| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website http://www.cardiologyres.org |
Case Report
Volume 9, Number 6, December 2018, pages 381-384
Pericarditis After Breast Implant Rupture: A Case Report
Clemence Bretaudeaua, e, Charlotte Vaysseb, c, Paul Guerbya, Olivier Lairezc, d, Marc Soule-Tholyb, Fabien Vidala, b, c, Elodie Chantalatb, c
aDepartment of Gynaecology Surgery, CHU Paule de Viguier, Toulouse, France
bDepartment of Gynaecology Surgery, CHU Rangueil, Toulouse, France
cUniversite Paul Sabatier, Toulouse, 118 route de Narbonne, 31062 Toulouse, France
dDepartement of Cardiology, CHU Rangueil, Toulouse, France
eCorresponding Author: Clemence Bretaudeau, Department of Gynaecology Surgery, CHU Paule de Viguier, Toulouse, 330 avenue de Grande-Bretagne, TSA 70034, 31059 Toulouse, France
Manuscript submitted July 5, 2018, accepted September 20, 2018
Short title: Pericarditis After Breast Implant Rupture
doi: https://doi.org/10.14740/cr756w
| Abstract | ▴Top |
A ruptured breast implant is usually asymptomatic and accidentally discovered during an imaging test. However, implant ruptures can cause isolated silicone granulomas and cases of severe systemic disease. We report the first case of a 39-year-old female patient with augmentation breast implants and myopericarditis secondary to implant rupture. Many etiologies of myopericarditis were explored, but none were selected with the exception of the rupture of the implant in the left breast. Magnetic resonance imaging showed a prosthetic rupture with capsular intrusion and formation of a silicone granuloma with inflammation of the pericardium on contact. Clinical and radiological improvement was observed in the short term after surgical removal of the implant. A review of the literature was conducted supporting the hypothesis of an autoimmune and inflammatory syndrome induced by an adjuvant.
Keywords: Autoimmune/inflammatory syndrome; Breast implant rupture; Myopericarditis; Silicone granuloma
| Introduction | ▴Top |
A ruptured breast implant is usually asymptomatic and discovered by chance during an imaging exam. Implant ruptures can cause silicone granulomas (inflammatory reactions to silicone) that are often isolated, but cases of serious systemic disease, even anaplastic large-cell lymphoma, have been described in the literature [1, 2]. We report on the case of a 39-year-old female patient with breast augmentation implants for aesthetic reasons, who presented with myopericarditis secondary to rupture of an implant in her left breast.
| Case Report | ▴Top |
A 39-year-old female patient with no significant medical or surgical history other than implants for breast augmentation [3] was referred for a gynaecological consultation for advice concerning a ruptured implant in the left breast, which was discovered by chance in the context of myopericarditis with no known aetiology. She had been treated for several months by cardiology and internal medicine teams for chest pain with exertional dyspnoea, chest tightness, vertigo and a decline in her general health condition, dominated by asthenia.
The cardiac symptomatology was marked by left chest pain, increased during changes of position and especially when inclining the trunk forward. The pain was accompanied by dyspnoea and asthenia at the least effort, of increasing evolution.
An electrocardiogram (ECG) showed negative T waves on the precordial leads V1 - V3 and ventricular extrasystoles with compensatory pause. An chest X-ray showed no particular abnormality (Fig. 1).
 Click for large image | Figure 1. Chest X-ray showing no abnormalities but an asymmetry between the right and left breast. |
The serological and immunological profiles were normal other than unspecified positive type-B antinuclear antibodies (ANA), a positive Strongyloidiasis serology, and a positive Chlamydia pneumoniae serology (presence of anti-G immunoglobulins (IgG)). Intradermal allergy testing was within normal limits at 5 mm (faint evidence of vaccination at birth). Troponin was negative. A chest, abdominal and pelvic CT scan (CAP CT) with contrast injection showed an isolated thin layer of pericardial effusion measuring 10 mm at the long axis, confirmed by a transthoracic echocardiogram (TTE) with normal cardiac function and left ventricular ejection fraction (LVEF) of 60%. The pericardial effusion was non-compressive and non-circumferential, measured a maximum of 1 cm over the right ventricle with no other abnormalities (Fig. 2). The diagnosis of myopericarditis was confirmed by cardiac magnetic resonance imaging (MRI).
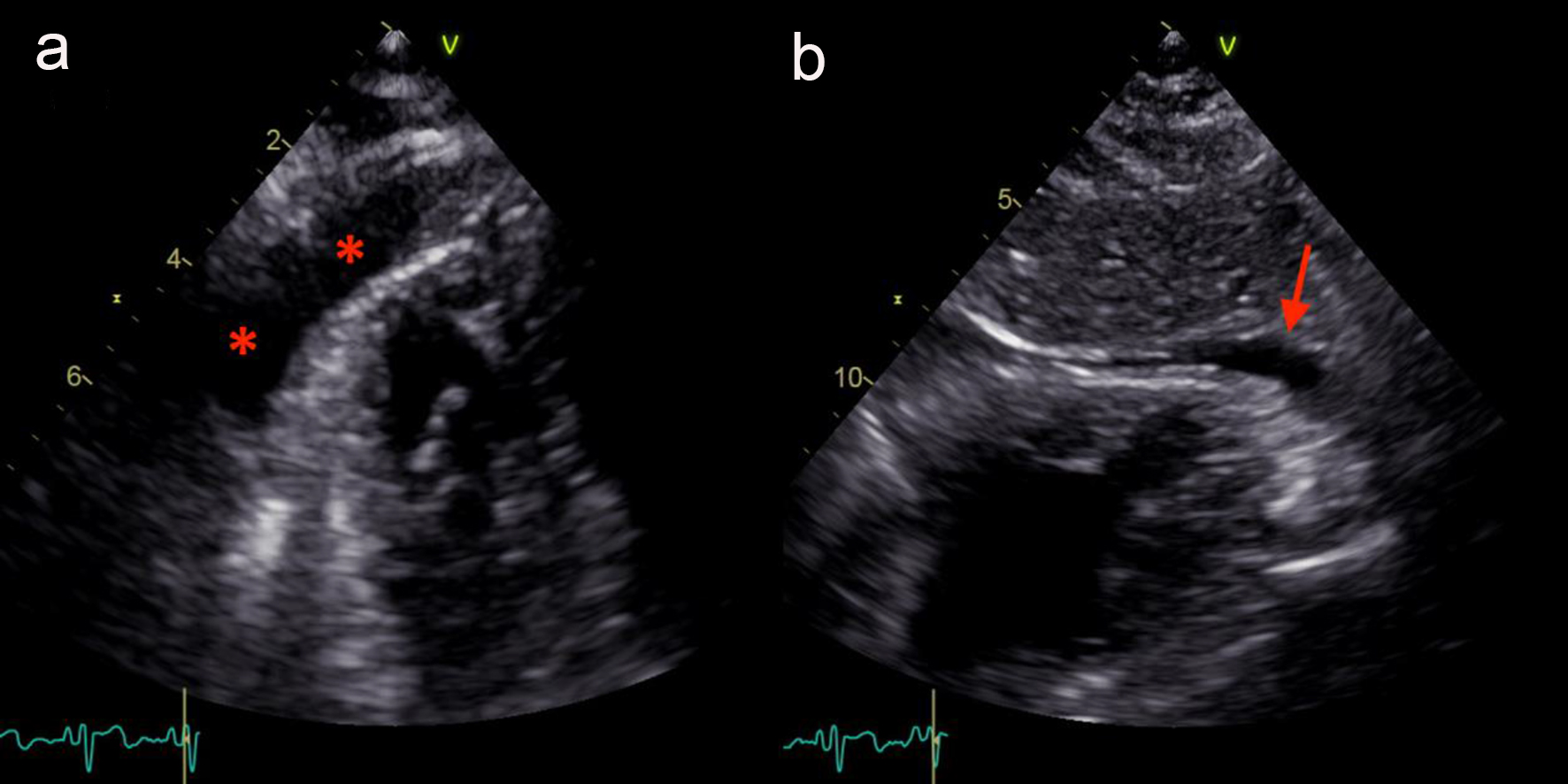 Click for large image | Figure 2. Echocardiography showing an apical pericardial effusion in apical four-chamber view (a, red stars) and subcostal view (b, red arrow). |
As no aetiology was found, the patient was treated empirically and successively with antibiotics, then aspirin and colchicine. No clinical or radiological improvement was obtained. A radiological breast assessment was initiated, which showed a suspected breast implant rupture on the ultrasound, which initially appeared to be intracapsular, in the left breast. The clinical breast exam was normal, with no obvious signs of implant rupture. The breast MRI showed intracapsular implant rupture in the lower outer quadrant with periprosthetic effusion, silicone granuloma and mirroring inflammatory changes on the proximal pericardium (Fig. 3).
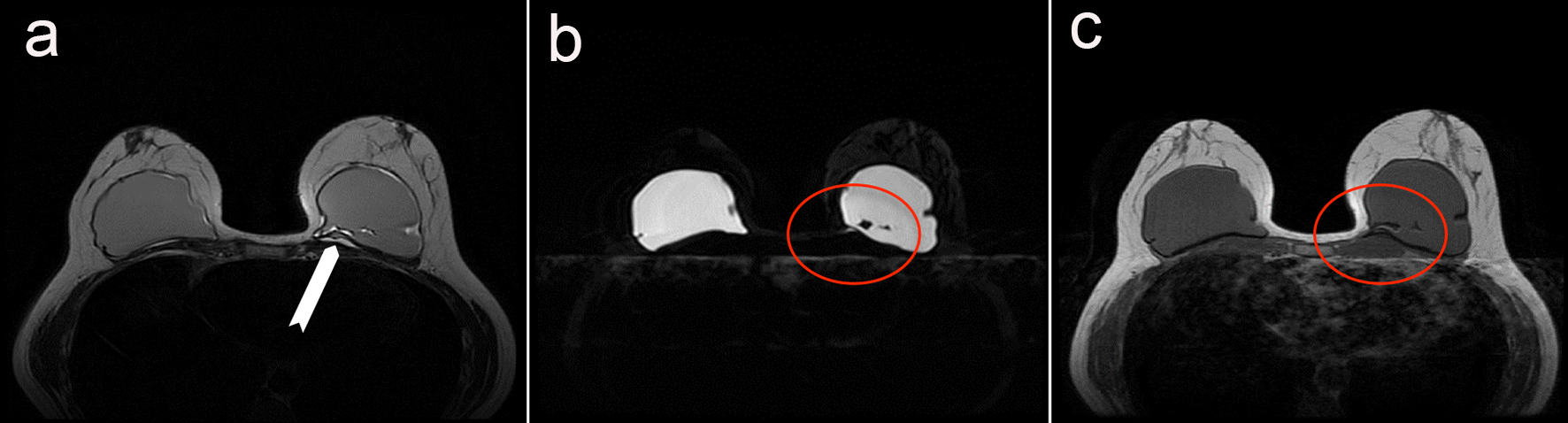 Click for large image | Figure 3. MRI showing the rupture of the implant in the left breast. (a) T2 propeller 3-0 sequence allowing minimizing the motion artifacts and showing a silicone granuloma. (b) Axial sequence T2 short T1 inversion recovery allowing the suppression of the fat signal. (c) Axial sequence T1. b and c show an effusion inside the silicone of the implant, indicating the rupture of both the implant and the periprosthetic capsule. |
Surgical removal of the breast implant was therefore recommended. Intraoperative observations confirmed the complete rupture of the implant with an extracapsular silicone granuloma not detected on the MRI. In addition to the implant removal, the silicone granuloma was completely excised and a total capsulectomy was performed. The anatomic pathology analysis of the specimen from the capsulectomy showed a simple periprosthetic shell of fibrous and inflammatory tissue, with no signs of malignancy.
In the immediate postoperative period, there was a marked improvement in her overall health with decreased asthenia. The cardiac symptoms persisted for several weeks after surgery, but were less severe. A TTE performed 1 month after the excision surgery showed resolution of the pericardial effusion. At 3 months, the patient continued to make good progress and was asymptomatic with no significant pericardial effusion.
| Discussion | ▴Top |
We report here on the first case of myopericarditis secondary to a ruptured breast implant in the left breast. In nearly 8 out of 10 cases of pericarditis, no specific aetiology could be identified [4]. Infectious causes are distinct from non-infectious causes.
Infectious causes encompassed viral infections (Coxsackie A virus, adenovirus, echovirus), bacterial infections (mycobacteria such as tuberculosis, septicaemia) and fungal infections (Candida, Aspergillus). In our cases, infectious causes were ruled out by bacteriological, virological and mycotic testing.
Non-infectious causes encompassed etiologies of cardiac origin (myocardial infarction with transmural necrosis or Dressler syndrome), paraneoplastic syndromes and systemic autoimmune diseases (disseminated lupus erythematosa, sarcoidosis and rheumatoid arthritis). In our patient, the cardiac assessment ruled out a myocardial infarction. CAP CT, radiological breast assessment and colonoscopy ruled out a paraneoplastic aetiology. Inflammatory and auto-immune assessments ruled out systemic autoimmune diseases.
Before confirming the diagnosis of benign idiopathic acute pericarditis, the hypothesis of a ruptured implant in the left breast was suggested. In fact, positive type-B ANAs have been observed in autoimmune/inflammatory syndrome induced by adjuvants (ASIA) in patients with ruptured silicone breast implants. Yehuda Shoenfeld [5] proposes the following criteria for diagnosing ASIA: exposure to an external stimulus (silicone, infection, vaccine and adjuvant) before the onset of “typical” clinical manifestations (muscle pain, muscle weakness, joint pain and/or arthritis, chronic asthenia, neurological manifestations, cognitive disorders and fever). The patient’s clinical improvement after the causal agent was removed is a strong argument in favour of this diagnosis. Numerous studies mention the production of more or less specific antibodies in patients with ruptured breast implants (or not) [6, 7], but also the onset of connective tissue diseases [8], especially scleroderma [9].
Some authors even talk of a “silicone implant incompatibility syndrome” [10]. In our case, the clinical and laboratory assessments performed on this patient showed no evidence suggestive of connective tissue diseases; however, the symptoms could correspond to this “silicone implant incompatibility syndrome”. These data are challenged by other studies that did not show a significant relationship between breast implants and connective tissue disease [11].
The spread of gel beyond the capsule in extracapsular ruptures leads to a risk of silicone granuloma [12] and of contact inflammatory reaction. In our case, the implant rupture was extracapsular and on the left side. This leads us to suggest potential inflammation of the pericardium and myocardium by contiguity.
Cases of silicone granuloma away from the site of the breast implant rupture suggest that the silicone is probably disseminated through the bloodstream and/or lymphatic system [13]. Some cases of silicone granulomas have been demonstrated very far from the initial diffusion site, for example, in the lower limbs [14]. They may be associated with systemic manifestations [15].
Given the resolution of the symptoms and the ultrasonographical signs of pericarditis in our patient after explantation, we concluded that her symptoms were due to rupture of her breast implant because of the formation of a thoracic silicone granuloma with myocardial contact inflammation and partly to ASIA.
Although current data point to many systemic and local complications related to silicone breast implants, they do not establish a significant enough relationship to warrant prohibiting the use of these implants, the aesthetic qualities of which are irrefutable.
Conflict of Interests
The authors declare having no conflicts of interests.
| References | ▴Top |
- Silverman BG, Brown SL, Bright RA, Kaczmarek RG, Arrowsmith-Lowe JB, Kessler DA. Reported complications of silicone gel breast implants: an epidemiologic review. Ann Intern Med. 1996;124(8):744-756.
doi pubmed - Doren EL, Miranda RN, Selber JC, Garvey PB, Liu J, Medeiros LJ, Butler CE, et al. U.S. epidemiology of breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2017;139(5):1042-1050.
doi pubmed - Khan AW, Craig M, Jarmulowicz M, Davidson BR. Liver tumours due to endometriosis and endometrial stromal sarcoma. HPB (Oxford). 2002;4(1):43-45.
doi pubmed - Zayas R, Anguita M, Torres F, Gimenez D, Bergillos F, Ruiz M, Ciudad M, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75(5):378-382.
doi - Shoenfeld Y, Agmon-Levin N. 'ASIA' - autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36(1):4-8.
doi pubmed - Cuellar ML, Scopelitis E, Tenenbaum SA, Garry RF, Silveira LH, Cabrera G, Espinoza LR. Serum antinuclear antibodies in women with silicone breast implants. J Rheumatol. 1995;22(2):236-240.
pubmed - Bar-Meir E, Teuber SS, Lin HC, Alosacie I, Goddard G, Terybery J, Barka N, et al. Multiple autoantibodies in patients with silicone breast implants. J Autoimmun. 1995;8(2):267-277.
doi pubmed - Bassetto F, Scarpa C, Vindigni V, Doria A. The periprosthetic capsule and connective tissue diseases: a piece in the puzzle of autoimmune/autoinflammatory syndrome induced by adjuvants. Exp Biol Med (Maywood). 2012;237(10):1117-1122.
doi pubmed - Motegi S, Hattori T, Tago O, Shimizu A, Ishikawa O. Systemic sclerosis associated with silicone breast implantation. Eur J Dermatol. 2013;23(6):894-895.
pubmed - Kappel RM, Cohen Tervaert JW, Pruijn GJ. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) due to silicone implant incompatibility syndrome in three sisters. Clin Exp Rheumatol. 2014;32(2):256-258.
pubmed - Janowsky EC, Kupper LL, Hulka BS. Meta-analyses of the relation between silicone breast implants and the risk of connective-tissue diseases. N Engl J Med. 2000;342(11):781-790.
doi pubmed - Gorczyca DP, DeBruhl ND, Ahn CY, Hoyt A, Sayre JW, Nudell P, McCombs M, et al. Silicone breast implant ruptures in an animal model: comparison of mammography, MR imaging, US, and CT. Radiology. 1994;190(1):227-232.
doi pubmed - Dragu A, Theegarten D, Bach AD, Polykandriotis E, Arkudas A, Kneser U, Horch RE, et al. Intrapulmonary and cutaneous siliconomas after silent silicone breast implant failure. Breast J. 2009;15(5):496-499.
doi pubmed - Oh JH, Song SY, Lew DH, Lee DW. Distant migration of multiple siliconomas in lower extremities following breast implant rupture: case report. Plast Reconstr Surg Glob Open. 2016;4(10):e1011.
doi pubmed - Nesher G, Soriano A, Shlomai G, Iadgarov Y, Shulimzon TR, Borella E, Dicker D, et al. Severe ASIA syndrome associated with lymph node, thoracic, and pulmonary silicone infiltration following breast implant rupture: experience with four cases. Lupus. 2015;24(4-5):463-468.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.


