| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://www.cardiologyres.org |
Original Article
Volume 14, Number 4, August 2023, pages 250-260
The Impact of Glucagon-Like Peptide-1 Receptor Agonist on the Cardiovascular Outcomes in Patients With Type 2 Diabetes Mellitus: A Meta-Analysis and Systematic Review
Ali Rahmana, e, Sura Alqaisia, Sunil E. Saithb, Rana Alzakharic, Ralph Levyd
aDepartment of Internal Medicine, Memorial Healthcare System, Pembroke Pines, FL 33028, USA
bCardiovascular Fellowship Program, Cardiovascular Disease at SUNY Downstate Health Sciences University, Brooklyn, NY, USA
cCardiovascular Fellowship Program, University of Texas Medical Branch Cardiovascular Disease Program, Galveston, TX, USA
dDepartment of Memorial Health Cardiology, Cardiovascular Disease at Memorial Healthcare System, Pembroke Pines, FL 33028, USA
eCorresponding Author: Ali Rahman, Department of Internal Medicine, Memorial Healthcare System, Pembroke Pines, FL 33028, USA
Manuscript submitted June 5, 2023, accepted July 11, 2023, published online July 12, 2023
Short title: Impact of GLP-1 RA in T2DM Patients
doi: https://doi.org/10.14740/cr1523
| Abstract | ▴Top |
Background: Since 2005, the cardioprotective effects of glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have garnered attention. The cardioprotective effect could be an added benefit to the use of GLP-1 RA. This systematic review and meta-analysis aimed at summarizing observational studies that recruited type 2 diabetes individuals with fewer cardiovascular (CV) events before enrolling in the research.
Methods: Systematically, the databases were searched for observational studies reporting compound CV events and deaths in type 2 diabetics without having the risk of cardiovascular diseases (CVDs) compared to other glucose-lowering agents. A meta-analysis was carried out using random effects model to estimate the overall hazard ratio (HR) with a 95% confidence interval (CI). Five studies were found eligible for the systematic review including a total of 64,452 patients receiving either liraglutide (three studies) or exenatide (two studies).
Results: The pooled HR for major adverse cardiac event (MACE) and extended MACE was 0.72 (95% CI: 0.65 - 0.93, I2 = 68%) and 0.93 (95% CI: 0.89 - 0.98, I2 = 29%), respectively. The pooled HR for hospitalization due to heart failure (HHF) and occurrence of HF was 0.84 (95% CI: 0.77 - 0.91, I2 = 79%) and 0.83 (95% CI: 0.75 - 0.94, I2 = 95%), respectively. For stroke, GLP-1 RA was associated with a significant risk reduction of 0.86 (95% CI: 0.75 - 0.98, I2 = 81%). There was no significant myocardial infarction (MI) risk reduction with GLP-1 RA. As for all-cause mortality, the pooled HR for the occurrence of all-cause mortality was 0.82 (95% CI: 0.76 - 0.88, I2 = 0%). The pooled HR for the occurrence of CV death was 0.75 (95% CI: 0.65 - 0.85, I2 = 38%). GLP-1 RA therapy was associated with a significantly low risk of MACE, extended MACE, all-cause mortality, and CV mortality. Except for MACE, the heterogenicity among the studies was low.
Conclusion: We conclude that GLP-1 RA is associated with a low risk of CV events composites and mortality. The findings support the cardioprotective effect of GLP-1 RA.
Keywords: Diabetes mellitus; GLP-1 receptor agonist; Exenatide; Liraglutide; Cardiovascular events; MACE
| Introduction | ▴Top |
Since the approval of exenatide, the first glucagon-like peptide 1 receptor agonist (GLP-1 RA) in 2005 [1], researchers have been interested in the cardioprotective effect of the new anti-hyperglycemic drugs. The GLP-1 RA activates GLP-1 receptors on the beta cells leading to increased insulin secretion and decreased inappropriate glucose-dependent glucagon secretion [2, 3]. Additionally, GLP-1 RA has a potential effect on reducing body weight by reducing gastric emptying and increasing satiety [4]. Consequently, GLP-1 RA has become an attractive choice for the treatment of type 2 diabetes mellitus (T2DM) due to the effective reduction of glycosylated hemoglobin (HbA1c) with a lower risk of hypoglycemia and increased weight reduction [5]. Therefore, most of the clinical trials had been directed toward non-inferiority studies [3, 6] to meet the US FDA-issued guidance and the European Medical Agency recommendations that focused on the cardiovascular (CV) [7] safety of the novel drugs [8-10].
The GLP-1 RA group has been shown to not only have acceptable CV safety profiles in primary analyses but also to lower the major adverse cardiac events (MACEs) independent of their effects on hyperglycemia [11]. Therefore, GLP-1 RA is pioneering a new standard of treatment for diabetic patients, giving physicians a good chance to improve patients’ CV health while controlling blood glucose levels. Several mechanisms have been conjectured to interpret the observed CV risk reduction with GLP-1 RA independent of glycemic outcomes. Weight reduction and lowering of blood pressure have been assumed to contribute to the non-glycemic benefits of GLP-1 RA [12]. Moreover, GLP-1 RA has effective anti-inflammatory and anti-oxidative stress properties that could be potential mechanisms for reducing CV risks [13]. Two systematic reviews and meta-analyses involving CV outcome trials showed that GLP-1 RA can reduce a composite of CV events (MACE) in T2DM patients by 12-14% relative to placebo [14, 15]. Furthermore, several post hoc studies attempted to use the data provided by the CV outcome trials to investigate the correlation between the administration of GLP-1 RA and CV outcomes [16-18].
However, these study trials recruited T2DM patients with CV events and patients aged more than 65 years. There have been a few observational studies that have included individuals who had fewer CV events in the time leading up to enrollment. For ethical reasons, the comparators to GLP-1 RA were glucose-lowering drugs such as sulfonylurea, metformin, other novel groups, or insulin [19-21]. As a result, the purposes of this study, a systematic review and meta-analysis, are to compile a summary of the findings of observational studies that recruited T2DM patients who have experienced fewer CV events in the time leading up to their enrollment in the study. The results of the study would characterize the correlation between GLP-1 RA and CV health. Moreover, further needed investigations would be highlighted to settle down the debate about the CV benefits of GLP-1 RA.
| Materials and Methods | ▴Top |
This systematic review and meta-analysis research was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [22, 23]. Additionally, the reporting of the meta-analysis of the observational study followed the Meta-Analysis of Observational Studies in Epidemiology standards [24] during the whole course of this research. The phases of processing were carried out in line with the Cochrane Handbook for Systematic Reviews of Interventions [25] and were demonstrated in the PRISMA flow chart (Fig. 1) [22].
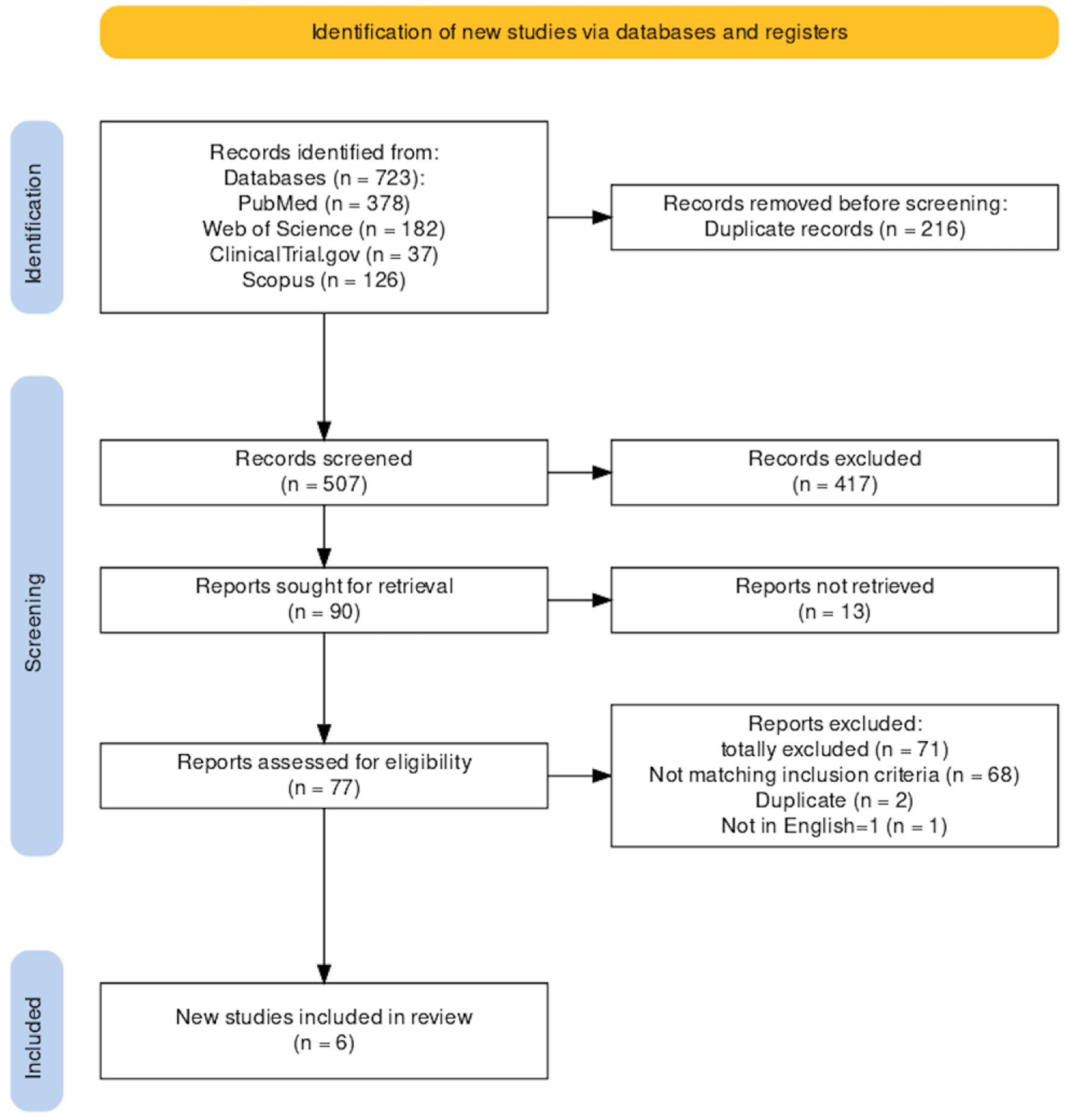 Click for large image | Figure 1. PRISMA flow chart. |
Search strategy
The systematic research was conducted on these databases: PubMed, Web of Science (WoS), and Scopus (through which Embase was searched as well) as well as unpublished articles placed in the registry ClinicalTrails.gov. Cited references were assessed and reviewed for inclusion eligibility. The research was performed in April 2023 on studies from 2005 (the data of the release of the first GLP-1 RA in the USA) up-to-date. Observational studies were identified. The database research was restricted by primary outcomes. The research terms included the appropriate keywords with the use of operators and Mesh terms to restrict the research to inclusion criteria.
Eligibility criteria
Inclusion criteria
The studies were deemed eligible for review if they fulfilled the inclusion criteria. The inclusion-exclusion criteria were first searched and further supported by the patients’ characteristics demonstrated in the corresponding table. The studies were selected based on the following criteria: 1) T2DM who were routine care patients or diagnosed as HbA1c > 6.5%. 2) Age of the participants > 18 years. 3) Diabetic patients with no serious CV events long enough (more than 6 months) before enrolling in the study including HF, unstable angina, or myocardial infarction (MI). 4) Glomerular filtration rate (GFR) ≥ 30 mL/min/1.73 m2 or no end-stage renal disease (ESRD). 5) Follow-up for study outcomes began on the day after cohort entry and continued in an “as-treated” approach until the occurrence of either of these events whichever came first: treatment discontinuation, switch to or augmentation with a drug in the comparator class, and the occurrence of a specific study outcome including death, end of continuous health plan enrollment, or end of the study period.
Exclusion criteria
Articles recruiting patients with the following criteria were excluded from the study: type 1 DM; secondary DM; malignancy; ESRD; renal replacement therapy (RRT); human immunodeficiency virus (HIV); solid organ transplant; nursing home admission at baseline; and the occurrence of one of the following high-risk CV events during the 60 days preceding cohort (study) entrance may operate as confounding and increase the frequency of CV outcomes: hospitalization for acute MI, coronary revascularization, unstable angina, ischemic or hemorrhagic stroke, transient ischemic attack, and heart failure (HF).
Exclusion based on the study article type included: 1) Preclinical studies. 2) Non-observational study articles were excluded from the research including randomized controlled studies (RCTs), narrative reviews, systematic reviews and meta-analyses, post hoc studies, case studies, commentaries, editorials, responses, study protocols, reports, conferences, abstracts, and research design articles. 3) Articles are written in languages other than English.
Outcomes
Primary outcomes
The primary outcomes included time to the first occurrence of: 1) 3P-MACEs: the time to the first event of CV death, non-fatal MI, or non-fatal stroke or 4P-MACEs: hospitalization for unstable angina (HUA). 2) Extended MACEs: MACE plus coronary revascularization, hospitalization for unstable angina pectoris, and HF.
Secondary outcomes
The secondary outcomes included time to the first occurrence of: 1) all CV events; 2) hospitalization for HF; 3) occurrence of HF; 4) stroke: fatal and non-fatal; 5) MI: fatal and non-fatal; 6) all-cause mortality; and 7) CV death.
Data selection and data extraction
Both XYZ and ABC conducted the screening of the search results independently. The eligibility criteria were used to identify the participants for the research based on the title and abstract. The complete text of the study was evaluated to determine the eligible articles for the study. Additionally, the bibliographic references of the included studies were manually searched as well. The data were collected and processed on a spreadsheet. The information that was collected from the data contained demographic details, age groups, gender, dosage groups, and the observed estimate. The consensus was used to settle a dispute on the inclusion of participants in the research.
Assessment of risk of bias
The evaluation of the risk of bias in the results of non-randomized studies of the effects of interventions was carried out using the Risk of Bias in Non-randomized Studies - of Interventions (ROBINS-I) [26]. ROBINS-I considers each study as an attempt to emulate a hypothetical pragmatic randomized trial. It covers seven distinct domains through which the bias might occur including the pre-intervention domain (bias due to confounding and bias in the selection of participants into the study), at intervention domain (bias in classification of intervention), and post-intervention bias (bias due to deviations from intended interventions, bias due to missing data, bias in measurement of outcomes, and bias in selection of the reported results).
Statistical analysis
This meta-analysis was carried out using the Review Manager (RevMan) computer program [27]. A random effects model was calculated because heterogeneity between the study is more likely due to the difference in clinical and methodological factors. Heterogeneity was assessed using a Cochrane Q and quantified using the I2 statistic [25], which shows the variance attributable to heterogeneity as a percentage, with P-values below 0.05 considered to indicate significant heterogeneity.
| Results | ▴Top |
Characteristics of the eligible studies
Applying the search strategy, we recognized 723 records from the identified databases. After removing 216 duplicated and 417 unrelated records, 90 records were left for retrieval. The non-retrieved records were 13 and 77 records were left for further full-text screening for eligibility. Among the records screened for eligibility, 71 were excluded for different reasons. In the end, six studies were selected as eligible for the study based on the inclusion criteria. The search strategy was summarized in the PRISMA flow chart (Fig. 1).
The eligible studies
Six studies were found eligible for the systematic review. One study was excluded because the comparator was another GLP-1 RA medication [28]. Finally, we identified four retrograde observational cohort studies [19, 20, 29, 30] and one comparator [21] study. Except for the comparative study, the other studies were data-based depended. Three studies were conducted in the USA, one study was conducted in Denmark, and one study was conducted in Denmark and Sweden from 2011 to 2022. Three studies investigated liraglutide and two studies investigated exenatide compared to non-insulin anti-diabetic agents (Supplementary Material 1, www.cardiologyres.org).
The eligible studies included a total of 504,029 enrolled participants (patients: 64,452 vs. comparators: 439,577), and males were 45% (n = 224,590) out of the enrolled participants. The diabetic patients were more than 18 with the mean population belonging to the middle-aged group. The duration of the diabetic state varied from as low as 9 months to more than 10 years. The HbA1c was 6.5-8.5% in one study [21]. The other studies did not report the level of HbA1c relying on the identification of diabetic patients based on ICD-9CM [29]. The basal metabolic index (BMI) was reported in only one study [30]. The characteristics of the eligible studies are summarized in Supplementary Material 1, www.cardiologyres.org.
Sensitivity analysis
A funnel plot is a graphical tool to assess the presence of publication bias in a meta-analysis. It plots the effect size of each study against its precision, which is inversely proportional to the standard error. In this case, the funnel plot shows only five studies, which is too few to draw any reliable conclusions about the presence or absence of publication bias according to the Cochrane Handbook for Systematic Reviews of Interventions. The funnel blot shows that the articles are asymmetrically distributed suggesting publication bias (Fig. 2).
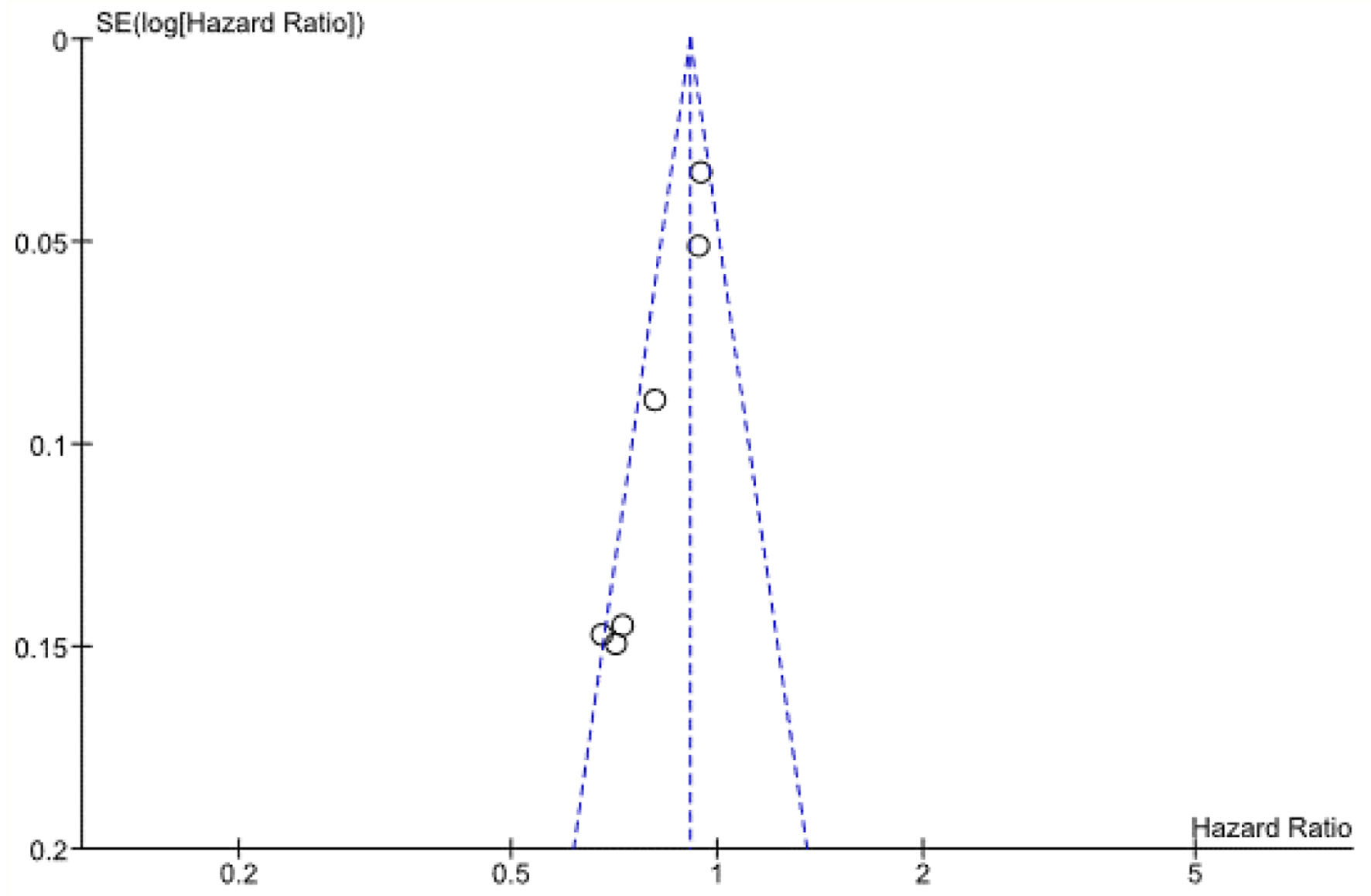 Click for large image | Figure 2. Funnel plot of comparison: 9 HR for extended MACE revised, outcome: 9.1 HR for extended MACE. HR: hazard ratio; MACE: major adverse cardiac event. |
Quantitative data analysis
Concerning the primary outcomes, the pooled hazard ratio (HR) for MACE was 0.72 (95% CI: 0.65 - 0.93), meaning that GLP-1 RA therapy was associated with significantly lower numbers of events. Heterogeneity among the studies was moderate (I2 = 68%) (Fig. 3). As far as the extended MACE is concerned, the pooled HR for extended MACE was 0.93 (95% CI: 0.89 - 0.98), meaning that GLP-1 RA therapy was associated with significantly lower numbers of events. Heterogeneity among the studies was low (I2 = 29%) (Fig. 4).
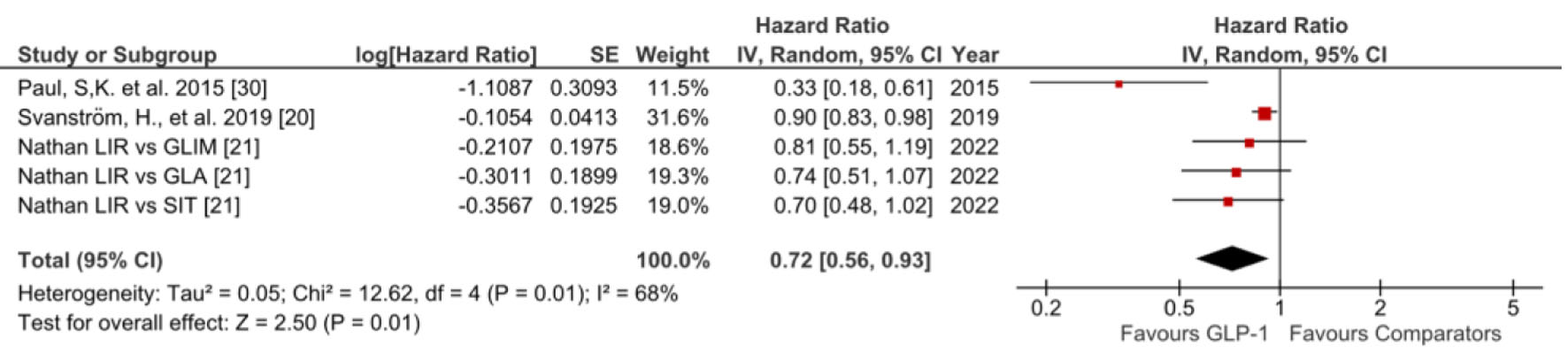 Click for large image | Figure 3. HR of MACE of GLP-1 RA versus comparators. GLA: glargine; GLIM: glimepiride; GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio; LIR: liraglutide; MACE: major adverse cardiac event; SIT: sitagliptin. |
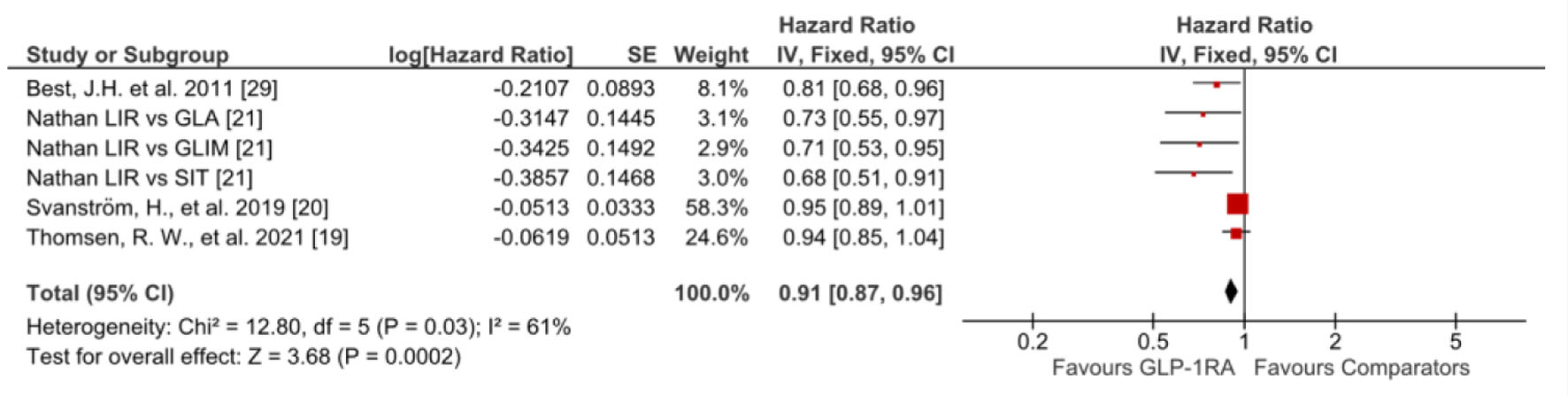 Click for large image | Figure 4. HR of extended MACE of GLP-1 RA versus comparators. GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio; MACE: major adverse cardiac event. |
The secondary outcomes were retrieved from a few studies. However, only one study reported all CV events between liraglutide and other comparators including glimepiride, sitagliptin, and glargine insulin [21]. Therefore, the three arms of the study were included in the meta-analysis. The pooled HR for all CV events was 0.71 (95% CI: 0.60 - 0.83), meaning that GLP-1 RA therapy was associated with significantly lower numbers of events. No heterogeneity was found among the arms of the study (I2 = 0%) (Fig. 5).
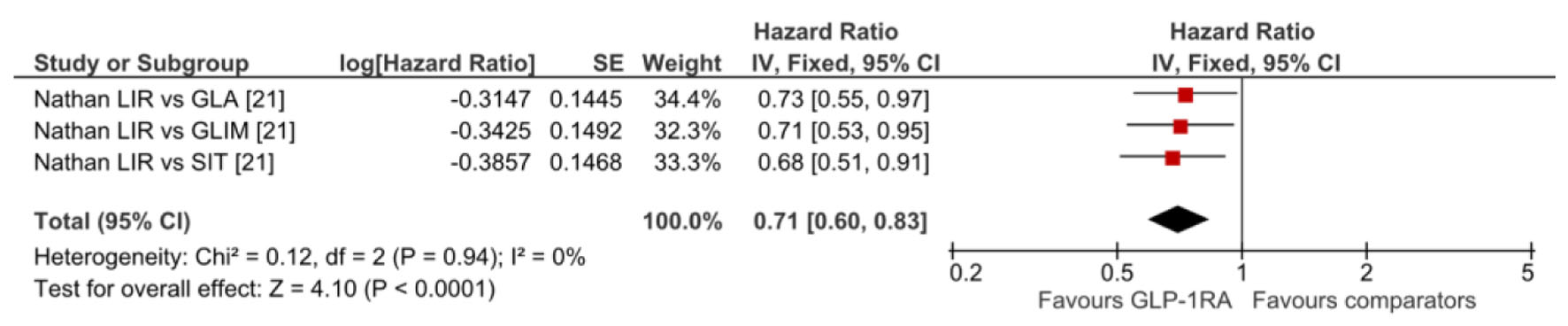 Click for large image | Figure 5. HR of all CV evets of GLP-1 RA versus comparators. CV: cardiovascular; GLA: glargine; GLIM: glimepiride; GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio; LIR: liraglutide; SIT: sitagliptin. |
For HF, the pooled analysis was calculated for hospitalization for and occurrence of HF subgroups. The pooled HR for hospitalization for HF (HHF) was 0.84 (95% CI: 0.77 - 0.91), meaning that GLP-1 RA therapy was associated with a significantly lower risk for HHF. Heterogeneity among the studies was moderate (I2 = 79%). In addition, the pooled HR for the occurrence of HF was 0.83 (95% CI: 0.75 - 0.94), meaning that GLP-1 RA therapy was associated with a significantly lower risk for the occurrence of HF. Heterogeneity among the studies was high (I2 = 95%). The pooled HR for both hospitalization and occurrence of HF subgroups was 0.84 (95% CI: 0.78 - 0.89). The heterogenicity between the studies of the subgroups was high (I2 = 86%) (Fig. 6).
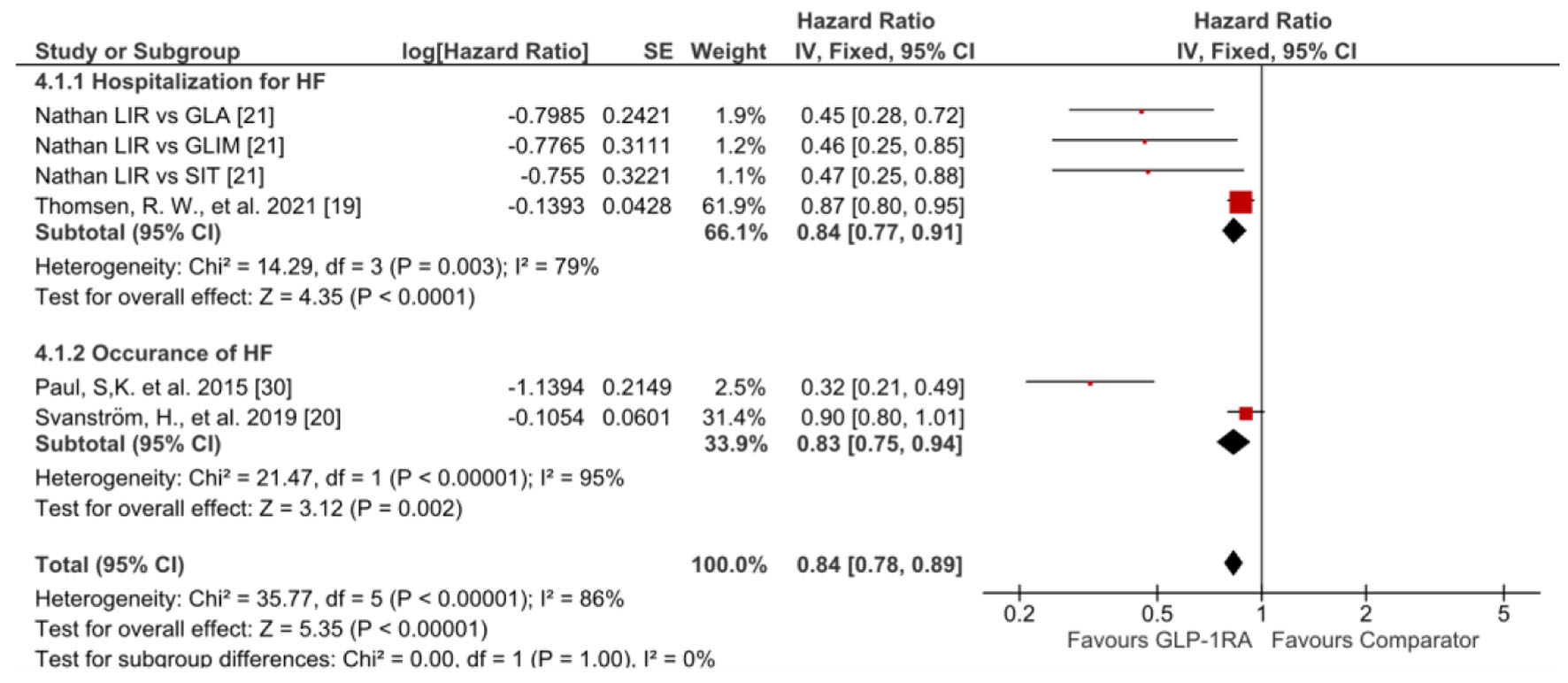 Click for large image | Figure 6. HR of HF of GLP-1 RA versus comparators including hospitalization for HF (upper half) and occurrence of HF (lower half). CV: cardiovascular; GLA: glargine; GLIM: glimepiride; GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio; LIR: liraglutide; SIT: sitagliptin. |
Given stroke, the pooled HR for the occurrence of stroke (fatal and non-fatal) was 0.86 (95% CI: 0.75 - 0.98), meaning that GLP-1 RA therapy was associated with a significantly lower risk for stroke compared to comparators. Heterogeneity among the studies was moderate (I2 = 81%) (Fig. 7).
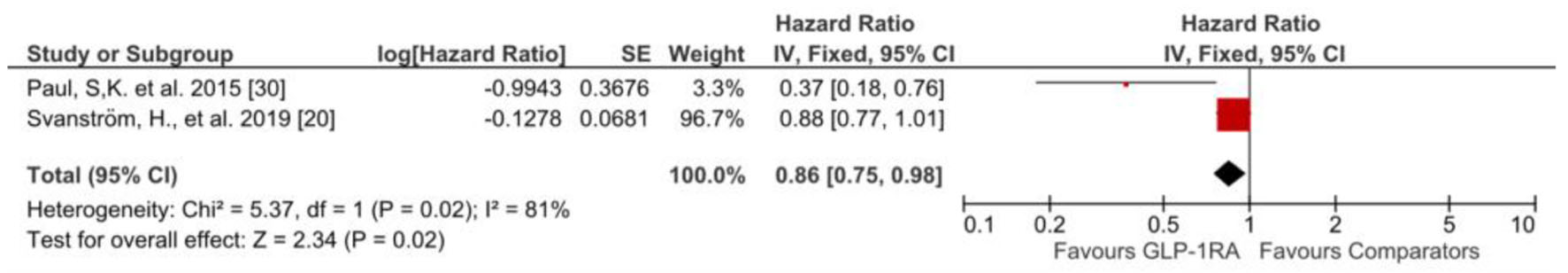 Click for large image | Figure 7. HR of stroke of GLP-1 RA versus comparators. GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio. |
As for MI, the pooled HR for the occurrence of MI (fatal and non-fatal) was 0.93 (95% CI: 0.83 - 1.04), meaning that GLP-1 RA therapy was associated with a non-significantly lower risk for MI compared to comparators. Heterogeneity among the studies was moderate (I2 = 78%) (Fig. 8).
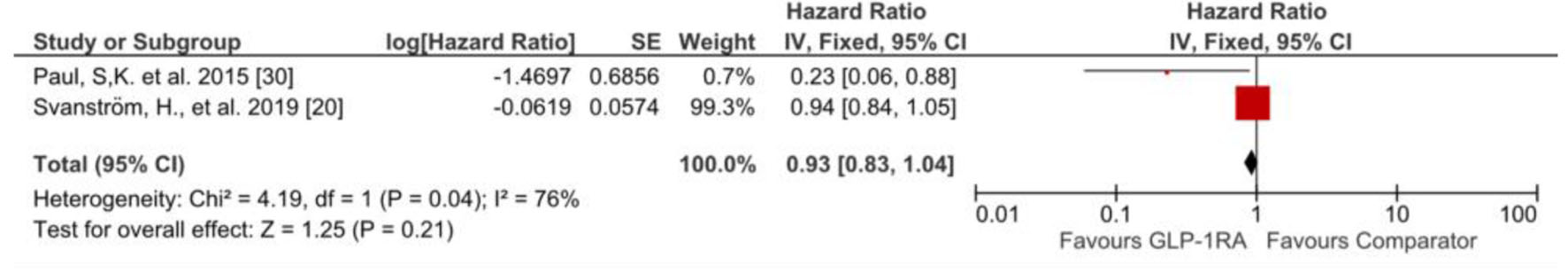 Click for large image | Figure 8. HR of myocardial infarction of GLP-1 RA versus comparators. GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio. |
As for all-cause mortality, the pooled HR for the occurrence of all-cause mortality was 0.82 (95% CI: 0.76 - 0.88), meaning that GLP-1 RA therapy was associated with significantly lower risk for all-cause mortality compared to comparators. No heterogeneity among the studies was found (I2 = 0%) (Fig. 9). Moreover, the pooled HR for the occurrence of CV death was 0.75 (95% CI: 0.65 - 0.85), meaning that GLP-1 RA therapy was associated with a significantly lower risk for CV death compared to comparators. Heterogeneity among the studies was low (I2 = 38%) (Fig. 10).
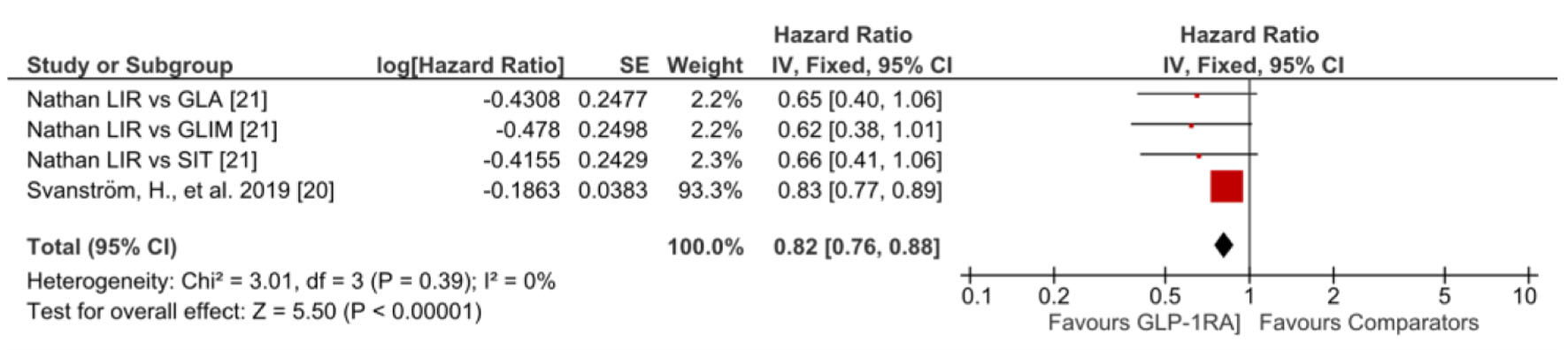 Click for large image | Figure 9. HR of all-cause mortality of GLP-1 RA versus comparators. GLA: glargine; GLIM: glimepiride; GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio; LIR: liraglutide; SIT: sitagliptin. |
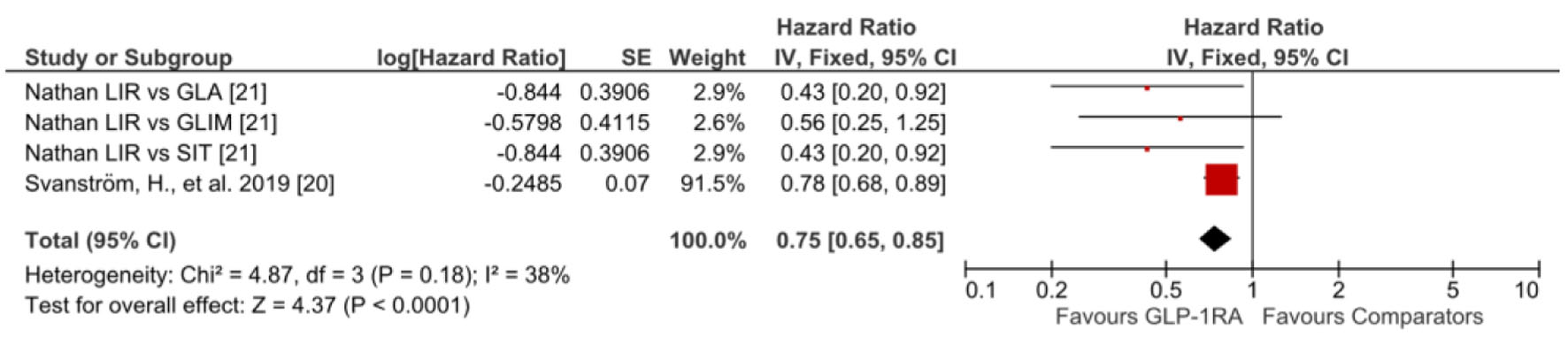 Click for large image | Figure 10. HR of CV death of GLP-1 RA versus comparators. CV: cardiovascular; GLA: glargine; GLIM: glimepiride; GLP-1 RA: glucagon-like peptide 1 receptor agonist; HR: hazard ratio; LIR: liraglutide; SIT: sitagliptin. |
| Discussion | ▴Top |
CVD represents the fundamental cause of morbidity and mortality among patients with T2DM in particular. The risk of CVD in T2DM patients is 2 - 4 times more likely than in those without diabetes [31]. Moreover, CV causes contribute to nearly half of the deaths attributed to diabetes in adult patients [32]. It was reported that adults with diabetes are subject to premature death related to the diabetes-associated CVD 15 years earlier than their healthy counterparts [33]. Furthermore, there is growing evidence in the literature that mortality in diabetic patients is substantially attributable to CV causes [34]. It was estimated that about 50% of all death diabetic patients can be attributed to CVD [35]. Additionally, the annualized death from CVD event rate in diabetic patients was 1.27/100 person-years compared to 0.51/100 person-years in nondiabetic subjects [36]. There is mounting evidence that CVD is mostly responsible for the health problems associated with diabetes including coronary heart disease, stroke, HF, and peripheral vascular disease as well as retinopathy, nephropathy, and neuropathy [31, 37]. Therefore, it is mandatory to focus on CVD in adult patients with diabetes that could have been already present even before the clinical diagnosis of diabetes [31]. Considering the detrimental impact of diabetes as a CV risk-determining factor, there is a growing interest in controlling CV events in diabetes patients in order to alleviate the physical, social, and economic burdens on patients and healthcare providers.
Consequently, the presence of an anti-diabetic drug that is safe and effective in controlling the glycemic state from one side and reducing the CV risk from the other would be a cutting edge in the management of T2DM. Among the novel anti-hyperglycemic agents, GLP-1 RA was observed to have a CV protective effect in several RCTs [38-40] and post hoc studies [38-40]. In addition, some observational studies that were carried out on diabetic patients without recent history, at least 1 year before enrollment in the study, of CV events showed promising results [19, 21].
The current study showed that GLP-1 RA was associated with a significantly low composite of CV events including MACE, extended MACE, and all CV events in observational studies that applied measures to control confounders. Concerning the individual CV risk factors, GLP-1 RA was found to be associated with a low risk of HF, HHF, and stroke. Although GLP-1 RA was found to be associated with a low risk of MI, the results were not significant. On the other hand, GLP-1 RA was found to be associated with a low risk of all-cause mortality and CV mortality with a statistically significant association. Additionally, the heterogeneity between the studies was null.
It is worth noting that the primary endpoint in the field of CV disease is a composite endpoint rather than the ideal single endpoint of the clinical trials. Composite endpoints have been focused on as a response to the FDA 2008 guidance to permit the conduction of CV outcome trials within a reasonable time frame [8]. The composite endpoints combine several clinical events that have common pathophysiological ground and similar beneficial outcomes. One advantage of using composite endpoints is that more events can be ascertained. Consequently, statistical power and precision are empowered [41]. Additionally, composite endpoints of mortality such as all-cause mortality and CV mortality are attractive endpoints because mortality can be determined without outcome ascertainment bias [42]. Therefore, both composite mortality endpoints are used in clinical trials to assure that any observed reduction in all-cause mortality would not be nullified by CV mortality [43]. Consequently, the current study focused on the most common primary composite endpoints namely MACE and extended MACE as well as all-cause mortality and CV mortality. In addition, individual outcomes such as stroke and MI have been included in the data analysis. Furthermore, HHF and the occurrence of HF have been analyzed separately because of the lack of justification to be included in the composite outcome [41].
For the composite endpoints, several studies reported the association between GLP-1 RA and the reduction of MACE and extended MACE. An earlier nested case-control study concluded that liraglutide, GLP-1 RA, was associated with composite endpoint reduction in diabetic patients [44]. In the LEADER study, liraglutide was associated with a low risk of composite endpoints compared to standard care therapy [45]. However, although lixisenatide, another GLP-1 RA member, was associated with a reduced risk of composite endpoints compared to the standard of care therapy in the ELIXA study, the result was statistically non-significant [46]. Both ELIXA and LEADER were designed basically as non-inferiority studies. Moreover, the diabetic patients enrolled in these studies were at a high risk of CVD. Therefore, the results of our study which included observational studies enrolling diabetic patients with no history of CV events long enough before the initiation of the study, provide evidence that GLP-1 RAs were associated with actual reduction in composite endpoints, MACE and extended MACE, thus stating the CV protective impact of GLP-1 RA.
Another composite endpoints analysis in this study included all-cause mortality and CV mortality. A recent systematic review study including 21 clinical trials found that GLP-1 RA was associated with a low risk of all-cause mortality and CV death [47]. Another systemic review including eight CV outcomes trials concurred that all-cause mortality and CV death are significantly reduced in diabetic patients who initiated GLP-1 RA therapy. Our study ascertained that GLP-1 RA has a powerful influence on reducing the risk of death in patients with T2DM.
Individual risk factors had been investigated as well. A systematic review and meta-analysis showed that GLP-1 RA reduced HHF significantly with no heterogenicity between the studies [3]. However, one observational study found that GLP-1 RA reduces the risk of HHF [30] and another study concluded the opposite [48]. This study confirmed the positive association of GLP-1 RA with the reduction of the risk of HHF. In addition, this study found that the occurrence of HF was reduced in adult patients with diabetes who received GLP-1 RA. Liraglutide was concluded to reduce the risk of non-fatal stroke and MI in diabetic patients with a marked reduction in renal function versus standards of care therapy as a placebo [49]. Another randomized study enrolling diabetic patients with and without CVD concluded that GLP-1 RA (exenatide) showed no significant difference to placebo group patients [50]. A deep insight into another randomized study showed that liraglutide, GLP-1 RA, was not significantly associated with a low risk of non-fatal MI or stroke [51]. However, these two randomized studies were designed as non-inferiority studies and were not focusing on the impact of GLP-1 RA on CV health. The findings of our study found that GLP-1 was associated with a significant reduction of stroke and MI. Therefore, this study assumed the protective influence of GLP-1 RA on CV health.
Strengths and limitations
One important aspect of this study is that participants who had no history of CV events for an adequate amount of time before the start of the observational studies were included. The observational studies that sought to directly evaluate the real influence of the innovative anti-hyperglycemic medicine on CV health were the primary focus of this systematic review, as opposed to the randomized non-inferiority trials. Because the comparison drugs were either standard or other novel anti-hyperglycemic medications, which may also have potential CV protective effects, the extent of GLP-1 RA’s cardioprotective effect cannot be overstated.
The main limitation of this study is the fewer numbers of the eligible studies included in this review. It is believed that the main reason for the paucity of the eligible criteria is that inclusion criteria were numerous and specific. Consequently, not all the studies had the relevant data that we were looking for. However, the information provided by these studies cannot be ignored. Moreover, the meta-analysis for HF included only two studies. Therefore, the studies highlighted the need for more research on this specific aspect.
Conclusion
GLP-1 RA is a novel class of glucose-lowering medications for T2DM. In addition to the effective antidiabetic impact, GLP-1 RA has CV protective potential. The summation of several observational studies provides supportive evidence for this assumption. Concerning the major adverse outcomes (MACE), GLP-1 RA is proven promising in reducing the risk of composite CV events. Additionally, GLP-1 RA can play an important role in extending life because they significantly reduce diabetes-associated mortality as well as CV-associated mortality. Therefore, GLP-1 RAs are promising class of antidiabetic medications. Further RCTs enrolling T2DM patients with no history of CVD are needed to establish the CV protective potentials of GLP-1 RA.
| Supplementary Material | ▴Top |
Suppl 1. Characteristics of the Eligible Studies.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Ali Rahman, Sura Alqaisi, Sunil E. Saith, and Rana Alzakhari contributed to study design, manuscript development, study selection, data collection, quality assessment, statistical analysis and figure and table design and development. Ralph Levy contributed to oversight and editing of final manuscript.
Data Availability
The authors declare that the data supporting the findings of this study are available within the article.
| References | ▴Top |
- Trujillo JM, Nuffer W, Ellis SL. GLP-1 receptor agonists: a review of head-to-head clinical studies. Ther Adv Endocrinol Metab. 2015;6(1):19-28.
doi pubmed pmc - Bonnet F. GLP-1 receptor agonist confer target organ protection in type 2 diabetes. Diabetes Metab. 2017;43(Suppl 1):2S1-2S2.
doi pubmed - Herrera Comoglio R, Vidal Guitart X. Cardiovascular outcomes, heart failure and mortality in type 2 diabetic patients treated with glucagon-like peptide 1 receptor agonists (GLP-1 RAs): A systematic review and meta-analysis of observational cohort studies. Int J Clin Pract. 2020;74(9):e13553.
doi pubmed - Nauck MA, Meier JJ, Cavender MA, Abd El Aziz M, Drucker DJ. Cardiovascular actions and clinical outcomes with glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors. Circulation. 2017;136(9):849-870.
doi pubmed - Trujillo JM, Nuffer W, Smith BA. GLP-1 receptor agonists: an updated review of head-to-head clinical studies. Ther Adv Endocrinol Metab. 2021;12:2042018821997320.
doi pubmed pmc - Bonora BM, Avogaro A, Fadini GP. Effects of exenatide long-acting release on cardiovascular events and mortality in patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Acta Diabetol. 2019;56(9):1051-1060.
doi pubmed - Arabi YM, Gordon AC, Derde LPG, Nichol AD, Murthy S, Beidh FA, Annane D, et al. Lopinavir-ritonavir and hydroxychloroquine for critically ill patients with COVID-19: REMAP-CAP randomized controlled trial. Intensive Care Med. 2021;47(8):867-886.
doi pubmed pmc - McGuire DK, Marx N, Johansen OE, Inzucchi SE, Rosenstock J, George JT. FDA guidance on antihyperglyacemic therapies for type 2 diabetes: One decade later. Diabetes Obes Metab. 2019;21(5):1073-1078.
doi pubmed - Hennekens CH, Hebert PR, Schneider WR, O'Brien P, Demets D, Borer JS. Academic perspectives on the United States Food and Drug Administration's guidance for industry on diabetes mellitus. Contemp Clin Trials. 2010;31(5):411-413.
doi pubmed - EMA: European Medicines Agency recommends suspension of Avandia, Avandamet and Avaglim. European Medicines Agency. 2018.
- Brown JM, Everett BM. Cardioprotective diabetes drugs: what cardiologists need to know. Cardiovasc Endocrinol Metab. 2019;8(4):96-105.
doi pubmed pmc - Cox EJ, Alicic RZ, Neumiller JJ, Tuttle KR. Clinical evidence and proposed mechanisms for cardiovascular and kidney benefits from glucagon-like peptide-1 receptor agonists. US Endocrinology. 2020.
- Sarnak MJ, Amann K, Bangalore S, Cavalcante JL, Charytan DM, Craig JC, Gill JS, et al. Chronic kidney disease and coronary artery disease: JACC State-of-the-Art review. J Am Coll Cardiol. 2019;74(14):1823-1838.
doi pubmed - Kristensen SL, Rorth R, Jhund PS, Docherty KF, Sattar N, Preiss D, Kober L, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019;7(10):776-785.
doi pubmed - Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, Lam CSP, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9(10):653-662.
doi pubmed - Leiter LA, Bain SC, Hramiak I, Jodar E, Madsbad S, Gondolf T, Hansen T, et al. Cardiovascular risk reduction with once-weekly semaglutide in subjects with type 2 diabetes: a post hoc analysis of gender, age, and baseline CV risk profile in the SUSTAIN 6 trial. Cardiovasc Diabetol. 2019;18(1):73.
doi pubmed pmc - Husain M, Consoli A, De Remigis A, Pettersson Meyer AS, Rasmussen S, Bain S. Semaglutide reduces cardiovascular events regardless of metformin use: a post hoc subgroup analysis of SUSTAIN 6 and PIONEER 6. Cardiovasc Diabetol. 2022;21(1):64.
doi pubmed pmc - Dagenais GR, Ryden L, Leiter LA, Lakshmanan M, Dyal L, Probstfield JL, Atisso CM, et al. Total cardiovascular or fatal events in people with type 2 diabetes and cardiovascular risk factors treated with dulaglutide in the REWIND trail: a post hoc analysis. Cardiovasc Diabetol. 2020;19(1):199.
doi pubmed pmc - Thomsen RW, Knudsen JS, Kahlert J, Baggesen LM, Lajer M, Holmgaard PH, Vedin O, et al. Cardiovascular Events, Acute Hospitalizations, and Mortality in Patients With Type 2 Diabetes Mellitus Who Initiate Empagliflozin Versus Liraglutide: A Comparative Effectiveness Study. J Am Heart Assoc. 2021;10(11):e019356.
doi pubmed pmc - Svanstrom H, Ueda P, Melbye M, Eliasson B, Svensson AM, Franzen S, Gudbjornsdottir S, et al. Use of liraglutide and risk of major cardiovascular events: a register-based cohort study in Denmark and Sweden. Lancet Diabetes Endocrinol. 2019;7(2):106-114.
doi pubmed - Grade Study Research Group, Nathan DM, Lachin JM, Bebu I, Burch HB, Buse JB, Cherrington AL, et al. Glycemia reduction in type 2 diabetes - microvascular and cardiovascular outcomes. N Engl J Med. 2022;387(12):1075-1088.
doi pubmed pmc - Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev. 2022;18(2):e1230.
doi pubmed pmc - Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
doi pubmed pmc - Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012.
doi pubmed - Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
doi pubmed pmc - Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
doi pubmed pmc - The Cochrane C. Review Manager (RevMan). 5.4 edition. 2020.
- Mirani M, Favacchio G, Serone E, Lucisano G, Rossi MC, Berra CC. Liraglutide and cardiovascular outcomes in a real world type 2 diabetes cohort. Pharmacol Res. 2018;137:270-279.
doi pubmed - Best JH, Hoogwerf BJ, Herman WH, Pelletier EM, Smith DB, Wenten M, Hussein MA. Risk of cardiovascular disease events in patients with type 2 diabetes prescribed the glucagon-like peptide 1 (GLP-1) receptor agonist exenatide twice daily or other glucose-lowering therapies: a retrospective analysis of the LifeLink database. Diabetes Care. 2011;34(1):90-95.
doi pubmed pmc - Paul SK, Klein K, Maggs D, Best JH. The association of the treatment with glucagon-like peptide-1 receptor agonist exenatide or insulin with cardiovascular outcomes in patients with type 2 diabetes: a retrospective observational study. Cardiovasc Diabetol. 2015;14:10.
doi pubmed pmc - Dal Canto E, Ceriello A, Ryden L, Ferrini M, Hansen TB, Schnell O, Standl E, et al. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26(2_suppl):25-32.
doi pubmed - van Dieren S, Beulens JW, van der Schouw YT, Grobbee DE, Neal B. The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil. 2010;17(Suppl 1):S3-S8.
doi pubmed - Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006;368(9529):29-36.
doi pubmed - Zhang Y, Niu J, Choi HK. Excess mortality among persons with type 2 diabetes. N Engl J Med. 2016;374(8):788.
doi pubmed - Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018;17(1):83.
doi pubmed pmc - Anand SS, Dagenais GR, Mohan V, Diaz R, Probstfield J, Freeman R, Shaw J, et al. Glucose levels are associated with cardiovascular disease and death in an international cohort of normal glycaemic and dysglycaemic men and women: the EpiDREAM cohort study. Eur J Prev Cardiol. 2012;19(4):755-764.
doi pubmed - Jia G, Hill MA, Sowers JR. Diabetic cardiomyopathy: an update of mechanisms contributing to this clinical entity. Circ Res. 2018;122(4):624-638.
doi pubmed pmc - Mosenzon O, Bain SC, Heerspink HJL, Idorn T, Mann JFE, Persson F, Pratley RE, et al. Cardiovascular and renal outcomes by baseline albuminuria status and renal function: Results from the LEADER randomized trial. Diabetes Obes Metab. 2020;22(11):2077-2088.
doi pubmed pmc - Branch KRH, Dagenais GR, Avezum A, Basile J, Conget I, Cushman WC, Jansky P, et al. Dulaglutide and cardiovascular and heart failure outcomes in patients with and without heart failure: a post-hoc analysis from the REWIND randomized trial. Eur J Heart Fail. 2022;24(10):1805-1812.
doi pubmed - Paiman EHM, van Eyk HJ, van Aalst MMA, Bizino MB, van der Geest RJ, Westenberg JJM, Geelhoed-Duijvestijn PH, et al. Effect of liraglutide on cardiovascular function and myocardial tissue characteristics in type 2 diabetes patients of South Asian descent living in the netherlands: a double-blind, randomized, placebo-controlled trial. J Magn Reson Imaging. 2020;51(6):1679-1688.
doi pubmed pmc - Marx N, McGuire DK, Perkovic V, Woerle HJ, Broedl UC, von Eynatten M, George JT, et al. Composite primary end points in cardiovascular outcomes trials involving type 2 diabetes patients: should unstable angina be included in the primary end point? Diabetes Care. 2017;40(9):1144-1151.
doi pubmed - Lubsen J, Kirwan BA. Combined endpoints: can we use them? Stat Med. 2002;21(19):2959-2970.
doi pubmed - Mao L, Kim K. Statistical models for composite endpoints of death and non-fatal events: a review. Stat Biopharm Res. 2021;13(3):260-269.
doi pubmed pmc - Gejl M, Starup-Linde J, Scheel-Thomsen J, Gregersen S, Vestergaard P. Risk of cardiovascular disease: the effects of diabetes and anti-diabetic drugs - a nested case-control study. Int J Cardiol. 2015;178:292-296.
doi pubmed - Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, Nissen SE, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311-322.
doi pubmed pmc - Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Kober LV, Lawson FC, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247-2257.
doi pubmed - Lin DS, Lee JK, Hung CS, Chen WJ. The efficacy and safety of novel classes of glucose-lowering drugs for cardiovascular outcomes: a network meta-analysis of randomised clinical trials. Diabetologia. 2021;64(12):2676-2686.
doi pubmed - Patorno E, Goldfine AB, Schneeweiss S, Everett BM, Glynn RJ, Liu J, Kim SC. Cardiovascular outcomes associated with canagliflozin versus other non-gliflozin antidiabetic drugs: population based cohort study. BMJ. 2018;360:k119.
doi pubmed pmc - Mann JFE, Fonseca V, Mosenzon O, Raz I, Goldman B, Idorn T, von Scholten BJ, et al. Effects of liraglutide versus placebo on cardiovascular events in patients with type 2 diabetes mellitus and chronic kidney disease. Circulation. 2018;138(25):2908-2918.
doi pubmed pmc - Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, Buse JB, Chan JC, et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(13):1228-1239.
doi pubmed pmc - Husain M, Birkenfeld AL, Donsmark M, Dungan K, Eliaschewitz FG, Franco DR, Jeppesen OK, et al. Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2019;381(9):841-851.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


