| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 15, Number 1, February 2024, pages 29-36
Partial Pressure of End-Tidal Oxygen and Blood Lactate During Cardiopulmonary Exercise Testing in Healthy Older Participants and Patients at Risk of Cardiac Disease
Kazuyuki Kominamia, c , Masatoshi Akinob
aDepartment of Rehabilitation, Sanseikai Kitano Hospital, 6-30, 1- chome, Kitano 1-jyo, Kiyota-ku, Sapporo, Hokkaido 004-0861, Japan
bDepartment of Internal Medicine, Sapporo Kiyota Hospital, 1-1, 1-chome, Shin-ei 1-jyo, Kiyota-ku, Sapporo, Hokkaido 004-0831, Japan
cCorresponding Author: Kazuyuki Kominami, Department of Rehabilitation, Sanseikai Kitano Hospital, 6-30, 1- chome, Kitano 1-jyo, Kiyota-ku, Sapporo, Hokkaido 004-0861, Japan
Manuscript submitted November 26, 2023, accepted January 3, 2024, published online February 28, 2024
Short title: Blood Lactate and End-Tidal Oxygen
doi: https://doi.org/10.14740/cr1597
| Abstract | ▴Top |
Background: The partial pressure of end-tidal oxygen (PETO2) and end-tidal oxygen concentration (ETO2) are among the indices that can be measured by exhaled gas analysis. Several observational studies have shown that skeletal muscle function is impaired in patients with cardiac disease; thus, the assessment of skeletal muscle function is important. Additionally, although it has recently been suggested that the difference in PETO2 from rest to the ventilatory anaerobic threshold (VAT) reflects oxygen availability in peripheral factors, primarily skeletal muscle, the evidence for this is not well established. Therefore, we hypothesized and investigated whether increased blood lactate (BLa) levels, resulting from decreased skeletal muscle and mitochondrial oxygen availability, and PETO2 dynamics during cardiopulmonary exercise testing (CPET) would be related.
Methods: All participants performed the symptomatic limited CPET, and their BLa levels were measured. The difference in PETO2 and ETO2 from rest to VAT determined by the V-slope method (ΔPETO2 and ΔETO2) was calculated and compared with the increase in BLa due to exercise testing.
Results: We recruited 22 healthy older participants (nine males; 69.4 ± 6.8 years) and 11 patients with cardiovascular risk (eight males; 73.0 ± 8.8 years). ΔPETO2 and ΔETO2 did not differ between the two groups (P = 0.355 and P = 0.369, respectively), showing no correlation between increase in BLa from rest to VAT, but were significantly correlated with an increase in BLa from rest to the end of exercise (ΔPETO2, P = 0.030; ΔETO2, P = 0.029). The correlation was particularly pronounced among those at cardiovascular risk (ΔPETO2, P = 0.012; ΔETO2, P = 0.011).
Conclusions: ΔPETO2 and ΔETO2 from rest to VAT during CPET may be useful as indices reflecting skeletal muscle oxygen utilization capacity.
Keywords: End-tidal oxygen; Blood lactate; Cardiopulmonary exercise testing; Cardiovascular disease; Incremental exercise; Older population
| Introduction | ▴Top |
For accurate exercise prescription and cardiorespiratory health assessment, cardiopulmonary exercise testing (CPET) using a respiratory gas analyzer system has become the gold standard protocol in research and clinical practice to quantify main aerobic parameters (e.g., maximal peak oxygen uptake (VO2), ventilatory anaerobic threshold (VAT), and respiratory compensation point (RCP)) [1]. In addition, the partial pressure of end-tidal oxygen (PETO2) and end-tidal oxygen concentration (ETO2) are among the indicators that can be measured by exhaled gas analysis.
When the oxygen demand of exercising muscles increases, blood flow to these muscles increases and oxygen extraction from the blood by the muscles increases, which leads to a decrease in the partial pressure of oxygen in the blood that returns to the lungs [2]. This, in turn, leads to a decrease in PETO2 during exercise. Thus, a greater decrease in PETO2 from rest to exercise would indicate greater oxygen extraction and utilization by the muscles.
In general, skeletal muscle oxygen utilization refers to the amount of oxygen supplied to and utilized by muscles during physical activity and is usually measured by methods such as near infrared spectroscopy (NIRS) and muscle oxygen saturation (SmO2) monitoring [3, 4]. In addition, differences in PETO2 from rest to VAT (ΔPETO2) reflect oxygen extraction capacity in peripheral factors, such as the skeletal muscles [5-7]. Blood lactate (BLa) exists as an intermediate metabolite between glycolysis and mitochondrial oxygen utilization [8], and decreased skeletal muscle and mitochondrial oxygen availability may indicate increased BLa [9, 10]. Although ΔPETO2 and BLa are not directly related, both are indicators of different aspects of muscle metabolism during exercise. ΔPETO2 reflects the extraction and utilization of oxygen by muscle [5-7], while BLa reflects the accumulation of lactic acid in the blood, a byproduct of anaerobic metabolism [11]. Additionally, various risk factors for cardiovascular disease have been reported to cause a decrease in type 1 fibers, leading to impaired skeletal muscle function [12, 13]. It is conceivable that a decrease in skeletal muscle oxygen availability would result in an early addition of anaerobic metabolism in response to increased exercise intensity, leading to a greater accumulation of lactate, while ΔPETO2 would decrease.
We hypothesized that low ΔPETO2, which indicates peripheral skeletal muscle oxygen utilization during CPET, would result in higher BLa at the end of exercise, and that this would be more pronounced in individuals at risk for cardiac disease. We, therefore, aimed to clarify the relationship between ΔPETO2 and BLa during CPET in healthy older participants and patients with risk for cardiac disease close to the age of eligibility for cardiac rehabilitation [14-16]. The results of this study will provide evidence that ΔPETO2 is an indicator of skeletal muscle oxygen utilization capacity and will provide a noninvasive indicator of changes in skeletal muscle function with exercise training.
| Materials and Methods | ▴Top |
Participants
We enrolled participants aged between 60 and 80 years during the period May 1, 2016, to April 30, 2019. The recruitment process resulted in 11 patients who were currently taking medication for either cardiovascular diseases (n = 5) or cardiovascular risk factors (n = 6), forming group P, which had an average age of 72.6 ± 8.5 years and consisted of nine males. Among these patients, the cardiovascular disease etiologies included coronary artery disease post-coronary artery bypass graft surgery (n = 2), myocardial infarction (n = 1), and valvular heart disease (n = 2), while the cardiovascular risk factors included hypertension (n = 11), impaired glucose tolerance or diabetes mellitus (n = 2), and hyperlipidemia (n = 8). For comparison purposes, 22 healthy participants were recruited, forming group H, and matched the age range of group P, with an average age of 69.3 ± 6.7 years and nine male participants (Table 1).
 Click to view | Table 1. Data of Participants’ Clinical Characteristics |
We excluded patients with recent changes in medication within 6 months, recent infection within 2 weeks, body temperature exceeding 37.5 °C, chronic atrial fibrillation or flutter, permanent pacemakers, and orthopedic conditions that could hinder exercise testing. Participants who were on warfarin or other anticoagulants and metformin for diabetes were also excluded. The cases and measurement records for this study were collected from participants in a previous study [17].
Exercise testing
CPET was performed using a stationary bicycle (StrengthErgo 8; Mitsubishi Electric Engineering, Tokyo, Japan) and a breath-by-breath gas analyzer (AE-300S; Minato Ikagaku Co., Tokyo, Japan). Symptomatic maximal exercise was performed using a ramp protocol of 10 W/min (incremental exercise). After 2 min rest (sitting on the stationary bicycle), warm-up exercises were performed for 2 min at 10 W. We used 10-s average data for all analyses. The output was obtained using a gas analyzer system.
VAT determination
We determined VAT during incremental exercise testing, visually determined using the modified V-slope method described by Sue et al [18], a modification of the method described by Beaver et al [19], as previously published [20, 21].
BLa measurement
Blood was sampled using a finger prick test. A topical vasodilator (Finalgon cream, nonivamide butoxyethyl; Boehringer Ingelheim, Gaithersburg, MD) was applied to three fingers of the left hand (second, third, and fourth). The cream was removed after 10 min, and the entire left hand, including the distal part of the forearm, was placed in a water bath (at 43 - 45 °C) for 10 min [22, 23]. The BLa levels were determined using Lactate Pro LT-1730 (Arkray, Kyoto, Japan), calibrated using a strip before each exercise session. Blood samples were collected every minute during the ramp exercise.
PETO2 and ΔETO2
Rest PETO2 and ETO2 were recorded as the mean value of the last half 1 min at the 2 min rest period in CPET. ΔPETO2 was the difference between VAT PETO2 and rest PETO2. ΔETO2 was calculated in the same way.
Rate of perceived exertion and miscellaneous measures
The rate of perceived exertion was measured using the Borg scale. Left ventricular ejection fraction was determined using the Teichholz method. Brain natriuretic peptide levels were determined using a chemiluminescent enzyme immunoassay.
Statistical analysis
Data are presented as mean ± standard deviation (SD) and 95% confidence intervals. Unpaired data were analyzed using Student’s t-test. Paired data were analyzed using paired t-tests. Comparisons of BLa, PETO2, and ETO2 between the two groups were performed using a repeated two-way analysis of variance (ANOVA). Plots of the ΔPETO2, ΔETO2, and BLa were linearly regressed, and regression equations and coefficients were calculated. The 95% confidence intervals were also calculated to determine the relationship between ΔPETO2, ΔETO2, and BLa. Statistical analyses were performed with Statistics for Excel 2012 (Social Survey Research Information Co., Tokyo, Japan).
Ethical considerations
The study was conducted in accordance with the principles outlined in the Declaration of Helsinki and approved by the Institutional Review Board of Sapporo Ryokuai Hospital (approval number: 19-1). Informed consent was obtained from all participants permission in writing provided for publication of this report. The authors confirm that there is no identifying information of the participants in the manuscript and that the information has been fully anonymized. Furthermore, the authors affirm that all mandatory health and safety procedures were observed while conducting the experimental work reported in this paper.
| Results | ▴Top |
The clinical characteristics of the participants are summarized in Table 1. Group P had a higher proportion of males, with significantly higher mean height and weight, than group H.
Change of PETO2, ETO2, and BLa
The changes over time in PETO2, ETO2, and BLa during the CPET are shown in Table 2. No significant differences were found between the two groups. There were also no significant differences in ΔPETO2 and ΔETO2 between the two groups (ΔPETO2 (at rest) H: -6.21 ± 3.13 (-4.91 to -7.52) mm Hg, P: -5.21 ± 3.13 (-3.36 to -7.06) mm Hg, P = 0.355; ΔETO2 (at rest) H: -0.89±0.45% (-0.70 to -1.07), P: -0.75±0.45% (-0.48 to -1.01), P = 0.369).
 Click to view | Table 2. Data of End-Tidal Oxygen Concentration and Blood Lactate in CPET |
Furthermore, there were no significant differences in ΔBLa from rest to VAT (VAT - rest; H: 0.35 ± 0.31 (0.22 - 0.48) mmol/L, P: 0.44 ± 0.31 (0.25 - 0.62) mmol, P = 0.483), rest to peak (peak - rest; H: 4.14 ± 2.28 (3.19 - 5.09) mmol/L, P: 4.85 ± 2.28 (3.43 - 6.26) mmol, P = 0.321), and VAT to peak (peak - VAT; H: 3.79 ± 2.25 (2.85 - 4.73) mmol/L, P: 4.39 ± 2.25 (3.00 - 5.79) mmol, P = 0.405).
ΔPETO2, ΔETO2, and BLa
There was a significant correlation between ΔPETO2 and ΔBLa (peak - rest) (r = 0.428 (0.100 ≤ ρ ≤ 0.673), P = 0.014), ΔPETO2, and ΔBLa (peak - AT) (r = 0.436 (0.109 ≤ ρ ≤ 0.678), P = 0.012). ΔETO2 showed a significant correlation as well (ΔBLa (peak - rest); r = 0.431 (0.102 ≤ ρ ≤ 0.674), P = 0.014, ΔBLa (peak - AT); r = 0.440 (0.114 ≤ ρ ≤ 0.681), P = 0.013).
Also, separating the healthy older and those at risk for cardiac disease, no correlation was observed in the healthy older; however, a significant correlation with ΔPETO2, ΔETO2, and ΔBLa was observed in those at risk for cardiac disease (Fig. 1) (ΔPETO2: P; r = 0.736 (0.243 ≤ ρ ≤ 0.927), P = 0.012, H; r = 0.205 (-0.237 ≤ ρ ≤ 0.577), P = 0.377, P vs. H; P = 0.082, ΔETO2: P; r = 0.739 (0.250 ≤ ρ ≤ 0.928), P = 0.011, H; r = 0.205 (-0.237 ≤ ρ ≤ 0.577), P = 0.376, P vs. H; P = 0.079).
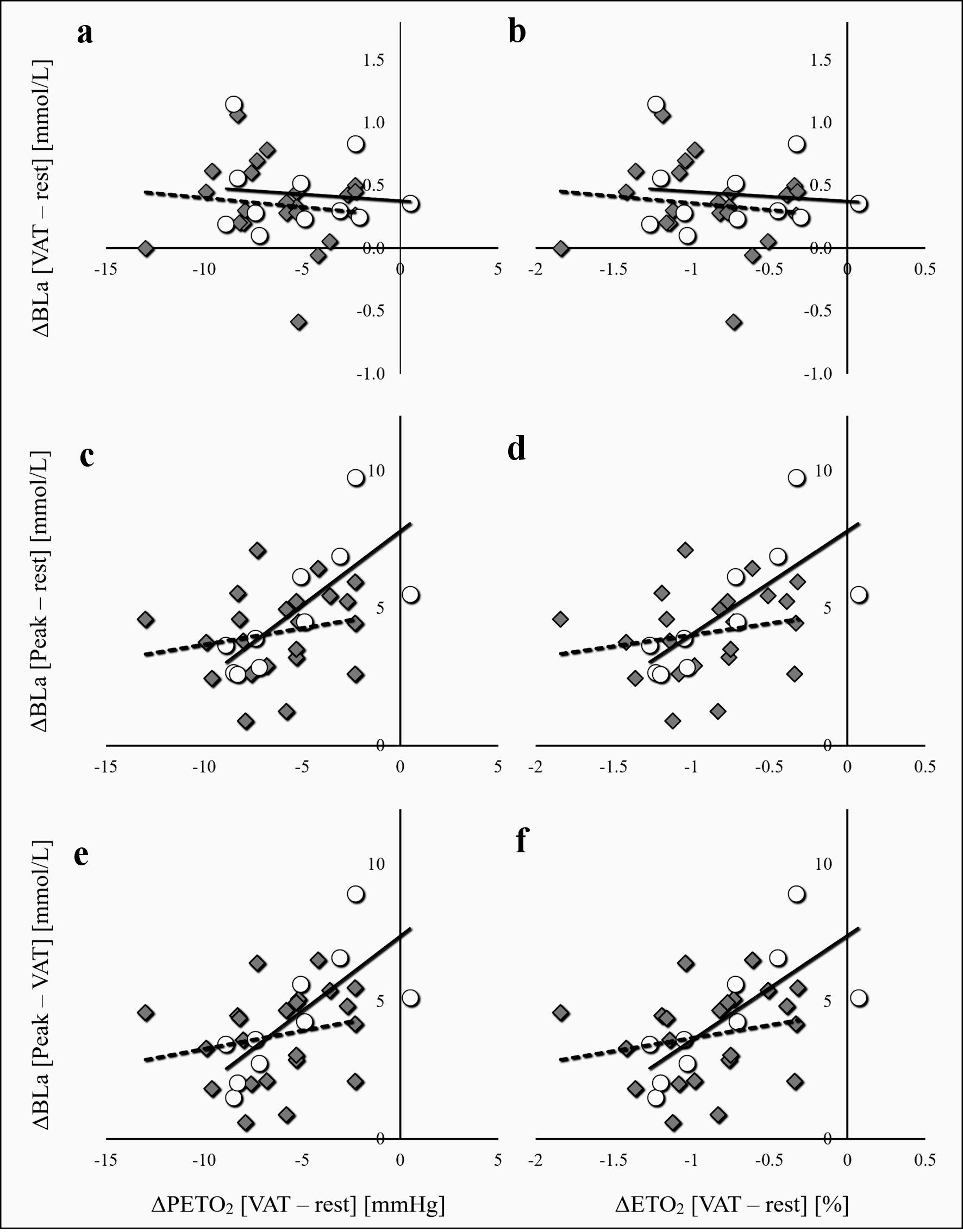 Click for large image | Figure 1. Relationship between ΔPETO2, ΔETO2, and BLa. The diamond (◊) and dotted line indicates healthy subjects, and the circle (○) and straight line indicate patients with cardiac risks. ΔPETO2 and ΔETO2 were not correlated with BLa from rest to VAT (BLa (VAT - rest)) in both groups (a, b). In subjects at risk for cardiac disease, ΔPETO2 from rest to VAT (ΔPETO2) showed a significant correlation with the increase in BLa from rest to peak (ΔBLa (peak - rest)) (c). ΔPETO2 and the increase in BLa from VAT to peak (ΔBLa (peak - VAT)) also showed a significant correlation (e). ΔETO2 also showed similar associations (d, f). ETO2: end-tidal oxygen concentration; PETO2: partial pressure of end-tidal oxygen; BLa: blood lactate; VAT: ventilatory anaerobic threshold. |
| Discussion | ▴Top |
ΔPETO2 and ΔETO2 did not differ between the two groups and were not correlated with an increase in BLa from rest to VAT, but they were significantly correlated with an increase in BLa from rest to the end of exercise. The correlation was particularly pronounced among those at cardiovascular risk. Therefore, ΔPETO2 and ΔETO2 from rest to VAT may be useful as indices reflecting skeletal muscle oxygen utilization capacity. To the best of our knowledge, this is one of the few studies to confirm the relationship between the change of BLa levels, ETO2, and PETO2 during incremental exercise testing in healthy older adults and patients with cardiovascular disease/risk factors. To date, these results have not been reported in healthy older adults or patients with cardiovascular risk.
PETO2 decreases from rest to VAT. This is due to an increase in oxygen uptake with exercise, an increase in minute ventilation, and an increase in oxygen utilization in the alveoli due to improved gas exchange efficiency, resulting in a decrease in oxygen in exhaled breath. Once VAT is reached, PETO2 begins to increase as the rate of anaerobic metabolism increases and the minute ventilation rate increases beyond oxygen uptake (i.e., ventilation increases beyond oxygen demand, and oxygen not used for gas exchange is returned to the exhaled breath). In the present study, PETO2 and ETO2 were significantly higher at VAT in patients with cardiovascular risk compared to healthy subjects. In addition, PETO2 and ETO2 from rest to VAT (ΔPETO2 and ΔETO2) tended to be lower, although the differences were not significant.
Various risk factors for cardiovascular disease have been reported to cause a decrease in type 1 fibers, leading to reduced skeletal muscle and mitochondrial function [12, 13]. Furthermore, progression to heart failure further reduces skeletal muscle and mitochondrial function [24-26]. Therefore, ΔPETO2 and ΔETO2 may gradually decrease with the progression of heart disease and the onset and severity of heart failure. Since the present study included well-controlled patients with risk of cardiac disease and healthy subjects, ΔPETO2 was comparable to that of the mild disease group in a previous study [6]. Therefore, it is possible that skeletal muscle function or skeletal muscle and mitochondrial oxygen utilization capacity was not as impaired as in the medium to severe disease group of the previous study. Alternatively, the limited number of cases in the present study may have resulted in the absence of statistically significant differences. The knowledge of the dynamics of PETO2 during the incremental exercise used in the present study is scarce, and it is desirable to continue the investigation and deepen the knowledge by including more severe cases of impaired cardiac function.
As exercise intensity increases, the exercising muscles produce the energy required for exercise. At exercise intensities below VAT, the electron transport chain is the main source of energy production, and as the exercise intensity increases and becomes higher than the VAT, the rate of energy production by the glycolytic pathway increases. This increased lactate produced by the exercising muscles exceeds the buffering capacity of the organism, resulting in increased BLa levels. Lactate produced by exercise has recently been shown to have a variety of positive effects on the body [27]. However, this BLa level is greatly influenced by the amount of lactate produced by the activity of the glycolytic system, skeletal muscle oxygen utilization capacity, and lactate clearance by mitochondrial function [8, 28]. Decreased skeletal muscle and mitochondrial oxygen utilization capacity facilitates the production of lactate to provide the energy required for exercise. In addition, patients with cardiac disease are more likely to have increased BLa levels during exercise [29]. Moreover, progression of renal dysfunction or anemia enhances glycolytic system activity, resulting in an increase in lactate production [30, 31]. However, since renal dysfunction or anemia was virtually absent in the patients with cardiac risk in the present study, increased lactate production due to glycolytic pathway activity was unlikely to occur, suggesting that decreased lactate clearance associated with impaired skeletal muscle mitochondrial function was responsible for the increased BLa levels (lactate shuttles are used as an energy substrate by skeletal muscle type I fibers in other parts of the body). This would suggest that BLa was slightly higher in the patients with cardiac risk compared to the healthy group at VAT, and that BLa was significantly higher at peak exercise. Thus, ΔPETO2 or ΔETO2 in patients with no or mildly impaired renal function during incremental exercise was associated with increased BLa levels as well as skeletal muscle oxygen utilization capacity.
However, PETO2 has been shown to be affected by changes in measured altitude or ventilation [32]. Since no differences were observed in the relationship of ΔPETO2 and ΔETO2 to changes in BLa, neither indicator requires consideration in a standard environment, but care should be taken in the handling of values and interpretation depending on the environment. In addition, since ΔPETO2 and ΔETO2 estimate skeletal muscle oxygen utilization capacity indirectly via the exhaled gas, they are not as accurate as direct measurements of muscle oxygenation such as NIRS and SmO2 monitoring, and their reliability may be increased when used in conjunction with these instruments [33, 34]. Furthermore, we believe that confirmation of underlying disease will be important in diseases such as chronic obstructive pulmonary disease (COPD), where the dead space is increased, because the respiratory state may be easily affected.
There are some limitations to this study. First, the number of cases is small. Therefore, the characteristics of the disease have not been adequately investigated. Second, the oxygen utilization capacity of skeletal muscle has not been directly examined. Therefore, skeletal muscle oxygen utilization has been assessed indirectly and other factors related to exhaled gas analysis and BLa levels have not been evaluated.
Conclusions
The amount of change in PETO2 from rest to VAT (ΔPETO2) was associated with the amount of increase in BLa during the subsequent incremental exercise. ΔPETO2 and ΔETO2 from rest to VAT may be useful as indices reflecting skeletal muscle oxygen utilization capacity.
Acknowledgments
None to declare.
Financial Disclosure
This study did not receive any funding support.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Informed consent was obtained from all participants’ permission in writing provided for publication of this report.
Author Contributions
KK and MA developed the study concept and were involved in its design and implementation. KK delivered program content to the participants, acquired data, analyzed the data, and prepared the manuscript. MA drafted the manuscript and approved the final draft. All the authors have read and approved the final version of the manuscript.
Data Availability
The dataset used in this study is available from the corresponding author upon request.
Abbreviations
VAT: ventilatory anaerobic threshold; CPET: cardiopulmonary exercise testing; VO2: oxygen uptake; ETO2: end-tidal oxygen concentration; PETO2: partial pressure of end-tidal oxygen
| References | ▴Top |
- Jabbar HR, Abbas A, Ahmed M, Klodell CT, Jr., Chang M, Dai Y, Draganov PV. The Incidence, Predictors and Outcomes of Gastrointestinal Bleeding in Patients with Left Ventricular Assist Device (LVAD). Dig Dis Sci. 2015;60(12):3697-3706.
doi pubmed - Miller LW, Pagani FD, Russell SD, John R, Boyle AJ, Aaronson KD, Conte JV, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357(9):885-896.
doi pubmed - Draper KV, Huang RJ, Gerson LB. GI bleeding in patients with continuous-flow left ventricular assist devices: a systematic review and meta-analysis. Gastrointest Endosc. 2014;80(3):435-446.e431.
doi pubmed - Demirozu ZT, Radovancevic R, Hochman LF, Gregoric ID, Letsou GV, Kar B, Bogaev RC, et al. Arteriovenous malformation and gastrointestinal bleeding in patients with the HeartMate II left ventricular assist device. J Heart Lung Transplant. 2011;30(8):849-853.
doi pubmed - Goldstein DJ, Aaronson KD, Tatooles AJ, Silvestry SC, Jeevanandam V, Gordon R, Hathaway DR, et al. Gastrointestinal bleeding in recipients of the HeartWare Ventricular Assist System. JACC Heart Fail. 2015;3(4):303-313.
doi pubmed - Aggarwal A, Pant R, Kumar S, Sharma P, Gallagher C, Tatooles AJ, Pappas PS, et al. Incidence and management of gastrointestinal bleeding with continuous flow assist devices. Ann Thorac Surg. 2012;93(5):1534-1540.
doi pubmed - Letsou GV, Shah N, Gregoric ID, Myers TJ, Delgado R, Frazier OH. Gastrointestinal bleeding from arteriovenous malformations in patients supported by the Jarvik 2000 axial-flow left ventricular assist device. J Heart Lung Transplant. 2005;24(1):105-109.
doi pubmed - Pate GE, Chandavimol M, Naiman SC, Webb JG. Heyde's syndrome: a review. J Heart Valve Dis. 2004;13(5):701-712.
pubmed - Baumann Kreuziger LM. Management of anticoagulation and antiplatelet therapy in patients with left ventricular assist devices. J Thromb Thrombolysis. 2015;39(3):337-344.
doi pubmed - Shrode CW, Draper KV, Huang RJ, Kennedy JL, Godsey AC, Morrison CC, Shami VM, et al. Significantly higher rates of gastrointestinal bleeding and thromboembolic events with left ventricular assist devices. Clin Gastroenterol Hepatol. 2014;12(9):1461-1467.
doi pubmed - Morgan JA, Paone G, Nemeh HW, Henry SE, Patel R, Vavra J, Williams CT, et al. Gastrointestinal bleeding with the HeartMate II left ventricular assist device. J Heart Lung Transplant. 2012;31(7):715-718.
doi pubmed - Taylor C, Bittner K, Bartell N, Aranez J, Alexis JD, Carlson B, Chen L, et al. Outcomes of gastrointestinal bleeding in patients with left ventricular assist devices: a tertiary care experience. Endosc Int Open. 2020;8(3):E301-E309.
doi pubmed pmc - Stern B, Maheshwari P, Gorrepati VS, Bethards D, Chintanaboina J, Boehmer J, Clarke K. Initial endoscopic intervention is not associated with reduced risk of recurrent gastrointestinal bleeding in left ventricular assist device patients. Ann Gastroenterol. 2021;34(5):660-668.
doi pubmed pmc - Truss WD, Weber F, Pamboukian SV, Tripathi A, Peter S. Early implementation of video capsule enteroscopy in patients with left ventricular assist devices and obscure gastrointestinal bleeding. ASAIO J. 2016;62(1):40-45.
doi pubmed - Meyer MM, Young SD, Sun B, Azzouz M, Firstenberg MS. Endoscopic evaluation and management of gastrointestinal bleeding in patients with ventricular assist devices. Gastroenterol Res Pract. 2012;2012:630483.
doi pubmed pmc - Sarosiek K, Bogar L, Conn MI, O'Hare B, Hirose H, Cavarocchi NC. An old problem with a new therapy: gastrointestinal bleeding in ventricular assist device patients and deep overtube-assisted enteroscopy. ASAIO J. 2013;59(4):384-389.
doi pubmed - Tabibian JH, Rhoades DP, Forde KA, McLean RC, Chandrasekhara V. Timing of gastrointestinal bleeding after implantation of left ventricular assist devices associates with anatomic location, presentation, and management. Clin Gastroenterol Hepatol. 2019;17(3):448-454.
doi pubmed - Dakik HK, McGhan AA, Chiu ST, Patel CB, Milano CA, Rogers JG, Chow SC, et al. The Diagnostic Yield of Repeated Endoscopic Evaluation in Patients with Gastrointestinal Bleeding and Left Ventricular Assist Devices. Dig Dis Sci. 2016;61(6):1603-1610.
doi pubmed - Elmunzer BJ, Padhya KT, Lewis JJ, Rangnekar AS, Saini SD, Eswaran SL, Scheiman JM, et al. Endoscopic findings and clinical outcomes in ventricular assist device recipients with gastrointestinal bleeding. Dig Dis Sci. 2011;56(11):3241-3246.
doi pubmed pmc - Palchaudhuri S, Dhawan I, Parsikia A, Birati EY, Wald J, Siddique SM, Fisher LR. Does endoscopic intervention prevent subsequent gastrointestinal bleeding in patients with left ventricular assist devices? A retrospective study. World J Gastroenterol. 2021;27(25):3877-3887.
doi pubmed pmc - Balcioglu O, Engin C, Yagdi T, Nalbantgil S, Baysal B, Erkul S, Engin Y, et al. Effect of aortic valve movements on gastrointestinal bleeding that occured in continuous flow left ventricular assist device patients. Transplant Proc. 2013;45(3):1020-1021.
doi pubmed - Scardulla F, Pasta S, D'Acquisto L, Sciacca S, Agnese V, Vergara C, Quarteroni A, et al. Shear stress alterations in the celiac trunk of patients with a continuous-flow left ventricular assist device as shown by in-silico and in-vitro flow analyses. J Heart Lung Transplant. 2017;36(8):906-913.
doi pubmed - Chong AY, Blann AD, Patel J, Freestone B, Hughes E, Lip GY. Endothelial dysfunction and damage in congestive heart failure: relation of flow-mediated dilation to circulating endothelial cells, plasma indexes of endothelial damage, and brain natriuretic peptide. Circulation. 2004;110(13):1794-1798.
doi pubmed - Hirose H, Sarosiek K, Cavarocchi NC. Ad hoc cost analysis of the new gastrointestinal bleeding algorithm in patients with ventricular assist device. ASAIO J. 2014;60(3):351-352.
doi pubmed - Axelrad JE, Pinsino A, Trinh PN, Thanataveerat A, Brooks C, Demmer RT, Effner L, et al. Limited usefulness of endoscopic evaluation in patients with continuous-flow left ventricular assist devices and gastrointestinal bleeding. J Heart Lung Transplant. 2018;37(6):723-732.
doi pubmed - Eckman PM, John R. Bleeding and thrombosis in patients with continuous-flow ventricular assist devices. Circulation. 2012;125(24):3038-3047.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


