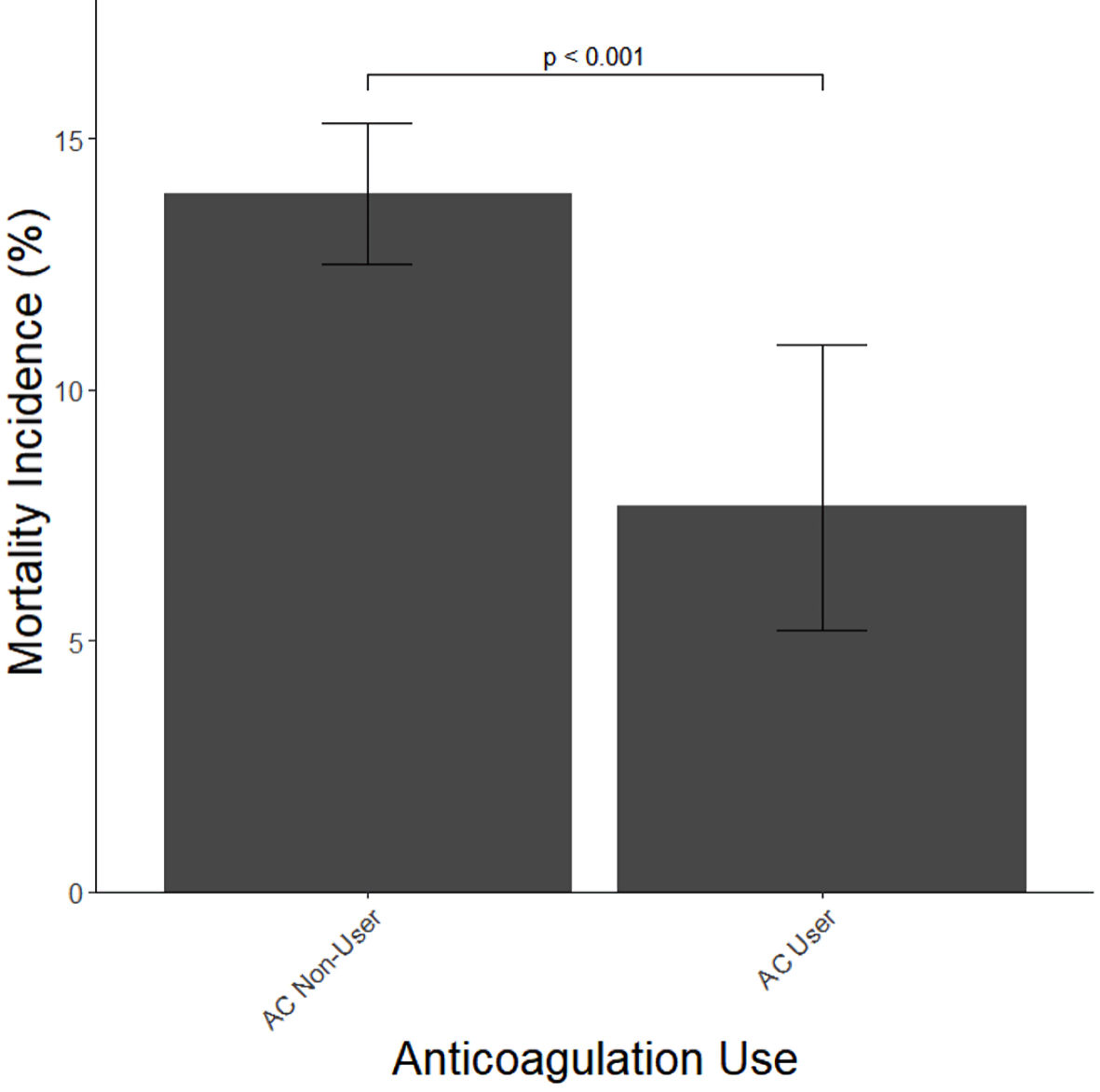 Click for large image | Figure 8. All-cause mortality incidence by use of anticoagulation. Bars illustrate mean ± SD. AC: anticoagulation; SD: standard deviation. |
| Discussion | ▴Top |
We demonstrated that ambulatory AC use significantly increased the risk of MACEs, including acute HF, MI, PE/DVT, pericardial effusion, and stroke in our patient cohort. However, AC users had a significantly decreased risk of all-cause mortality when hospitalized for COVID-19 infection. The mechanism of this disparity between MACEs and cardiovascular mortality may reflect the age disparity between the AC group and the non-AC group as the aging population likely has increased propensity toward MACEs. An additional possibility behind these findings is that AC, while preventing catastrophic adverse events such as stroke, may be causing more harm in this patient population as evidenced by the increased incidence of MACEs. However, it is unclear whether this risk of increased MACEs outweighs the benefit of decreased cardiovascular mortality in this population.
Based on the current literature, this appears to be the first large cohort study addressing the effect of ambulatory AC use in unvaccinated COVID-19 patients on all-cause mortality and MACEs. A recent meta-analysis of patients starting either therapeutic or prophylactic dosing of AC after hospital admission concluded that prophylactic AC is at least as effective as therapeutic AC at reducing all-cause mortality and the incidence of intubation [12]. However, this study did not distinguish between ambulatory AC and non-AC users and did not specifically assess MACE. Regarding inpatient AC use in COVID-19 patients, Paranjpe et al [13] showed that treating mechanically ventilated patients with AC doubled the median length of survival. Furthermore, Nadkarni et al [14] and Stone et al [15] showed AC use was associated with decreased all-cause mortality and incidence of intubation in COVID-19 patients. However, Lopes et al [16] showed no difference in clinical outcomes between COVID-19 patients receiving therapeutic or prophylactic AC but did show increased bleeding risk in therapeutic AC patients. Tremblay et al [17] also showed no significant difference in survival or time to mechanical ventilation in AC users with COVID-19. However, these previous studies did not assess specific mortality or MACEs in patients and are limited by the assessment of only inpatient AC use. Our study is unique given that it shows a decrease in all-cause mortality. Also, previous studies did not assess MACEs in this population.
Study strengths include a large and diverse patient population with known COVID-19 infection and ambulatory AC use from four different hospitals, individual chart review and comprehensive validation of data, and a focus on all-cause mortality and MACEs in a disproportionately vulnerable population of unvaccinated ambulatory AC users. However, this study does have limitations. Vaccinated patients were excluded from this study by design. Therefore, we have no data on the response of vaccinated patients to the continuation of AC after hospital admission. Additionally, a component of the data in this study relied on subjective information gathered from the patient to characterize compliance with ambulatory AC therapy which may lead to bias. Furthermore, the data do not analyze the initiation of AC after admission in this patient population and only serves to comment on the decision to continue AC inpatient if the patient is compliant with their outpatient regimen. In addition, the increased rate of MACEs in the AC group may be complicated by the age discrepancy in this retrospective study, as more AC users were significantly older than non-AC users. Future research, perhaps in a prospective fashion, is needed to further stratify the risk of MACE in an age-matched patient population. Finally, this cohort represents a subgroup of patients who suffer from chronic cardiovascular disease and therefore are excessively vulnerable; therefore, the generalizability of these findings remains to be determined.
This study showed ambulatory use of AC is associated with increased incidence of MACEs and decreased incidence of mortality in unvaccinated patients hospitalized with COVID-19 infection. Regarding the increased incidence of MACEs in AC users, it is important to remember the age discrepancy among the population in this study as increased incidence of MACEs would be expected in older individuals such as the AC user group in this data analysis. These results will help physicians stratify the risk of ambulatory AC users with COVID-19 for both MACEs and mortality, help guide the decision to continue AC inpatient in this patient population and prepare for and predict adverse outcomes. Given the findings of this study contradict various previous studies regarding the finding of increased MACE, further investigation is warranted. Future research may focus on prospective data regarding continuation of AC during the transition from outpatient to inpatient, as well as proper selection of patients for which increased MACEs outweighs the benefits of continuing AC after hospital admission.
Acknowledgments
The authors thank Anne Murray, PhD, MWC® for providing editorial support. The authors thank all contributors to the data-gathering process.
Financial Disclosure
This manuscript is not associated with any grants, contracts, or other forms of financial support.
Conflict of Interest
None to declare.
Informed Consent
Necessary informed consent was obtained.
Author Contributions
Nathan DeRon Jr. wrote the manuscript, performed all statistical analysis, and generated all figures. Lawrence Hoang contributed to statistical analysis and figure generation. Kristopher Aten contributed to writing and editing the results of the study. Sri Prathivada provided assistance with data collection and study design. Manavjot Sidhu contributed expertise in the field of cardiovascular disease, editing of the manuscript, and construction of the design and implementation of the data-gathering phase.
Data Availability
The data that support the findings of this study are available from the corresponding author, Dr. Nathan DeRon Jr., upon reasonable request.
| References | ▴Top |
- World Health Organization. n.d. The top 10 causes of death. World Health Organization. Retrieved January 23, 2023. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802-810.
doi pubmed pmc - Nguyen N, Nguyen H, Ukoha C, Hoang L, Patel C, Ikram FG, Acharya P, et al. Relation of interleukin-6 levels in COVID-19 patients with major adverse cardiac events. Proc (Bayl Univ Med Cent). 2022;35(1):6-9.
doi pubmed pmc - Wang L, Hoang L, Aten K, Abualfoul M, Canela V, Prathivada S, Vu M, et al. Mortality and major adverse cardiovascular events in hospitalized patients with atrial fibrillation with COVID-19. Am J Cardiol. 2023;189:41-48.
doi pubmed pmc - Dewland TA, Whitman IR, Win S, Sanchez JM, Olgin JE, Pletcher MJ, Santhosh L, et al. Prospective arrhythmia surveillance after a COVID-19 diagnosis. Open Heart. 2022;9(1):e001758.
doi pubmed pmc - Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062.
doi pubmed pmc - Oikonomou E, Lampsas S, Souvaliotis N, Sarantos S, Siasos G, Poulakou G, Lytra T, et al. Vaccination against SARS-CoV-2 protects from COVID-19-induced endothelial dysfunction. Curr Pharm Des. 2022;28(39):3225-3230.
doi pubmed - Singanayagam A, Hakki S, Dunning J, Madon KJ, Crone MA, Koycheva A, Derqui-Fernandez N, et al. Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study. Lancet Infect Dis. 2022;22(2):183-195.
doi pubmed pmc - ATTACC Investigators; ACTIV-4a Investigators; REMAP-CAP Investigators; Lawler PR, Goligher EC, Berger JS, Neal MD, et al. Therapeutic anticoagulation with heparin in noncritically ill patients with COVID-19. N Engl J Med. 2021;385(9):790-802.
doi pubmed pmc - Spyropoulos AC, Goldin M, Giannis D, Diab W, Wang J, Khanijo S, Mignatti A, et al. Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with COVID-19: the HEP-COVID randomized clinical trial. JAMA Intern Med. 2021;181(12):1612-1620.
doi pubmed pmc - Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48(3):452-458.
doi pubmed pmc - Muthiah A, Srikumar S, Saravanan PB, Perumal S. Anti-coagulation therapy on COVID-19 patients: A systematic review and meta-analysis. Lung India. 2022;39(6):562-570.
doi pubmed pmc - Paranjpe I, Fuster V, Lala A, Russak AJ, Glicksberg BS, Levin MA, Charney AW, et al. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76(1):122-124.
doi pubmed pmc - Nadkarni GN, Lala A, Bagiella E, Chang HL, Moreno PR, Pujadas E, Arvind V, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76(16):1815-1826.
doi pubmed pmc - Stone GW, Farkouh ME, Lala A, Tinuoye E, Dressler O, Moreno PR, Palacios IF, et al. Randomized trial of anticoagulation strategies for noncritically ill patients hospitalized with COVID-19. J Am Coll Cardiol. 2023;81(18):1747-1762.
doi pubmed pmc - Lopes RD, de Barros ESPGM, Furtado RHM, Macedo AVS, Bronhara B, Damiani LP, Barbosa LM, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet. 2021;397(10291):2253-2263.
doi pubmed pmc - Tremblay D, van Gerwen M, Alsen M, Thibaud S, Kessler A, Venugopal S, Makki I, et al. Impact of anticoagulation prior to COVID-19 infection: a propensity score-matched cohort study. Blood. 2020;136(1):144-147.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


